Familial Hypercholesterolemia Symptoms: In the realm of inherited health conditions, Familial Hypercholesterolemia (FH) stands out as a critical yet often underdiagnosed condition.
This genetic disorder affects the body’s ability to regulate cholesterol levels, leading to an increased risk of heart disease and stroke.
Understanding the symptoms and causes of Familial Hypercholesterolemia is essential for early detection and management, offering a beacon of hope for those affected.
Understanding Familial Hypercholesterolemia
Familial Hypercholesterolemia (FH) is a genetic disorder that can lead to early heart disease and other serious health issues if not managed properly. It’s characterized by high cholesterol levels, specifically LDL (low-density lipoprotein) cholesterol, which is often referred to as “bad” cholesterol due to its ability to accumulate in the blood vessels and cause blockages. Understanding the prevalence, genetic nature, and implications of FH is crucial for managing and mitigating its impact on health.
Prevalence of Familial Hypercholesterolemia
FH is more common than many might think, affecting 1 in every 250 people worldwide. This prevalence signifies that millions of individuals are living with a higher risk of developing premature cardiovascular disease. Despite its frequency, FH remains underdiagnosed and undertreated, highlighting the importance of raising awareness and improving screening practices to identify and support those affected.
The Genetic Nature of the Condition
The roots of FH lie in the genes. It is inherited in an autosomal dominant manner, meaning that just one copy of the altered gene from an affected parent can lead to the condition. There are specific genes associated with FH, including those involved in the metabolism of LDL cholesterol. Mutations in these genes impair the body’s ability to remove LDL cholesterol from the blood, resulting in its high levels.
The Role of Cholesterol in the Body
Cholesterol plays a pivotal role in the body, contributing to the formation of cell membranes, certain hormones, and vitamin D. However, when its levels in the blood become too high, particularly with LDL cholesterol, the risk of health issues such as heart attacks and strokes increases significantly. The body needs a balanced level of cholesterol for optimal health, but excess LDL cholesterol can lead to the development of plaque in the arteries, a condition known as atherosclerosis, which is a major contributor to heart disease.
Why FH Is a Significant Health Concern
FH is a significant health concern because individuals with this condition have a much higher risk of developing heart disease at a younger age compared to the general population. Without appropriate management, people with FH can develop heart-related conditions as early as their thirties or forties. The inherited nature of FH also means that it affects multiple family members, underscoring the need for family-based screening and intervention strategies.
Early detection and treatment are key in managing FH. Lifestyle changes, medications to lower cholesterol levels, and regular monitoring can help manage the condition and reduce the risk of heart disease. Given the genetic basis of FH, genetic counseling may also be beneficial for affected individuals and their families, providing them with information and support to navigate the implications of this condition.
However, Familial Hypercholesterolemia is a prevalent and serious genetic disorder that requires increased awareness, early detection, and effective management to mitigate its impact on health. Understanding the genetic basis and the role of cholesterol in FH helps in crafting targeted interventions to improve outcomes for those affected.
Symptoms of Familial Hypercholesterolemia
Understanding the symptoms of FH is crucial for early detection and management. This article delves into the common symptoms associated with FH, explores the age-related onset of symptoms, and shares anonymized case studies to illustrate real-life examples.
Common Symptoms Associated with Familial Hypercholesterolemia
Individuals with FH may experience a range of symptoms, often related to the buildup of cholesterol in the body. The most common symptoms include:
- High Cholesterol Levels: Elevated levels of low-density lipoprotein (LDL) cholesterol, often discovered during routine blood tests.
