Epilepsy Treatment: Epilepsy is a neurological condition characterized by the occurrence of recurrent, unprovoked seizures. It affects millions of people worldwide, across all ages, genders, and ethnic backgrounds.
Understanding the nuances of epilepsy diagnosis and treatment is crucial for improving the quality of life for those affected by this condition.
This comprehensive guide delves into the latest methodologies and treatment options available, offering hope and actionable insights for patients and their families.
Understanding Epilepsy
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures. These seizures result from sudden, excessive electrical discharges in a group of brain cells. Different parts of the brain can initiate a seizure either in isolation or spread to the whole brain, affecting consciousness, movements, and sensations. Understanding the types of epilepsy and seizures, alongside their causes and risk factors, is crucial for managing this condition effectively.
Definition and Types of Epilepsy
Epilepsy encompasses a spectrum of brain disorders varying in severity, ranging from benign to more severe conditions. It’s classified based on the type of seizure experienced, which helps in understanding the part of the brain affected and the best treatment approaches. The two primary types of seizures are generalized seizures and focal seizures.
- Generalized Seizures: These seizures involve all areas of the brain from the onset. They are further divided into several categories, including absence seizures (brief loss of consciousness), tonic-clonic seizures (previously known as grand mal seizures, involving muscle rigidity and convulsions), and myoclonic seizures (sudden muscle jerks), among others.
- Focal Seizures: Previously known as partial seizures, focal seizures originate in a specific part of the brain and can affect both consciousness and specific parts of the body. They can remain localized or spread to other brain areas, becoming generalized. Focal seizures are categorized based on the level of awareness during the seizure: focal aware seizures (consciousness not impaired) and focal impaired awareness seizures (consciousness is impaired).
Causes and Risk Factors
Several factors contribute to the development of epilepsy. While in many cases the exact cause remains unknown, known factors include:
- Genetic Predisposition: Family history of epilepsy increases the risk of developing the condition. Certain genes are known to influence the likelihood of seizures, and genetic testing may help in some cases to determine risk.
- Brain Conditions or Injuries: Traumatic brain injuries, stroke, brain tumors, and conditions that cause brain damage, such as neurofibromatosis or tuberous sclerosis, can lead to epilepsy. Brain injuries are among the most common causes of epilepsy in adults over the age of 35.
- Infectious Diseases: Infections such as meningitis, viral encephalitis, and HIV/AIDS can cause epilepsy. Preventing these infections can lower the risk of developing seizures.
- Developmental Disorders: Neurodevelopmental disorders, including autism and neurofibromatosis, have been linked to a higher risk of epilepsy. These conditions may affect brain development and function, leading to seizures.
By recognizing the types of seizures and identifying potential causes and risk factors, individuals and healthcare providers can work together to develop a comprehensive treatment plan. Lifestyle adjustments, medication, and sometimes surgery can help manage epilepsy, improving the quality of life for those affected.
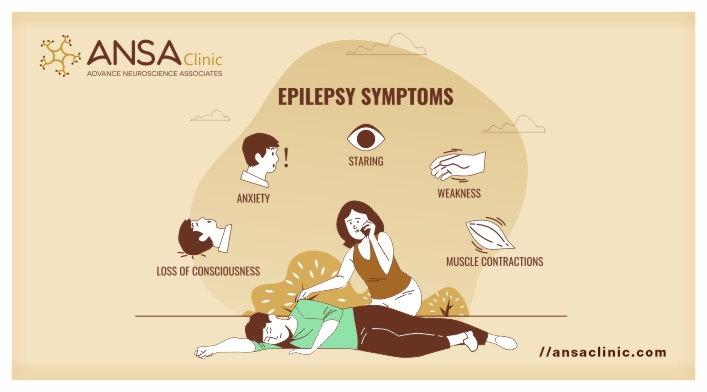
Signs and Symptoms of Epilepsy
Understanding the signs and symptoms of epilepsy is crucial for early diagnosis and effective management. Here, we’ll explore the common indicators of seizures, how to distinguish between different seizure types, and when it’s essential to seek medical advice.
Common Indicators of Seizures
Seizures can manifest in various ways, but some common indicators include:
- Sudden Confusion: A temporary state of confusion where the person may not understand what is happening around them.
- Staring Spells: Brief, unresponsive periods where the individual stares blankly into space.
- Uncontrollable Jerking Movements: Movements of the arms and legs that are sudden, brief, and cannot be controlled.
