Familial Mediterranean Fever Symptoms: Familial Mediterranean Fever (FMF) is a hereditary inflammatory disorder that primarily affects people of Mediterranean and Middle Eastern descent, including those of Armenian, Arab, Turkish, and Jewish ancestry.
It is characterized by recurrent episodes of fever, abdominal pain, chest pain, and arthritis. Understanding the symptoms and causes of FMF is crucial for early diagnosis and effective management of the condition.
What is Familial Mediterranean Fever?
Familial Mediterranean Fever (FMF) is a hereditary inflammatory disorder that predominantly affects individuals of Mediterranean ancestry, including those from Sephardic Jewish, Armenian, Arab, and Turkish backgrounds. This genetic condition is characterized by recurrent episodes of fever and painful inflammation in the abdomen, chest, or joints. The episodes or attacks can vary in frequency and intensity and are often accompanied by skin rashes or swelling. FMF is caused by mutations in the MEFV gene, which plays a crucial role in the body’s inflammatory response. Despite its potential severity, with timely diagnosis and proper treatment, individuals with FMF can lead full and active lives.
Statistics on Prevalence and Populations Most Affected
Familial Mediterranean Fever is most prevalent among populations with Mediterranean lineage, with the highest incidence rates observed in Armenians, Sephardic Jews, Arabs, and Turks. The disorder affects approximately 1 in 200 to 1 in 1,000 individuals within these communities. However, due to increasing global migration and intermarriage, FMF cases are now being identified in a wider range of ethnic groups and geographical locations.
Among the affected populations, the carrier frequency of MEFV gene mutations can be as high as 1 in 5, which significantly contributes to the disease’s prevalence within these communities. Despite its genetic nature, the expression of FMF and the severity of its symptoms can vary widely among individuals, even those within the same family. This variation underscores the importance of genetic counseling and personalized medical management for those at risk or diagnosed with Familial Mediterranean Fever.
The condition’s impact extends beyond the individual, affecting families and communities due to its hereditary nature. Awareness and understanding of FMF are crucial for early diagnosis and effective treatment, helping to reduce the burden of the disease on affected populations. Advances in genetic testing and targeted therapies offer hope for improved management and quality of life for those living with Familial Mediterranean Fever.
Causes of Familial Mediterranean Fever
Understanding the causes and triggers of FMF can help in managing the condition more effectively. This article delves into the genetic underpinnings of FMF, its inheritance patterns, and various environmental and lifestyle factors that may exacerbate or trigger symptoms.
Genetic Mutations Responsible for FMF
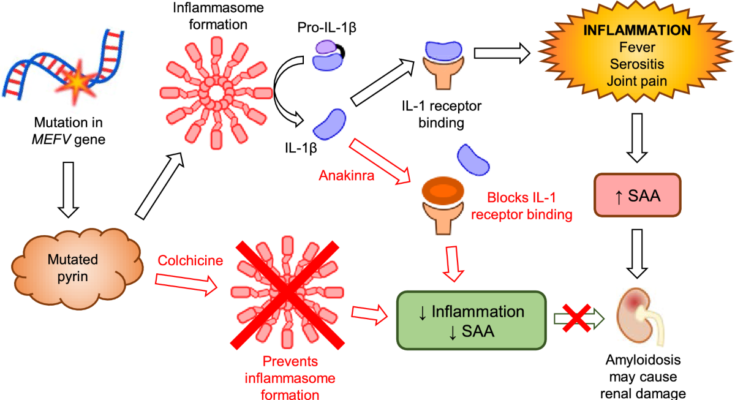
The primary cause of Familial Mediterranean Fever is mutations in the MEFV gene. This gene plays a crucial role in the body’s immune response, helping to regulate inflammation. Mutations in the MEFV gene disrupt its normal function, leading to uncontrolled inflammation, which is characteristic of FMF. These genetic changes are directly linked to the condition’s hallmark symptoms, such as fever, abdominal pain, chest pain, and joint pain.
How FMF is Inherited
FMF is inherited in an autosomal recessive pattern. This means that to develop the disorder, an individual must receive a mutated copy of the gene from both parents. If a person inherits only one mutated gene, they are considered a carrier and may not show symptoms. Carriers have a 50% chance of passing the mutated gene to their offspring. When two carriers have a child, there is a 25% chance the child will inherit FMF, a 50% chance the child will be a carrier, and a 25% chance the child will inherit normal genes from both parents.
Environmental and Lifestyle Factors That Might Trigger Symptoms
While FMF is a genetic condition, certain environmental and lifestyle factors can trigger symptoms or worsen them. These include:
- Stress: Both physical and emotional stress have been noted to precipitate FMF attacks. Managing stress through relaxation techniques and stress management strategies can help mitigate these effects.
