COVID-19 Symptoms: In an era defined by the global spread of novel pathogens, understanding the symptoms and causes of COVID-19 is crucial for public health and individual well-being.
As the world grapples with the ongoing challenges posed by the coronavirus pandemic, it is imperative to disseminate accurate and comprehensive information about this disease, which has affected millions worldwide.
This article aims to provide a detailed overview of the symptoms associated with COVID-19, explore its primary causes, and offer insights into the mechanisms of its transmission, all in an effort to arm the reader with knowledge essential for navigating the current health crisis.
Understanding COVID-19
The novel coronavirus, COVID-19, has undeniably left an indelible mark on global health and the way we perceive pandemics. Originating in late 2019, the virus has since traversed continents, infecting millions and prompting unprecedented public health responses. This article aims to shed light on the origins and transmission mechanisms of COVID-19, enhancing public understanding of this formidable virus.
Brief History and Origin of the Virus
COVID-19, caused by the SARS-CoV-2 virus, was first identified in Wuhan, Hubei Province, China, in December 2019. The virus is believed to have zoonotic origins, meaning it initially transmitted from animals to humans. While the exact source remains under investigation, bats are considered a primary reservoir, with the possibility of intermediate hosts that facilitated its jump to humans. The rapid spread and mutation of the virus underscore its complexity and the challenges in containing it.
How COVID-19 Spreads Among People
COVID-19 primarily spreads through respiratory droplets when an infected person coughs, sneezes, talks, or breathes. These droplets can land in the mouths or noses of people nearby, potentially entering the lungs and leading to infection. The virus can spread from person to person, especially in close contact situations (within about 6 feet). It’s also possible for COVID-19 to be contracted by touching surfaces or objects that have the virus on them and then touching one’s face, although this is not the main way the virus spreads.
Understanding the transmission dynamics of COVID-19 is crucial for implementing effective public health measures. Social distancing, wearing masks, frequent hand washing, and vaccination have emerged as key strategies to mitigate the spread. As the virus continues to evolve, so too does our response, highlighting the importance of staying informed and adaptable.
Early Symptoms of COVID-19
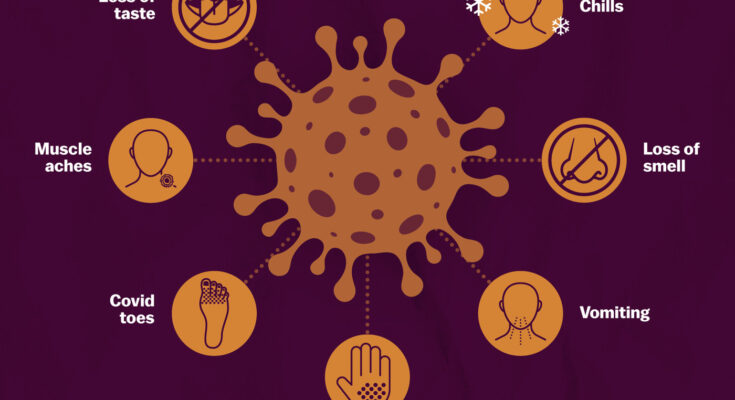
Common early symptoms of COVID-19 include fever, dry cough, tiredness, and loss of taste or smell. Understanding these symptoms can help individuals seek medical advice and testing promptly, reducing the risk of transmission.
Detailed Descriptions of Each Symptom
- Fever: Fever is often one of the first signs of COVID-19. It’s characterized by a body temperature higher than 100.4°F (38°C). Individuals may experience chills, sweating, and a feeling of warmth that fluctuates throughout the day.
- Dry Cough: A persistent dry cough is another hallmark symptom of COVID-19. This cough is usually harsh and does not produce phlegm. It can be irritating to the throat and may lead to a sore throat.
- Tiredness: Many people with COVID-19 report feeling unusually tired or fatigued. This tiredness is not relieved by rest and can significantly impact daily activities. It’s often described as feeling drained or having no energy.
- Loss of Taste or Smell: A sudden loss of taste or smell, without nasal congestion, is a distinctive symptom of COVID-19. This can occur without any other symptoms and may last for several days or weeks.
Comparison of COVID-19 Symptoms with Other Common Illnesses
COVID-19 symptoms can be similar to those of the flu and common cold, which can make it challenging to distinguish between these illnesses without testing. For example, fever, cough, and tiredness are common in both COVID-19 and the flu. However, the loss of taste or smell is more specific to COVID-19 and less common in other respiratory illnesses.
Unlike the common cold, which usually starts with a sore throat or runny nose, COVID-19 symptoms tend to be more severe and can escalate quickly, especially in older adults or individuals with underlying health conditions. The flu shares many symptoms with COVID-19 but differs in the speed of symptom onset and the presence of body aches, which are more pronounced with the flu.