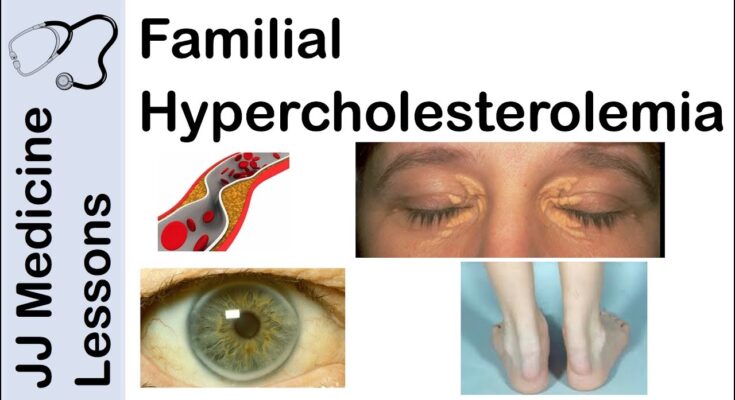
- Xanthomas: Yellowish-orange fatty deposits under the skin, particularly around the eyes, elbows, knees, and buttocks.
- Corneal Arcus: A gray or white arc visible above or below the outer part of the cornea. This symptom is more common in older adults but can appear at any age in people with FH.
- Chest Pain or Angina: Resulting from reduced blood flow to the heart muscles due to narrowed arteries.
- Heart Attack at an Early Age: Individuals with FH are at a higher risk of experiencing a heart attack earlier in life compared to the general population.
Age-related Onset of Symptoms and Variability
The onset and severity of symptoms can vary widely among individuals with FH. While some may show signs of high cholesterol and xanthomas in childhood, others might not experience noticeable symptoms until adulthood. The variability in symptom onset underscores the importance of genetic screening and early intervention, especially for those with a family history of FH or premature heart disease.
Real-life Examples: Case Studies
To illustrate the impact of FH on individuals and the importance of early detection, let’s consider two anonymized case studies:
- Case Study 1: A 35-year-old individual was diagnosed with FH after experiencing chest pain. Despite having a healthy lifestyle, a detailed evaluation revealed high LDL cholesterol levels and xanthomas on their elbows. Early intervention with statin therapy significantly improved their cholesterol levels and reduced the risk of heart disease.
- Case Study 2: In a family screening for FH, a 10-year-old child was found to have elevated cholesterol levels, despite showing no physical symptoms. Genetic testing confirmed the diagnosis of FH. Starting treatment at a young age has been key in managing the child’s cholesterol levels and preventing the early onset of heart disease.
Regular screenings, especially for those with a family history of FH or heart disease, can lead to early diagnosis and significantly better health outcomes. The case studies highlight the importance of awareness and proactive health management in dealing with FH.
Causes and Risk Factors of Familial Hypercholesterolemia
Understanding the causes and risk factors associated with FH is crucial for managing the condition effectively. In this article, we delve into the genetic mutation responsible for FH, how it’s inherited, the environmental and lifestyle factors that can exacerbate its symptoms, and the concept of polygenic FH.
The Genetic Mutation Responsible for FH and Its Inheritance Patterns
Familial Hypercholesterolemia is primarily caused by a genetic mutation that affects the body’s ability to regulate cholesterol levels. The most common mutations occur in the LDL receptor gene, but mutations in other genes such as those encoding apolipoprotein B, PCSK9, and LDLRAP1 can also cause FH. These mutations can significantly increase the risk of heart disease from an early age.
FH is predominantly inherited in an autosomal dominant pattern, meaning only one copy of the mutated gene, inherited from either parent, is sufficient to cause the disorder. This inheritance pattern explains why FH often affects multiple family members across generations. If one parent has FH, each child has a 50% chance of inheriting the condition.
Environmental and Lifestyle Factors That Can Exacerbate Symptoms of FH
While genetic factors play a pivotal role in the development of FH, environmental and lifestyle factors can significantly impact the severity of its symptoms. Factors that can exacerbate symptoms include:
- Diet: High intake of saturated fats and cholesterol can raise LDL cholesterol levels even further in individuals with FH.
- Physical Inactivity: Lack of regular exercise can contribute to higher LDL cholesterol levels and worsen the symptoms of FH.
- Obesity: Carrying excess weight can increase cholesterol levels and compound the risk of cardiovascular complications.
- Smoking: Smoking cigarettes can further increase the risk of heart disease in individuals with FH by damaging the blood vessels.