- Diet: Some individuals with FMF report that certain foods can trigger their symptoms. While there’s no specific diet for FMF, maintaining a balanced diet and avoiding foods that seem to trigger symptoms may be beneficial.
- Infections: Infections can provoke inflammatory responses in the body, potentially triggering FMF attacks. Regular handwashing, staying up-to-date with vaccinations, and other preventive measures can help reduce this risk.
- Physical Fatigue: Overexertion and physical fatigue might trigger FMF symptoms. It’s important for individuals with FMF to balance activity with rest and not push beyond their limits.
However, understanding these triggers and how FMF is inherited allows individuals and families to better navigate the challenges of the condition. With advancements in genetic testing and personalized medicine, managing FMF has become more effective, improving the quality of life for those affected.
Common Symptoms of Familial Mediterranean Fever
Understanding the symptoms of FMF is crucial for early diagnosis and effective management. This comprehensive list of symptoms, their manifestation, and potential impact on patients’ lives aims to provide valuable insights for those affected by FMF and their caregivers.
Key Symptoms of FMF
- Fever: Sudden spikes in temperature are a hallmark of FMF. These fever episodes typically last from a few hours to three days and are often accompanied by other symptoms listed below.
- Abdominal Pain: Severe pain in the abdomen, mimicking appendicitis, is common. This can be distressing and may lead to unnecessary surgical intervention if not correctly diagnosed.
- Chest Pain: Episodes can include sharp, stabbing chest pain that intensifies with deep breaths or coughs, often mistaken for pleurisy or other pulmonary conditions.
- Joint Pain: Arthritis, especially in the ankles, knees, and hips, occurs during flare-ups. Swelling and severe pain can limit mobility and affect daily activities.
- Skin Rash: A red, raised rash, typically on the lower legs, may appear during episodes. This symptom, though less common, can be uncomfortable and impact a patient’s self-esteem.
- Muscle Aches: Diffuse muscle pain during episodes adds to the discomfort experienced by patients.
Episodic Nature and Impact on Life
The symptoms of FMF are episodic, meaning they come and go, with patients often experiencing periods of good health in between attacks. However, the unpredictability of these episodes can significantly impact the quality of life, causing anxiety and uncertainty. Patients may find it challenging to plan activities or commit to obligations for fear of an impending episode. Moreover, the symptoms can be debilitating, affecting academic, professional, and social engagements.
Long-term complications of untreated or inadequately managed FMF include protein buildup in organs (amyloidosis), leading to kidney failure and other serious health issues. Hence, recognizing these symptoms early and seeking appropriate medical advice is vital.
However, Familial Mediterranean Fever is a condition with a profound impact on patients’ lives due to its episodic nature and the severe symptoms experienced during flare-ups. Early diagnosis and management are key to improving the quality of life for those affected by FMF. Understanding and recognizing the symptoms are the first steps toward achieving this goal.
Diagnosing Familial Mediterranean Fever (FMF)
Early and accurate diagnosis is crucial for managing symptoms and preventing complications. Below, we delve into the diagnostic criteria, medical tests, and the pivotal role of genetic testing in diagnosing FMF.
List of Diagnostic Criteria for FMF
The diagnosis of Familial Mediterranean Fever relies on a combination of clinical criteria and genetic testing. The key clinical criteria include:
- Recurrent Fever: Sporadic episodes of fever without any external infection.
- Abdominal Pain: Acute inflammation causing severe abdominal pain, resembling appendicitis.
- Chest Pain: Inflammation of the lining around the lungs, causing sharp chest pain, especially when breathing.
- Joint Pain: Arthritis or arthralgia, typically affecting the ankles, knees, or hips.
- Erysipelas-like Erythema: Red, painful skin rashes, usually on the legs.
- Family History: A family history of FMF or unexplained episodes of fever and inflammation.
These criteria help guide clinicians in suspecting FMF but are not definitive without further diagnostic testing.
Medical Tests and Procedures Used to Diagnose FMF
While there’s no single test for FMF, a combination of procedures and tests are used to rule out other conditions and confirm the diagnosis:
- Complete Blood Count (CBC): To check for signs of infection or inflammation through elevated white blood cell count.
- Acute Phase Reactants: Tests for elevated levels of C-reactive protein (CRP) and serum amyloid A (SAA) that indicate inflammation.
- Abdominal Ultrasound: To visualize abdominal inflammation and exclude other causes of abdominal pain.
- Echocardiography: Used occasionally to assess for inflammation of the heart covering, known as pericarditis.