- Loss of Consciousness or Awareness: The person may lose consciousness or awareness of their surroundings, even if for a short time.
- Psychic Symptoms: These might include fear, anxiety, or experiencing deja vu.
Recognizing these signs early on can be a significant step towards managing epilepsy effectively.
Distinguishing Between Seizure Types
Seizures are primarily classified into two categories: focal (partial) seizures and generalized seizures.
- Focal Seizures: These originate in just one part of the brain. Symptoms may vary depending on the affected area and can range from involuntary jerking of a body part to experiencing sudden, intense emotions or changes in the sense of taste, smell, sight, hearing, or touch.
- Generalized Seizures: These affect all areas of the brain. Types include absence seizures (brief loss of awareness), tonic-clonic seizures (convulsions, muscle stiffness, and loss of consciousness), and several others, each presenting with its unique set of symptoms.
Understanding the type of seizure can help in tailoring the treatment approach effectively.
When to Seek Medical Advice
It’s imperative to seek medical advice if you or someone you know experiences:
- A seizure for the first time.
- Seizures that happen more frequently than usual.
- Seizures that last longer than usual or appear different.
- Difficulty regaining consciousness or breathing after a seizure.
- A seizure that occurs in water, posing a risk of drowning.
- Seizures alongside symptoms like high fever, heat exhaustion, or during pregnancy.
Immediate medical help can prevent complications and improve the quality of life for those with epilepsy.
With appropriate treatment and support, many individuals with epilepsy can lead full, active lives. If you suspect you or someone close to you is exhibiting signs of epilepsy, do not hesitate to consult a healthcare professional for an accurate diagnosis and tailored treatment plan.
Diagnosing Epilepsy: A Comprehensive Guide
Diagnosing epilepsy involves a detailed evaluation process, encompassing medical history review, physical examinations, and a series of diagnostic tests. This comprehensive approach ensures accurate diagnosis and effective management of epilepsy. Understanding the diagnostic process is crucial for patients and caregivers alike.
Medical History and Physical Examination
The first step in diagnosing epilepsy is a thorough review of the patient’s medical history and a comprehensive physical examination. Healthcare providers inquire about the frequency, duration, and type of seizures experienced. They also consider any potential triggers or preceding symptoms. Information about the patient’s family history of epilepsy or other neurological conditions is equally important. This initial assessment provides critical insights into the patient’s condition and guides further diagnostic testing.
Diagnostic Tests and Procedures
Following the initial evaluation, a series of diagnostic tests and procedures are typically recommended to confirm the presence of epilepsy and determine its type and cause. These include:
Electroencephalogram (EEG)
The EEG is the most commonly used test for diagnosing epilepsy. It records electrical activity in the brain through electrodes attached to the scalp. EEGs can identify abnormal patterns that indicate a tendency toward seizures, providing vital information about the type and focus of seizures.
Magnetic Resonance Imaging (MRI)
An MRI uses powerful magnets and radio waves to create detailed images of the brain. It can detect abnormalities such as tumors, brain damage, or developmental disorders that may cause seizures. MRI scans are crucial for identifying the underlying causes of epilepsy and assisting in treatment planning.
Computed Tomography (CT) Scan
A CT scan provides cross-sectional images of the brain using X-rays. It helps in detecting structural brain abnormalities, such as hemorrhages or tumors, that might lead to seizures. Though not as detailed as MRI, CT scans are faster and widely accessible, making them valuable in emergency situations.
Blood Tests
Blood tests can identify signs of infections, genetic conditions, or electrolyte imbalances that may contribute to seizures. While not used to diagnose epilepsy directly, these tests are important for ruling out other conditions that could mimic epileptic seizures.
Challenges in Diagnosing Epilepsy and the Importance of a Thorough Evaluation
Diagnosing epilepsy can be challenging due to the diverse types of seizures and their varied manifestations. Some seizures might be subtle, while others are unmistakably dramatic. Moreover, other medical conditions can mimic epileptic seizures, leading to misdiagnosis. Hence, a thorough evaluation, including a detailed medical history, physical examination, and appropriate diagnostic tests, is essential. Accurate diagnosis is crucial for effective treatment and management of epilepsy, helping patients achieve better control over their seizures and improving their quality of life.
However, understanding the diagnostic process of epilepsy is the first step toward managing this complex condition. Through comprehensive evaluation and advanced diagnostic tools, healthcare providers can offer targeted treatments that significantly improve patient outcomes.