Managing these lifestyle factors is crucial for individuals with FH to minimize their risk of developing heart disease.
The Concept of Polygenic FH for Individuals with Multiple Minor Gene Variations
Polygenic Familial Hypercholesterolemia is a form of the disorder where individuals have high cholesterol levels not because of a single gene mutation, but due to the cumulative effect of minor variations in several genes associated with cholesterol metabolism. This form of FH can be more challenging to diagnose, as it doesn’t follow the straightforward inheritance patterns seen with monogenic FH. Polygenic FH suggests that even small genetic variations, when combined, can significantly impact cholesterol levels and cardiovascular risk.
However, Familial Hypercholesterolemia is a complex disorder influenced by both genetic and environmental factors. Understanding these factors is essential for effective management and treatment of FH. Individuals with a family history of high cholesterol or heart disease should consider genetic testing and consultation with a healthcare professional to determine their risk and appropriate steps for prevention and management.
Diagnosing Familial Hypercholesterolemia
This guide delves into the diagnostic criteria, the pivotal role of family history, and addresses the challenges faced during diagnosis, emphasizing the significance of early detection.
List of Diagnostic Criteria and Methods
To accurately diagnose Familial Hypercholesterolemia, healthcare providers rely on a combination of clinical evaluations, genetic testing, and lipid profiling. The primary diagnostic criteria include:
- Elevated LDL Cholesterol Levels: Significantly high levels of LDL cholesterol are a hallmark of FH. Levels vary with age and are typically above the 95th percentile for the general population.
- Physical Signs: Visible symptoms such as xanthomas (cholesterol deposits in the skin or tendons) and corneal arcus (cholesterol deposit around the cornea) can indicate FH.
- Genetic Testing: Identifying mutations in genes responsible for cholesterol regulation (e.g., LDLR, ApoB, or PCSK9) provides a definitive diagnosis.
- Family History: A strong history of premature cardiovascular disease or high cholesterol levels among immediate family members supports an FH diagnosis.
The Importance of Family History in Diagnosing FH
Family history plays a crucial role in diagnosing Familial Hypercholesterolemia. It provides insights into the genetic component of the disease, enabling healthcare providers to identify at-risk individuals early. Documenting and evaluating cardiovascular diseases and cholesterol levels in parents, siblings, and extended family members help in predicting the likelihood of FH. This knowledge facilitates targeted screening and personalized treatment plans, significantly improving outcomes for those affected.
Challenges in Diagnosing FH and the Importance of Early Detection
Despite clear diagnostic criteria, diagnosing FH poses several challenges. The variability in symptom presentation and overlap with other types of hypercholesterolemia often lead to underdiagnosis or misdiagnosis. Additionally, the lack of awareness and screening practices contribute to delayed detection.
Early detection of FH is imperative for preventing cardiovascular diseases. Implementing routine cholesterol screenings, especially for those with a family history of high cholesterol or heart disease, can lead to timely intervention. Early diagnosis allows for the management of cholesterol levels through lifestyle changes, medications, and, in some cases, more aggressive treatments to prevent heart disease.
With early detection and appropriate treatment, individuals with FH can lead long, healthy lives, minimizing the risk of cardiovascular diseases. It underscores the need for heightened awareness, routine screenings, and a comprehensive approach to healthcare that includes the familial context in diagnosing genetic disorders like FH.
Managing Symptoms of Familial Hypercholesterolemia
Managing its symptoms effectively involves a multifaceted approach that includes lifestyle modifications, medication, and regular monitoring. Below, we outline strategies to control cholesterol levels and mitigate the risks associated with FH.
Lifestyle Modifications
One of the cornerstones of managing FH is through lifestyle changes that help control cholesterol levels:
- Diet: Adopting a heart-healthy diet is crucial. Focus on incorporating foods rich in omega-3 fatty acids, such as salmon and flaxseeds, and increase your intake of fruits, vegetables, and whole grains. Limit consumption of saturated fats found in red meat and dairy products, and avoid trans fats commonly found in processed foods.
