Familial Hypercholesterolemia Treatment: Familial Hypercholesterolemia (FH) is a genetic disorder characterized by high cholesterol levels, particularly high levels of low-density lipoprotein (LDL), often referred to as “bad” cholesterol.
This condition elevates the risk of developing heart disease at an early age. Understanding and managing FH is crucial for those affected and their families.
Understanding Familial Hypercholesterolemia
Familial Hypercholesterolemia (FH) is a genetic disorder characterized by high cholesterol levels, specifically low-density lipoprotein (LDL), often referred to as “bad” cholesterol. Understanding FH is crucial for early diagnosis and management to prevent cardiovascular diseases. This section delves into the epidemiology, genetic factors, and symptoms of FH, providing a comprehensive overview of the condition.
Epidemiology: Prevalence and Demographics Affected
Familial Hypercholesterolemia is relatively common, affecting 1 in every 250 people globally. However, rates can vary significantly among populations. For instance, certain communities may have a higher prevalence due to founder effects and genetic isolation. Despite its widespread nature, FH often remains underdiagnosed and undertreated, partly due to a lack of awareness and testing.
The condition affects both males and females equally and can manifest at any age, including in children. The universal nature of FH underscores the importance of understanding its impact across diverse demographic groups. Early detection and intervention are key to managing FH and reducing the risk of heart disease.
Genetics Behind FH: Understanding the Hereditary Nature
FH is primarily caused by mutations in genes that regulate cholesterol metabolism. The most common genes involved include LDLR (low-density lipoprotein receptor), APOB (apolipoprotein B), and PCSK9 (proprotein convertase subtilisin/kexin type 9). These mutations lead to the inefficient clearance of LDL cholesterol from the bloodstream, resulting in its accumulation and high blood cholesterol levels.
The disorder follows an autosomal dominant inheritance pattern, meaning a mutation in just one copy of the gene (inherited from either parent) is sufficient to cause the condition. This genetic aspect makes FH a hereditary condition, with a 50% chance of passing it to offspring, emphasizing the need for family screening and genetic counseling.
Symptoms of Familial Hypercholesterolemia
Individuals with FH may exhibit several signs and symptoms, often related to the effects of high cholesterol on the cardiovascular system. Key symptoms include:
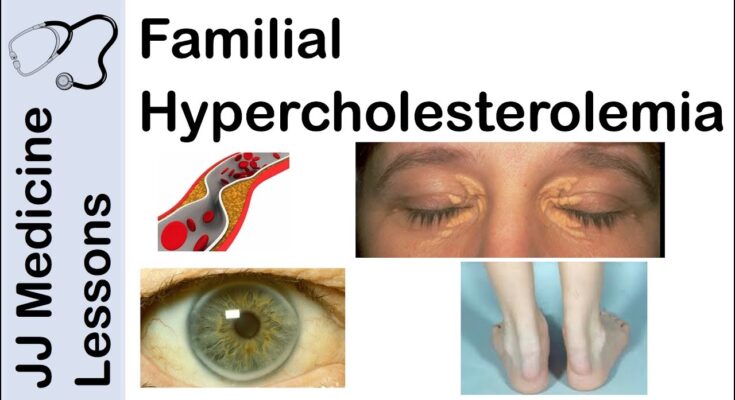
- Xanthomas: Yellowish deposits of cholesterol under the skin, especially around the eyelids (xanthelasmas), elbows, knees, and buttocks.
- Corneal Arcus: A gray or white ring around the cornea of the eye, indicative of cholesterol deposits.
- Chest Pain or Angina: Due to the buildup of plaque in the arteries that supply the heart.
- Heart Attacks and Strokes: At younger ages than typical, caused by accelerated atherosclerosis (hardening and narrowing of arteries).
It’s crucial to note that some people with FH may not show visible symptoms for years, which is why genetic screening and regular cholesterol checks are essential for those with a family history of high cholesterol or premature heart disease.
However, understanding Familial Hypercholesterolemia is pivotal in the early detection and management of the condition. Recognizing the signs and knowing the genetic risk can lead to timely interventions, reducing the risk of heart disease and improving quality of life for affected individuals and their families.