The Role of Genetic Testing in FMF Diagnosis
Genetic testing plays a critical role in the diagnosis of FMF. The condition is caused by mutations in the MEFV gene, which encodes a protein called pyrin. Pyrin plays a key role in regulating inflammation in the body. Genetic testing can identify mutations in the MEFV gene, providing a definitive diagnosis of FMF. It’s particularly useful in cases where clinical symptoms are unclear or to confirm a suspected diagnosis based on clinical criteria.
- Confirmation of Diagnosis: A positive genetic test for mutations in the MEFV gene confirms the diagnosis of FMF.
- Family Screening: Genetic testing can also be used to screen family members of an affected individual, even if they are asymptomatic.
- Tailoring Treatment: Understanding the specific genetic mutations can help tailor treatment plans, particularly in determining the necessity and dosage of colchicine, the primary treatment for FMF.
However, diagnosing Familial Mediterranean Fever involves a thorough evaluation of clinical symptoms, supported by specific medical tests and procedures. Genetic testing is paramount in confirming the diagnosis, screening family members, and guiding the management of the disease. Early diagnosis and appropriate treatment can significantly improve the quality of life for individuals with FMF, preventing complications and controlling symptoms.
Complications Associated with Familial Mediterranean Fever (FMF)
Understanding these complications and the importance of vigilant monitoring and management is crucial for patients and healthcare providers alike.
Risk of Developing Amyloidosis and Its Implications
One of the most significant complications associated with FMF is the risk of developing amyloidosis. Amyloidosis occurs when a protein called amyloid accumulates in organs and tissues, impairing their normal function. In the context of FMF, the type of amyloidosis most commonly observed is AA amyloidosis, which primarily affects the kidneys, leading to kidney failure if not addressed promptly. The buildup of amyloid proteins can also impact other organs, including the heart, spleen, and gastrointestinal system, potentially leading to a wide range of health issues. Early detection and treatment of FMF are critical to reducing the risk of amyloidosis and its severe consequences.
Other Potential Complications
In addition to amyloidosis, FMF can lead to several other complications, particularly if the condition is poorly controlled or undiagnosed. Kidney problems are among the most serious, with amyloidosis being a leading cause of renal failure in FMF patients. However, even in the absence of amyloidosis, FMF can contribute to impaired kidney function over time.
Other potential complications include:
- Inflammatory complications: FMF can cause chronic inflammation in various parts of the body, leading to complications such as arthritis, skin rashes, and inflammatory bowel disease.
- Increased risk of infections: Episodes of fever and inflammation can weaken the body’s immune response, making it more susceptible to infections.
- Heart problems: Though less common, chronic inflammation associated with FMF can affect the heart, leading to conditions such as pericarditis (inflammation of the heart’s outer layer) and, in rare cases, myocarditis (inflammation of the heart muscle).
Importance of Monitoring and Managing Symptoms
Given the potential severity of these complications, it’s imperative for individuals with FMF to closely monitor their symptoms and seek timely medical intervention. Effective management of FMF through medications like colchicine can significantly reduce the frequency and severity of attacks, thereby lowering the risk of complications such as amyloidosis and kidney disease. Regular follow-ups with healthcare providers, including routine blood tests and kidney function assessments, play a pivotal role in early detection and management of complications.
Lifestyle adjustments, such as adopting an anti-inflammatory diet and maintaining a healthy weight, can also support overall health and potentially mitigate some of the complications associated with FMF. Moreover, genetic counseling may be beneficial for individuals with a family history of FMF, especially for those considering starting a family.
However, while Familial Mediterranean Fever can lead to significant health complications, proactive management and monitoring can help mitigate these risks. Understanding the potential complications and the importance of vigilant care is crucial for those living with FMF and their healthcare providers to ensure the best possible outcomes.
Treatment Options for Familial Mediterranean Fever (FMF)
Managing FMF involves a comprehensive strategy aimed at minimizing episodes, managing acute attacks, and preventing complications, such as amyloidosis. Here’s a closer look at the treatment goals and options for FMF, including medications, therapies, lifestyle adjustments, and home remedies.
Treatment Goals for FMF
The primary objectives in treating FMF are to:
- Prevent Acute Attacks: Reducing the frequency and severity of flare-ups is crucial to improving the quality of life for FMF patients.
- Manage Symptoms: Effective symptom control can significantly reduce discomfort during episodes.
- Prevent Complications: Long-term goals include preventing the development of amyloidosis, a serious complication that can lead to kidney failure.
- Improve Quality of Life: Ultimately, treatments aim to enable individuals to lead active, fulfilling lives despite their condition.