- Exercise: Regular physical activity can help lower LDL (bad) cholesterol and improve overall heart health. Aim for at least 30 minutes of moderate exercise, such as brisk walking, cycling, or swimming, most days of the week.
- Weight Management: Achieving and maintaining a healthy weight can help lower cholesterol levels and reduce the risk of heart disease.
- Avoid Smoking: Smoking can exacerbate the effects of high cholesterol, leading to faster development of clogged arteries. Quitting smoking can significantly improve heart health.
Medication Options
For many people with FH, lifestyle changes alone are not enough to reduce cholesterol to safe levels. Medications play a key role in managing the condition:
- Statins: These are the most commonly prescribed medications for lowering cholesterol. They work by inhibiting an enzyme the liver uses to produce cholesterol, thereby lowering LDL cholesterol levels.
- PCSK9 Inhibitors: For individuals who do not respond adequately to statins, PCSK9 inhibitors can be an effective alternative. These drugs work by helping the liver remove more LDL cholesterol from the blood.
Monitoring and Follow-Up Care
Regular follow-ups with a healthcare provider are essential for anyone with FH. These appointments allow for monitoring the effectiveness of the treatment plan and making adjustments as necessary:
- Regular Cholesterol Testing: Monitoring cholesterol levels helps assess the effectiveness of the treatment plan and whether any adjustments are needed.
- Assessment of Heart Health: Regular screenings for signs of heart disease may be recommended, including blood pressure monitoring, blood tests for inflammation, and possibly imaging tests.
By adhering to these recommendations, individuals with FH can significantly reduce their risk of heart disease and lead healthier lives. Consult with a healthcare provider to develop a personalized plan that best meets your needs.
Prevention and Awareness of Familial Hypercholesterolemia
In this guide, we’ll explore effective strategies for at-risk individuals, the importance of genetic counseling, and the role of public health initiatives in combating FH.
Strategies for At-Risk Individuals
For individuals at risk of FH, proactive measures can significantly reduce the likelihood of severe symptoms and improve quality of life. Key strategies include:
- Regular Health Screenings: Early detection through cholesterol level checks can identify FH at a manageable stage.
- Lifestyle Modifications: Adopting a heart-healthy diet, engaging in regular physical activity, and avoiding tobacco products can help manage cholesterol levels.
- Medication Adherence: For many, lifestyle changes alone may not be enough. Statins and other cholesterol-lowering medications, prescribed by healthcare professionals, are vital in controlling FH.
- Family Health History: Understanding your family health history can alert you to the potential risk of FH, prompting early intervention.
The Role of Genetic Counseling
Genetic counseling is indispensable for families affected by FH. It offers:
- Personalized Risk Assessment: Genetic counselors can assess individual and family risks for FH, providing a clearer understanding of the condition.
- Informed Decision-Making: Counselors guide families through potential health decisions, including the implications of genetic testing for family members.
- Support and Resources: Families receive emotional support and access to resources and communities for ongoing management of FH.
Public Health Initiatives and Awareness Campaigns
Increasing public knowledge about FH is critical for early detection and management. Public health initiatives and awareness campaigns aim to:
- Educate the Public: Through informative campaigns, individuals learn about FH symptoms, risks, and the importance of cholesterol management.
- Promote Screening Programs: Encouraging regular cholesterol screenings can lead to early detection of FH, preventing more serious health issues.
- Support Affected Families: By providing resources and support, these initiatives help families navigate the complexities of FH management.
Awareness, early detection, and proactive management are key to preventing severe symptoms and ensuring those affected can lead healthy lives. Public health initiatives and genetic counseling play pivotal roles in educating and supporting at-risk individuals and their families, making FH a manageable condition rather than a daunting diagnosis.
FAQs on Familial Hypercholesterolemia Symptoms
What is Familial Hypercholesterolemia (FH)?
Familial Hypercholesterolemia is a genetic condition characterized by high cholesterol levels, particularly low-density lipoprotein (LDL), or “bad” cholesterol. It increases the risk of heart disease from a young age.