Diagnosing Familial Hypercholesterolemia: A Guide to Early Detection and Methods
Early detection and treatment are crucial for managing this condition effectively. This comprehensive guide outlines the importance of early diagnosis, methods for diagnosing FH, screening guidelines, and the critical role of family history in the diagnostic process.
The Importance of Early Detection in Familial Hypercholesterolemia Treatment
Early detection of Familial Hypercholesterolemia is paramount. Identifying FH early can lead to prompt treatment, greatly reducing the risk of heart disease and stroke. With early intervention, individuals can manage their cholesterol levels through lifestyle changes, medications, or a combination of both, potentially saving lives and improving quality of life.
List of Methods for Diagnosing Familial Hypercholesterolemia
Diagnosing FH involves a combination of clinical evaluation, genetic testing, and understanding the individual’s family history. Here’s a closer look at each method:
- Clinical Evaluation: Healthcare professionals look for physical signs of elevated cholesterol, such as xanthomas (cholesterol deposits in the skin) or corneal arcus (cholesterol deposit around the cornea of the eye).
- Genetic Testing: This method confirms the diagnosis by identifying mutations in genes responsible for FH. It’s particularly useful for at-risk family members.
- Lipid Testing: A simple blood test can measure cholesterol levels, providing initial indicators of FH.
Screening Guidelines: Who Should Get Tested and When
Screening for FH is recommended for individuals with a family history of premature heart disease or high cholesterol levels. Children in families with a known history of FH should undergo cholesterol testing between the ages of 9 and 11, and then again between 17 and 21. Adults with no symptoms should be screened every 4 to 6 years, while those with risk factors may need more frequent testing.
Diagnostic Criteria for FH: Clinical Signs and Genetic Testing
The diagnostic criteria for FH include a combination of high LDL cholesterol levels, family history of FH or premature heart disease, and physical signs of high cholesterol. Genetic testing can confirm the diagnosis, providing a clear indication of the condition’s presence.
The Role of Family History in Diagnosing FH
Family history plays a crucial role in diagnosing Familial Hypercholesterolemia. A detailed family history of heart disease, stroke, or high cholesterol can prompt earlier screening and diagnosis, leading to timely treatment. Sharing this information with your healthcare provider can help tailor the diagnostic process and treatment plan to your specific needs.
However, early detection and diagnosis of Familial Hypercholesterolemia are critical steps in managing this condition and reducing the risk of heart disease. Through a combination of screening, clinical evaluation, and acknowledging the importance of family history, individuals at risk can receive the necessary care to lead healthy lives.
Treatment Options for Familial Hypercholesterolemia
Managing FH effectively involves a comprehensive approach combining lifestyle changes, pharmacological treatments, and, in some cases, advanced therapies. Here, we explore the treatment objectives, strategies, and the distinct approaches needed for managing FH in children versus adults, aimed at improving outcomes and enhancing quality of life.
Objectives and Strategies for Treating Familial Hypercholesterolemia
The primary objectives in treating FH are to lower cholesterol levels, particularly low-density lipoprotein (LDL) cholesterol, to reduce the risk of heart disease, and to prevent the onset of cardiovascular events. Strategies to achieve these objectives include lifestyle modifications, pharmacological interventions, and advanced therapeutic options, each tailored to the individual’s specific needs and health status.
Lifestyle Modifications
Lifestyle changes are foundational in managing FH and can significantly impact overall health and cholesterol levels. Key lifestyle modifications include:
- Diet: Adopting a heart-healthy diet that’s low in saturated fats and cholesterol and rich in fruits, vegetables, whole grains, and lean protein can help lower LDL cholesterol levels.
- Exercise: Regular physical activity helps improve heart health, increase HDL (good) cholesterol, and can contribute to weight loss. Aim for at least 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise per week.
- Weight Management: Achieving and maintaining a healthy weight can help lower cholesterol levels and reduce the risk of heart complications.
Pharmacological Treatments
When lifestyle modifications are not enough to reach cholesterol goals, medication may be necessary:
- Statins: These are the cornerstone of pharmacological treatment for FH, working to lower LDL cholesterol by slowing down the liver’s production of cholesterol.