Epilepsy, a neurological condition characterized by recurrent seizures, affects millions worldwide. Treatment strategies aim to control seizures, minimize side effects, and maintain or improve quality of life. This comprehensive guide explores the various treatment options available, including medication management, surgical interventions, neuromodulation therapies, and dietary approaches.
Medication Management
The cornerstone of epilepsy treatment is medication management, primarily through antiepileptic drugs (AEDs). These medications aim to prevent seizure occurrences without causing significant side effects. Understanding the types of AEDs, customizing treatment plans, and managing potential side effects are crucial steps in effective epilepsy management.
Types of Antiepileptic Drugs (AEDs)
AEDs are categorized based on their mechanism of action. Some common types include sodium channel blockers, GABA enhancers, and calcium channel blockers. Selecting the right AED depends on the type of seizures, the patient’s age, potential side effects, and other health conditions.
Tailoring Medication to the Individual
Personalizing medication plans is vital for effective epilepsy management. Factors such as seizure type, frequency, patient lifestyle, and co-existing health conditions guide the choice of AED. Regular follow-ups are essential to adjust dosages and medications as needed.
Managing Side Effects
While AEDs are effective in controlling seizures, they can cause side effects ranging from mild (dizziness, weight changes) to severe (mood changes, allergic reactions). Monitoring and managing these side effects are paramount to maintaining patient well-being.
Surgical Interventions
Surgery is considered when AEDs fail to control seizures, known as drug-resistant epilepsy. Surgical options vary based on the type of epilepsy and the area of the brain involved.
When Surgery is Considered
Epilepsy surgery is an option for individuals with focal seizures that originate in a specific part of the brain that can be safely removed without significant impact on function.
Types of Epilepsy Surgeries
Common surgical procedures include resective surgery, which involves removing the seizure-generating brain area, and disconnective surgery, which prevents seizure spread by severing neural connections.
Outcomes and Risks
Surgery can significantly reduce or even stop seizures for many patients. However, potential risks include changes in cognition, mood, and neurological function, underscoring the need for thorough pre-surgical evaluation and post-operative care.
Neuromodulation Therapies
Neuromodulation therapies offer alternative treatment options for drug-resistant epilepsy. These involve using devices to alter neuronal activity and reduce seizure frequency.
Vagus Nerve Stimulation (VNS)
VNS involves implanting a device that sends mild electrical pulses to the brain through the vagus nerve. It’s used for individuals who don’t respond well to AEDs or are not candidates for surgery.
Responsive Neurostimulation (RNS)
RNS devices monitor brain activity and deliver electrical stimulation to specific areas when a seizure is detected, aiming to stop it before symptoms occur.
Deep Brain Stimulation (DBS)
DBS targets deep brain structures with electrical impulses to modulate the networks involved in seizure generation. It’s considered for severe, drug-resistant cases.
Dietary Therapies
Dietary approaches can complement other treatments, especially in children. These diets are often used when AEDs are ineffective or cause intolerable side effects.
Ketogenic Diet
This high-fat, low-carbohydrate diet alters the energy metabolism in the brain, which can help control seizures.
Modified Atkins Diet
Similar to the ketogenic diet but less restrictive, the Modified Atkins Diet allows for more proteins and is easier to follow.
Low Glycemic Index Treatment
This diet focuses on foods with a low glycemic index to control blood sugar levels, which can help manage seizures in some individuals.
However, treating epilepsy is a multifaceted approach that requires a personalized strategy. By understanding the various options available and working closely with healthcare professionals, individuals with epilepsy can find the most effective treatment plan to manage their condition.
Living with Epilepsy
Living with epilepsy involves adapting various aspects of daily life to manage the condition effectively. Understanding how to navigate life with epilepsy can empower individuals to lead fulfilling lives despite the challenges. This guide explores lifestyle adjustments, coping strategies, the importance of support groups and counseling, and managing epilepsy across different life stages.
Lifestyle Adjustments and Coping Strategies
Living with epilepsy requires making certain lifestyle adjustments to minimize the frequency and severity of seizures. Key strategies include:
- Adhering to Medication Regimens: Consistently taking prescribed medications is crucial for controlling seizures. It’s important to follow your healthcare provider’s instructions closely and discuss any side effects or concerns.
- Maintaining a Healthy Lifestyle: A balanced diet, regular exercise, and adequate sleep can help manage epilepsy. Some individuals may find a ketogenic diet beneficial, but it should only be followed under medical supervision.