Medications and Therapies Commonly Used in FMF Management
1. Colchicine: This is the cornerstone of FMF treatment. Regular use can prevent attacks and the development of amyloidosis. It’s effective in reducing symptoms for many patients, although some may experience side effects like gastrointestinal discomfort.
2. Anti-inflammatory Medications: For acute flare-ups, non-steroidal anti-inflammatory drugs (NSAIDs) may be used to reduce inflammation and pain.
3. Biologic Agents: In cases where colchicine is ineffective or not tolerated, biologic agents targeting specific inflammatory pathways (e.g., Anakinra, Canakinumab) may be prescribed. These are especially useful in controlling inflammation and preventing flare-ups.
4. Genetic Counseling: Since FMF is a genetic disorder, counseling may be beneficial for patients and their families to understand the condition and its implications.
Lifestyle Adjustments and Home Remedies That May Help Manage Symptoms
1. Diet and Nutrition: While there’s no specific diet for FMF, eating a balanced diet and staying hydrated can help manage overall health. Some individuals find that certain foods trigger their symptoms, so keeping a food diary might be helpful.
2. Stress Management: Stress can exacerbate FMF symptoms, so incorporating stress-reduction techniques like yoga, meditation, or deep-breathing exercises can be beneficial.
3. Regular Exercise: Moderate, regular exercise can help maintain joint flexibility and overall health, but it’s important to avoid overexertion, especially during flare-ups.
4. Adequate Rest: Ensuring sufficient sleep and rest, particularly during episodes, is important in managing FMF symptoms.
5. Avoiding Triggers: If specific triggers for FMF episodes have been identified, avoiding these can help manage the condition.
However, managing Familial Mediterranean Fever involves a comprehensive approach that includes medication, therapy, and lifestyle adjustments. Each patient’s treatment plan should be tailored to their specific needs and regularly reviewed to ensure it continues to meet their health goals. Collaboration between patients and healthcare providers is key to effectively managing FMF and maintaining a high quality of life.
Living with Familial Mediterranean Fever
Here, we explore practical tips for daily management of FMF symptoms, underscore the importance of regular medical check-ups, and highlight support resources available for individuals and families affected by this condition.
Tips for Daily Management of FMF Symptoms
1. Understand Your Triggers: Identifying and avoiding triggers that exacerbate FMF symptoms is crucial. Common triggers include stress, certain foods, and physical exhaustion. Keeping a symptoms diary can help you track and understand your triggers better.
2. Stick to Your Treatment Plan: Consistency in taking prescribed medications, such as colchicine, can prevent flare-ups and reduce symptoms. Always consult your doctor before making any changes to your medication regimen.
3. Adopt a Healthy Lifestyle: A balanced diet, regular exercise, and sufficient sleep can strengthen your immune system and potentially lessen the severity of symptoms. Consider incorporating anti-inflammatory foods into your diet.
4. Stress Management: Since stress can trigger FMF symptoms, finding effective ways to manage stress is vital. Techniques such as mindfulness, meditation, and gentle yoga can be beneficial.
Importance of Regular Medical Check-ups and Communication with Healthcare Providers
Regular Monitoring: FMF requires ongoing management, including regular medical check-ups. These appointments allow your healthcare provider to monitor your condition, adjust treatments as necessary, and prevent complications.
Open Communication: Establishing open communication with your healthcare team is essential. Don’t hesitate to share any changes in your symptoms, concerns about side effects of medications, or any other health issues you might be experiencing.
Support Resources for Individuals and Families Affected by FMF
1. Support Groups: Joining FMF-specific support groups can offer emotional support, valuable insights, and practical tips from others who understand what you’re going through.
2. Educational Resources: Educating yourself and your family about FMF is crucial. Reputable sources such as the FMF Foundation offer a wealth of information, from treatment options to coping strategies.
3. Professional Counseling: Living with a chronic condition can be emotionally taxing. Professional counseling or therapy can provide support in dealing with the psychological aspects of chronic illness.
4. Advocacy and Awareness: Getting involved in FMF advocacy and awareness can be empowering. It provides a sense of community and purpose, helping to bring attention to the needs of those living with FMF.
Remember, you are not alone in this journey. Utilizing available resources and maintaining open lines of communication with your healthcare providers and support network are key to managing FMF effectively.
FAQs on Familial Mediterranean Fever Symptoms
What are the primary symptoms of Familial Mediterranean Fever?
The hallmark symptoms of FMF include episodic fever, abdominal pain, chest pain, and arthritis, particularly in the ankles and knees. These symptoms are a result of inflammation in the abdomen, chest, or joints. Fever episodes typically last from 12 to 72 hours and are often accompanied by signs of inflammation without any apparent infection.