- PCSK9 Inhibitors: These newer medications can significantly lower LDL cholesterol levels and are often used in people who have a genetic condition leading to high cholesterol or in those who cannot tolerate statins.
- Other Medications: Depending on individual needs, other drugs like ezetimibe (which reduces the amount of cholesterol absorbed by the body) or bile acid sequestrants (which bind to bile acids, forcing the body to use excess cholesterol to make more bile acids) may be used.
Advanced Therapies
For individuals with severe FH or those who do not respond adequately to medication, advanced therapies may be considered:
- LDL Apheresis: Similar to dialysis, this process removes LDL cholesterol from the blood and is typically done every two weeks.
- Potential Future Treatments: Research is ongoing into gene therapies and other innovative treatments that target the underlying genetic causes of FH.
Managing FH in Children vs. Adults
The management of FH in children requires a careful, age-appropriate approach compared to adults:
- Children: Lifestyle interventions are the first line of treatment. Medications, typically statins, may be considered for children as young as 8 to 10 years old if lifestyle changes are insufficient and the child has a family history of early heart disease or other risk factors.
- Adults: Treatment typically involves a combination of lifestyle modifications and medication. The approach may be more aggressive in adults, especially those with additional risk factors for cardiovascular disease.
By integrating lifestyle changes, pharmacological treatments, and possibly advanced therapies, individuals with FH can manage their condition effectively. Regular monitoring and personalized care strategies, considering the differences between children and adults, are essential to achieving optimal health outcomes.
Challenges in Managing Familial Hypercholesterolemia
Here, we delve into the complexities of handling this condition, focusing on recognizing barriers to effective treatment, improving treatment adherence, and monitoring the long-term health implications associated with FH.
Recognizing and Overcoming Barriers to Effective Treatment
One of the primary hurdles in managing FH is the late or missed diagnosis. Given its hereditary nature, many individuals may not realize they are at risk until the condition has progressed significantly. Educating both the public and healthcare professionals about the signs and genetic markers of FH is crucial for early identification and intervention.
Another challenge is the accessibility and affordability of treatment. Advanced lipid-lowering therapies can be costly and may not be readily available in all regions. Healthcare systems must strive to make these treatments more accessible to those diagnosed with FH to prevent the progression of heart disease.
Adherence to Treatment: Strategies for Success
Treatment adherence is another critical aspect of managing FH effectively. The long-term nature of FH treatment, often involving daily medication, lifestyle adjustments, and regular health checks, can be overwhelming for patients. Here are strategies to enhance adherence:
- Educational Support: Providing patients with comprehensive information about FH and the importance of ongoing treatment can motivate adherence.
- Personalized Care Plans: Tailoring treatment plans to fit individual lifestyles and preferences can improve patient engagement and adherence.
- Regular Follow-ups: Scheduled check-ins with healthcare providers help monitor progress, address concerns, and adjust treatments as needed.
Monitoring and Managing Long-Term Health Implications of FH
Long-term management of FH involves vigilant monitoring of heart health and cholesterol levels. Regular cardiovascular evaluations are necessary to detect and address any arising complications early. Additionally, patients should be informed about the potential long-term effects of FH on their health and the importance of maintaining a heart-healthy lifestyle.
Lifestyle modifications, including a balanced diet, regular physical activity, and smoking cessation, play a vital role in managing FH. These changes, alongside medication, can significantly reduce the risk of heart disease and improve overall health outcomes.
However, effectively managing Familial Hypercholesterolemia requires a multifaceted approach. Early detection, accessible treatments, adherence strategies, and ongoing monitoring are all crucial components of a successful management plan. By addressing these challenges head-on, patients with FH can lead healthier, longer lives.
The Role of Healthcare Professionals in Familial Hypercholesterolemia Management
Effective management of FH requires a comprehensive approach, emphasizing the crucial role of healthcare professionals. By employing a multidisciplinary strategy, providing patient education, and staying updated with the latest research and guidelines, healthcare providers can significantly improve outcomes for patients with FH.