- Avoiding Triggers: Identifying and avoiding known seizure triggers, such as flashing lights, stress, or lack of sleep, can help reduce the occurrence of seizures.
- Stress Management: Techniques such as meditation, yoga, and deep-breathing exercises can help manage stress, which is a common trigger for seizures.
The Role of Support Groups and Counseling
Support groups and counseling play a pivotal role in managing epilepsy. They offer:
- Emotional Support: Connecting with others who understand the challenges of living with epilepsy can provide emotional support, reduce feelings of isolation, and boost morale.
- Educational Resources: Support groups often provide valuable information about managing epilepsy, including tips on lifestyle adjustments and updates on new treatments.
- Counseling Services: Professional counseling can help individuals cope with the psychological and emotional aspects of epilepsy, including anxiety, depression, and self-esteem issues.
Managing Epilepsy in Different Life Stages
Epilepsy requires tailored management strategies at different stages of life:
- Children: Managing epilepsy in children involves close collaboration with teachers and school staff to ensure a safe learning environment. Educational plans may need to be adjusted to accommodate the child’s needs.
- Adults: Adults with epilepsy may face challenges in the workplace or in managing responsibilities such as driving. It’s important to understand your legal rights and seek accommodations when necessary.
- Elderly: In elderly individuals, managing epilepsy can be complicated by the presence of other health conditions. Adjustments in medication and closer monitoring may be required.
Remember, each person’s experience with epilepsy is unique, and what works for one individual may not work for another. Consulting with healthcare providers to tailor a management plan that suits your specific needs is essential.
Innovations in Epilepsy Treatment: Paving the Way for New Horizons
Epilepsy, a neurological disorder marked by recurrent, unprovoked seizures, has been a focal point of medical research for decades. Recent years have witnessed groundbreaking advancements in the treatment of epilepsy, offering new hope and improved quality of life for individuals living with this challenging condition. This section delves into the latest innovations in epilepsy treatment, including cutting-edge medication, surgical techniques, and promising research directions.
Recent Advancements in Medication and Surgical Techniques
The development of new antiepileptic drugs (AEDs) has significantly broadened the therapeutic arsenal against epilepsy. These medications aim to offer better seizure control, fewer side effects, and improved adherence compared to older treatments. Among the most notable advancements are drugs that target specific subtypes of epileptic seizures, allowing for more personalized and effective treatment plans.
In the realm of surgical interventions, minimally invasive techniques have transformed epilepsy surgery. Procedures such as laser ablation therapy and responsive neurostimulation (RNS) are providing safer and more precise options for patients who do not respond to medication. Laser ablation uses targeted laser energy to remove seizure-causing brain tissue without the need for a large incision, minimizing recovery time and risks associated with traditional brain surgery. RNS, on the other hand, involves implanting a device that monitors brain activity and delivers electrical pulses to interrupt seizures before symptoms occur.
Emerging Therapies and Research Directions
Beyond traditional medications and surgeries, the frontier of epilepsy treatment is expanding into novel territories. Gene therapy, for example, is emerging as a potential avenue for treating genetic forms of epilepsy. This approach aims to correct or modify the genes responsible for seizures, offering a long-term solution rather than merely managing symptoms.
Dietary therapies, while not new, have gained renewed interest for their role in managing epilepsy, especially in children. The ketogenic diet, high in fats and low in carbohydrates, has been shown to significantly reduce seizure frequency in some patients, offering an alternative for those who cannot tolerate medication.
Finally, the exploration of cannabis-derived compounds, such as cannabidiol (CBD), has opened up new therapeutic possibilities. Clinical trials have demonstrated the efficacy of CBD in reducing seizures in certain forms of epilepsy, leading to the approval of the first cannabis-based medication for epilepsy treatment.
The landscape of epilepsy treatment is undergoing a rapid transformation, fueled by relentless innovation and research. From advancements in medication and surgical techniques to the exploration of gene therapy and dietary interventions, these developments are broadening the horizons for effective epilepsy management. As research continues to push the boundaries of what’s possible, the future holds promise for even more revolutionary treatments, ultimately aiming to achieve seizure freedom and enhance the quality of life for individuals with epilepsy.
FAQs: Understanding Epilepsy and Its Treatment
What is epilepsy?
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures. These seizures result from sudden, excessive electrical discharges in a group of brain cells. Different parts of the brain can initiate a seizure, making the symptoms and effects of epilepsy varied among individuals.
Who can develop epilepsy?