How do I know if I have FH? What are the symptoms?
Most individuals with FH might not experience any overt symptoms until the onset of heart disease. However, some signs can include fatty deposits in the skin or tendons (xanthomas), a gray or white color in the cornea (corneal arcus), or chest pain (angina) due to heart disease.
Can children have symptoms of FH?
Yes, children can have FH. While they may not show symptoms early on, they can develop fatty deposits in their skin or tendons, which are tell-tale signs. Early screening is recommended for children with a family history of FH or heart disease.
Are there any specific signs of FH that I should look out for?
Yes, specific signs to watch for include fatty growths around the eyes, knuckles, or Achilles tendons, and a family history of early heart disease. If you notice these signs or have a family history, it’s important to consult a healthcare provider for evaluation.
How is FH diagnosed?
FH is diagnosed through a combination of family history, physical exams, and blood tests to measure cholesterol levels. Genetic testing may also be recommended to confirm the diagnosis.
Can FH be treated?
Yes, FH can be managed with lifestyle changes, medications to lower cholesterol levels, and, in some cases, procedures to remove cholesterol from the blood. Early diagnosis and treatment are crucial to managing the condition effectively.
Does having FH mean I will definitely develop heart disease?
While FH significantly increases the risk of developing heart disease at an early age, it’s not a certainty. With appropriate management, including medication, lifestyle changes, and regular monitoring, individuals with FH can lead healthy lives.
Where can I find more information or support for FH?
Several organizations offer resources, support groups, and information for individuals with FH and their families. It’s also important to consult healthcare providers who specialize in lipid disorders for personalized advice and treatment plans.
Conclusion
If you have a family history of high cholesterol or cardiovascular diseases, the call to action could not be clearer: consider getting screened for FH. This proactive approach can be a pivotal step in safeguarding your health and ensuring a better quality of life. Screening is a simple process, yet it holds the power to alter the course of your health journey positively.
Furthermore, the continuous research and support for individuals with Familial Hypercholesterolemia are crucial. It’s through ongoing studies and advancements in medical science that we can hope to find more comprehensive treatments and possibly a cure in the future. Supporting this cause not only helps those currently affected by FH but also protects future generations from the grips of this genetic condition.
In closing, let us all recognize the significance of early detection and support for Familial Hypercholesterolemia. It’s a collective effort that promises a healthier future for individuals and their families affected by this condition. Whether you’re considering screening for yourself, advocating for more research, or offering support to those affected, every action counts towards a greater good. Together, we can make a difference in the lives of those living with Familial Hypercholesterolemia.
References
For further reading and to validate the information provided about Familial Hypercholesterolemia (FH) symptoms, we recommend consulting the following reputable sources:
- Centers for Disease Control and Prevention (CDC) – The CDC offers an in-depth overview of Familial Hypercholesterolemia, including symptoms, causes, and treatments. A valuable resource for understanding how FH affects individuals and public health strategies for management. Read more at the CDC.
- Mayo Clinic – Renowned for its patient care and health information, the Mayo Clinic provides a detailed guide on Familial Hypercholesterolemia. This includes symptom lists, diagnostic methods, and potential lifestyle changes and treatments. Explore Mayo Clinic’s FH Guide.
- National Heart, Lung, and Blood Institute (NHLBI) – As part of the National Institutes of Health, the NHLBI provides comprehensive resources on Familial Hypercholesterolemia, covering research, treatment strategies, and ongoing studies. Visit NHLBI for detailed information.
- Genetic and Rare Diseases Information Center (GARD) – An excellent source for understanding the genetic aspect of FH and its rarity. GARD offers detailed explanations on symptoms, inheritance patterns, and links to further research. Check out GARD’s Familial Hypercholesterolemia page.
By consulting these sources, readers can deepen their understanding of Familial Hypercholesterolemia, from its symptoms and causes to the latest in treatment and research. These links were selected for their authority, depth of information, and accessibility to ensure readers have access to reliable and up-to-date information.