Multidisciplinary Approach: Collaborating Across Specialties
The complexity of FH necessitates a multidisciplinary approach, bringing together healthcare professionals from various specialties to provide holistic care. Cardiologists, endocrinologists, genetic counselors, dietitians, and primary care physicians must work in concert to develop and implement personalized treatment plans. This collaborative effort ensures that all aspects of the patient’s health are addressed, from genetic testing and medication management to lifestyle modifications and preventive care. By fostering teamwork across specialties, healthcare providers can deliver more effective and coordinated care, ultimately enhancing the quality of life for individuals with FH.
Patient Education and Support: Tools and Resources for Patients and Families
Educating patients and their families about FH is paramount to successful management. Healthcare professionals play a key role in providing accurate information, resources, and support to help individuals understand their condition and the necessary steps to manage it effectively. This includes guidance on diet, exercise, medication adherence, and the importance of regular health check-ups. Additionally, offering resources such as support groups and educational materials can empower patients and their families, making them active participants in the management of FH. Patient education not only helps in mitigating the impact of the condition but also in reducing the risk of complications associated with FH.
Staying Updated: The Importance of Ongoing Research and Guidelines
The field of FH management is constantly evolving, with ongoing research shedding new light on effective treatments and strategies. Healthcare professionals must stay abreast of the latest developments, research findings, and clinical guidelines to provide the best care possible. This commitment to continuous learning enables providers to integrate new evidence-based practices into patient care plans, improving outcomes. Staying informed about advancements in genetic testing, novel therapeutic options, and guideline updates is crucial for the proactive management of FH.
However, the role of healthcare professionals in the management of familial hypercholesterolemia is multifaceted, requiring a collaborative, informed, and patient-centered approach. By working together across disciplines, providing comprehensive patient education, and staying updated with the latest in FH research and guidelines, healthcare providers can significantly impact the lives of those affected by this challenging condition.
Patient Case Studies and Success Stories: Transforming Lives with Familial Hypercholesterolemia Treatment
Discover the power of effective diagnosis and treatment through real-life patient case studies and success stories of individuals battling Familial Hypercholesterolemia (FH). These narratives not only shed light on the challenges faced by patients with FH but also highlight the remarkable outcomes achieved through personalized treatment plans.
The Journey to Diagnosis
Familial Hypercholesterolemia, a genetic disorder characterized by high cholesterol levels, often goes undetected due to its asymptomatic nature in the early stages. However, early diagnosis can significantly alter the course of treatment and prevent severe cardiovascular diseases. Our case studies begin with the story of individuals who, through vigilant healthcare screening and genetic testing, were diagnosed with FH. These stories emphasize the importance of awareness and early detection in managing this inheritable condition.
Crafting Personalized Treatment Plans
Following diagnosis, the creation of a personalized treatment plan is crucial. Our success stories delve into the tailored approaches adopted by healthcare professionals to manage FH effectively. These include a combination of lifestyle modifications, medication, and in some cases, advanced therapies like LDL apheresis. By focusing on the individual needs and genetic makeup of each patient, these personalized plans demonstrate a higher success rate in lowering cholesterol levels and reducing the risk of heart disease.
Transformative Outcomes
The impact of personalized treatment plans on patient outcomes is profound. Through our collection of success stories, we witness the transformative journey of patients who went from high-risk profiles to leading healthier lives with managed cholesterol levels. These narratives not only inspire hope but also underscore the importance of a patient-centered approach in treating Familial Hypercholesterolemia.
Each story is a testament to the resilience of patients and the dedication of healthcare providers in the fight against FH. They illuminate the pathway towards a healthier future, underscoring the significance of personalized treatment in achieving optimal health outcomes.
In the battle against Familial Hypercholesterolemia, these real-life examples offer insight, inspiration, and evidence of what can be achieved through dedicated care and tailored treatment strategies.
FAQs on Familial Hypercholesterolemia Treatment
What is Familial Hypercholesterolemia (FH)?
Familial Hypercholesterolemia is a genetic disorder characterized by high LDL cholesterol levels, which can lead to an increased risk of heart disease. It is inherited, meaning it’s passed down from parents to children.