Epilepsy does not discriminate. It can affect people of any age, race, or gender. According to the World Health Organization, approximately 50 million people worldwide have epilepsy, making it one of the most common neurological diseases globally.
Can epilepsy be cured?
While there is currently no cure for epilepsy, many treatment options can effectively manage seizures. These treatments include medications, surgical procedures, dietary changes, and nerve stimulation therapies. The effectiveness of treatment varies from person to person; some individuals may achieve complete seizure control with medication, while others may require additional treatments.
Is epilepsy contagious?
No, epilepsy is not contagious. You cannot catch epilepsy from someone else. The causes of epilepsy include genetic factors, brain trauma, stroke, infections, and more, but it is never spread from person to person.
Can people with epilepsy live normal lives?
Absolutely. With proper treatment and management, many people with epilepsy can lead full, productive lives. Adjustments may be necessary to manage the condition, such as taking medication regularly, avoiding potential seizure triggers, and sometimes modifying activities. However, many individuals with epilepsy work, attend school, and participate in a wide range of activities and hobbies.
Are seizures always noticeable?
Seizures can vary greatly in how they manifest. While some seizures are evident due to their physical symptoms (such as convulsions), others can be less noticeable, involving subtle changes in sensation, emotion, or behavior. This variability sometimes leads to underdiagnosis or misdiagnosis of the condition.
Can stress cause epilepsy?
Stress alone does not cause epilepsy. However, for individuals with epilepsy, stress can be a trigger that increases the likelihood of having a seizure. Managing stress through relaxation techniques, exercise, and other methods can be an important part of managing epilepsy.
Is it possible to die from epilepsy?
While most people with epilepsy live a normal life span, the condition does carry an increased risk of mortality compared to the general population. This increased risk is due to several factors, including the severity of seizures, the potential for accidents during seizures, and the small risk of SUDEP (sudden unexpected death in epilepsy). However, with proper management and care, the risks associated with epilepsy can often be significantly reduced.
Conclusion
For individuals living with epilepsy and their families, navigating the journey can be challenging. Yet, the importance of professional guidance cannot be overstated. Healthcare professionals specializing in epilepsy can offer comprehensive evaluations to confirm diagnoses and recommend treatment options that are best suited to each individual’s circumstances. These tailored treatment plans can significantly improve the quality of life for those affected, reducing the frequency and severity of seizures and enabling a more active, fulfilling life.
Moreover, seeking out support extends beyond clinical interventions. Connecting with support groups and networks can provide invaluable emotional and practical support. Sharing experiences with others who understand the realities of living with epilepsy can offer comfort, reduce feelings of isolation, and empower individuals and families to advocate for their needs.
In conclusion, while epilepsy may pose significant challenges, with the right knowledge, support, and professional guidance, individuals living with epilepsy can lead vibrant, active lives. We encourage anyone affected by epilepsy to reach out to healthcare professionals and support networks to gain the assistance and encouragement necessary to navigate this path. Remember, you are not alone, and there are resources and communities ready to support you every step of the way.
References
To ensure the accuracy and reliability of the information we’ve shared regarding epilepsy treatment, we encourage our readers to explore additional resources. Below, you will find a list of reputable sources that can offer further insight into the latest research, treatment options, and support for those affected by epilepsy:
- Epilepsy Foundation – A leading source of information for individuals with epilepsy and their families. The Epilepsy Foundation offers comprehensive resources on treatment options, research updates, and support services. Visit their website for more information: Epilepsy Foundation Official Website.
- Mayo Clinic – Known for its patient care and research, Mayo Clinic provides detailed guides on epilepsy symptoms, causes, and treatment methods. Their website is a valuable resource for understanding the medical perspective on epilepsy: Mayo Clinic Epilepsy Guide.
- National Institute of Neurological Disorders and Stroke (NINDS) – As part of the U.S. National Institutes of Health, NINDS offers extensive research-focused information on neurological disorders, including epilepsy. Find cutting-edge research and treatment advances here: NINDS Epilepsy Information Page.
- World Health Organization (WHO) – The WHO provides global insights into epilepsy, including statistics, treatment strategies worldwide, and public health policies. Their epilepsy section can broaden your understanding of how epilepsy is viewed and treated globally: WHO Epilepsy Fact Sheet.
By consulting these sources, readers can further their understanding of epilepsy, stay informed about the latest treatment options, and find support. Remember, while online resources are valuable for gaining knowledge, consulting with a healthcare professional is crucial for personalized medical advice and treatment planning.