Can FMF cause symptoms outside of fever episodes?
Yes, some individuals with FMF may experience symptoms between fever episodes. These can include muscle aches, fatigue, and a persistent rash. It’s also worth noting that FMF can lead to complications like amyloidosis, which may cause chronic kidney disease, if not properly managed.
How soon do symptoms appear in individuals with FMF?
Symptoms of FMF often begin in childhood or adolescence, typically before the age of 20. Early onset of symptoms is common, but the exact age when symptoms first appear can vary widely among individuals.
Do FMF symptoms differ between children and adults?
While the core symptoms of FMF are similar across age groups, children may have more frequent episodes of fever and may not articulate their symptoms clearly. Abdominal pain and fever are the most common symptoms in children, whereas adults may report more joint involvement and chest pain.
Can stress trigger FMF symptoms?
Stress, both physical and emotional, can indeed trigger an FMF attack. Other potential triggers include certain foods, menstrual cycles in women, and even mild illness. Managing stress and avoiding known triggers can help in reducing the frequency and severity of FMF episodes.
How are FMF symptoms diagnosed?
FMF is diagnosed based on a combination of clinical symptoms, family history, and genetic testing. The presence of the MEFV gene mutation confirms the diagnosis, but a diagnosis can also be made based on symptom history and response to treatment with colchicine, a medication that significantly reduces attack frequency and severity in individuals with FMF.
Can FMF symptoms be managed or treated?
Yes, FMF symptoms can be effectively managed with regular use of colchicine, which helps prevent attacks and reduces the risk of developing amyloidosis. For individuals who do not respond well to colchicine, biologic therapies targeting specific inflammatory pathways may be an option.
Conclusion
If you or someone close to you is experiencing symptoms reminiscent of FMF, such as recurrent fevers, joint pain, or abdominal discomfort, it’s crucial to take these signs seriously. While this article has provided a comprehensive overview, it’s essential to remember that nothing can substitute for professional medical advice. Healthcare professionals can offer tailored advice, accurate diagnoses, and effective treatment plans that are beyond the scope of general information.
Therefore, we strongly encourage anyone who suspects they or a loved one might be dealing with Familial Mediterranean Fever to seek out professional medical consultation. Early diagnosis and intervention can make a significant difference in managing the symptoms and improving the quality of life for those affected. Remember, reaching out for help is a sign of strength and the first step towards recovery.
Let this article serve as a starting point for your journey towards understanding and addressing FMF. With the right information and professional guidance, navigating this condition becomes more manageable, allowing affected individuals and their families to lead fuller, healthier lives.
References
For those seeking more comprehensive insights into Familial Mediterranean Fever (FMF) and its symptoms, the following sources offer detailed information from reputable institutions and research studies. These resources provide a deeper understanding of FMF, including its diagnosis, treatment options, and the latest advancements in research. Whether you’re a patient, caregiver, or healthcare professional, these references can serve as valuable tools for expanding your knowledge on FMF.
- Mayo Clinic: The Mayo Clinic’s overview of Familial Mediterranean Fever offers a concise yet thorough examination of the condition, including symptoms, causes, and treatment options. It is an excellent starting point for individuals looking to understand the basics of FMF. Visit Mayo Clinic’s FMF page.
- National Institutes of Health (NIH): The NIH’s Genetic and Rare Diseases Information Center provides an in-depth look at FMF, covering a wide range of topics from genetic factors to management and treatment strategies. This resource is ideal for readers seeking detailed scientific information and research findings. Read more at NIH’s GARD.
- Orphanet: Offering a comprehensive database on rare diseases, Orphanet presents valuable information on Familial Mediterranean Fever, including epidemiology, pathophysiology, and therapeutic procedures. Orphanet’s articles are peer-reviewed and provide an international perspective on FMF. Explore FMF on Orphanet.
- PubMed Central: For those interested in the latest research studies and clinical trials, PubMed Central offers access to a vast collection of free full-text articles. A search for Familial Mediterranean Fever yields numerous articles, reviews, and study results that can help readers stay up-to-date with the latest advancements in FMF research. Search for FMF articles on PubMed Central.
- American College of Rheumatology (ACR): The ACR provides resources specifically for healthcare professionals, including guidelines on diagnosing and managing Familial Mediterranean Fever. Their resources are based on the latest evidence and expert consensus, making them a reliable source for clinicians. Visit ACR for FMF guidelines.
By exploring these resources, readers can gain a well-rounded understanding of Familial Mediterranean Fever, from its symptoms and causes to the forefront of research and treatment.