How is Familial Hypercholesterolemia treated?
The treatment of FH focuses on lowering LDL cholesterol levels. This usually involves a combination of lifestyle changes, such as diet and exercise, and medication. Statins are the most common type of medication prescribed, but other options may include PCSK9 inhibitors, bile acid sequestrants, and cholesterol absorption inhibitors.
Can diet and exercise alone manage FH?
While diet and exercise are critical components of managing FH, they are often not enough to lower cholesterol levels to a safe range on their own. Most individuals with FH will require medication to effectively reduce their LDL cholesterol levels.
Are there any side effects of FH treatments?
Like all medications, those used to treat FH can have side effects. Statins, for example, may cause muscle pain, digestive problems, and increased blood sugar levels. It’s important to discuss potential side effects with your healthcare provider.
Is Familial Hypercholesterolemia curable?
Currently, there is no cure for Familial Hypercholesterolemia. However, with appropriate treatment and lifestyle changes, individuals with FH can manage their cholesterol levels effectively and reduce their risk of heart disease.
How often should someone with FH see a doctor?
Individuals with FH should have regular check-ups with their healthcare provider to monitor their cholesterol levels and adjust their treatment plan as necessary. Typically, this may be every 3 to 6 months, depending on the severity of their condition and their response to treatment.
Can children be treated for FH?
Yes, children can be treated for Familial Hypercholesterolemia. Early diagnosis and treatment are crucial to prevent the development of heart disease later in life. The treatment plan for children may include lifestyle changes and, in some cases, medication.
Is genetic testing available for FH?
Yes, genetic testing can identify the specific mutations causing FH. This can be helpful for confirming the diagnosis and may also provide information that can guide treatment decisions. Additionally, it can identify at-risk family members who may also need treatment.
Can lifestyle changes prevent Familial Hypercholesterolemia?
While lifestyle changes cannot prevent FH, as it is a genetic condition, they are essential for managing cholesterol levels and reducing the risk of heart disease. A heart-healthy diet, regular exercise, and avoiding smoking can significantly benefit individuals with FH.
Where can I find support for managing FH?
Several organizations offer resources and support for individuals with Familial Hypercholesterolemia and their families. These include patient advocacy groups, online communities, and healthcare providers specializing in lipid disorders.
Conclusion:
Encountering FH requires a multifaceted approach, integrating lifestyle modifications with possible pharmacological interventions to manage cholesterol levels effectively.
The journey towards a healthier life begins with awareness and is sustained by the commitment to proactive health management. For individuals at risk, the call to action cannot be overstated.
Undergoing genetic testing and regular cholesterol screenings is a critical step in unveiling the presence of FH, enabling early and targeted interventions that can drastically alter the course of one’s health trajectory.
References
For those seeking more in-depth information and validation of the treatment options for Familial Hypercholesterolemia, we have compiled a list of reputable sources. These references are crucial for patients, healthcare professionals, and researchers who wish to explore the latest in disease management and therapy advancements.
- National Heart, Lung, and Blood Institute (NHLBI): The NHLBI offers comprehensive guidelines and resources on the diagnosis, treatment, and management of Familial Hypercholesterolemia. Their publications are grounded in extensive research and are invaluable for understanding the disease. Visit NHLBI on Familial Hypercholesterolemia.
- Mayo Clinic: Renowned for its patient care and research, the Mayo Clinic offers an overview of Familial Hypercholesterolemia, its symptoms, causes, and treatment options. Their website is a trusted source for medical information and patient education. Learn More at Mayo Clinic.
- PubMed Central (PMC): PMC is a free full-text archive of biomedical and life sciences journal literature. It is a valuable resource for those looking to delve into the scientific research and clinical studies on Familial Hypercholesterolemia. Search PMC for Familial Hypercholesterolemia Studies.
By exploring these resources, readers can gain a comprehensive understanding of Familial Hypercholesterolemia, including the latest treatment options and research findings. These references are instrumental in providing high-quality, evidence-based information that supports informed decision-making in healthcare.