Recognizing these early symptoms and understanding their differences from other common illnesses is crucial for early detection and prevention of COVID-19 spread. If you experience any of these symptoms, especially if they are severe or worsening, it is important to seek medical advice and get tested for COVID-19.
By staying informed about the early symptoms of COVID-19 and how they compare with symptoms of other illnesses, individuals can take proactive steps towards their health and contribute to the safety and well-being of their communities.
Advanced Symptoms of COVID-19
As we continue to navigate through the pandemic, understanding the symptoms of COVID-19 is crucial for ensuring the health and safety of ourselves and others. While many people with COVID-19 experience mild symptoms that can be managed at home, it is vital to recognize when the virus is manifesting in more severe forms that require immediate medical intervention. In this section, we will delve into the advanced symptoms of COVID-19 that should prompt you to seek medical attention without delay.
Difficulty Breathing or Shortness of Breath
One of the hallmark signs that COVID-19 has progressed to a more serious stage is difficulty breathing or experiencing shortness of breath. This symptom is particularly concerning because it indicates that your lungs may not be functioning properly. If you find yourself unable to catch your breath after minimal exertion, or if breathing becomes laborious even when you’re at rest, it’s imperative to contact healthcare services immediately. Difficulty breathing can quickly escalate, necessitating prompt medical evaluation and support.
Chest Pain or Pressure
Another advanced symptom of COVID-19 is persistent chest pain or a sensation of pressure in the chest area. This symptom should never be overlooked, as it could signify a severe complication related to the heart or lungs. Chest pain associated with COVID-19 may feel different from other types of chest pain, such as that caused by heartburn or muscle strain. It is often described as a constant, pressing discomfort that does not improve with rest. If you experience this symptom, it’s crucial to seek medical care immediately to rule out life-threatening conditions like pulmonary embolism or myocarditis.
Loss of Speech or Movement
A less common but equally alarming symptom of advanced COVID-19 is the sudden loss of speech or movement. This could indicate a neurological complication or even a stroke, which are known but rare complications of the virus. The loss of speech might manifest as difficulty forming words, slurred speech, or an inability to speak at all. Similarly, loss of movement could affect any part of the body, rendering it difficult or impossible to move an arm, leg, or even to walk. These symptoms require urgent medical attention to prevent long-term damage and to address the underlying cause effectively.
Early intervention can be lifesaving and can significantly impact the outcome for those suffering from severe forms of COVID-19. Always err on the side of caution and consult with healthcare professionals if you or someone you know exhibits these symptoms. Remember, in the battle against COVID-19, being informed and vigilant is our best defense.
Causes of COVID-19
Understanding the origins and transmission methods of this virus is crucial for preventing its spread and safeguarding public health. This article delves into the causes of COVID-19, exploring how the SARS-CoV-2 virus leads to the disease, the significance of droplets and airborne particles in its transmission, and the role of close contact and contaminated surfaces.
How the SARS-CoV-2 Virus Causes COVID-19
The SARS-CoV-2 virus, belonging to the coronavirus family, is the direct cause of COVID-19. It infects individuals through entry points like the nose, mouth, or eyes, primarily when people inhale respiratory droplets containing the virus. Once inside the body, the virus attaches to cells in the respiratory tract, using its spike proteins to enter and replicate within these cells. This process can lead to symptoms ranging from mild, like cough and fever, to severe illnesses, including pneumonia and acute respiratory distress syndrome.
The Role of Droplets and Airborne Particles in Transmission
Transmission of COVID-19 occurs mainly through respiratory droplets and airborne particles. When an infected person coughs, sneezes, talks, or breathes, they release droplets of various sizes. Larger droplets may fall to the ground quickly, while smaller droplets, or aerosols, can linger in the air for hours, especially in enclosed spaces with poor ventilation. This makes places like indoor restaurants, gyms, and social gatherings particularly high-risk for spreading the virus.
The Impact of Close Contact and Contaminated Surfaces
Close contact with an infected person poses a significant risk for contracting COVID-19. Being within 6 feet of someone who has the virus increases the likelihood of inhaling respiratory droplets or getting these droplets on your skin and subsequently touching your face. Additionally, touching surfaces contaminated with the virus and then touching the face can also lead to infection, although this is not the primary way the virus spreads. Regular handwashing and surface disinfection are key strategies in reducing the risk from contaminated surfaces.
However, COVID-19 is caused by the SARS-CoV-2 virus, which spreads primarily through respiratory droplets and airborne particles. The risk of transmission is heightened by close contact with infected individuals and, to a lesser extent, contact with contaminated surfaces. Understanding these transmission mechanisms is essential for implementing effective prevention and control measures. Stay informed, stay safe, and adhere to public health guidelines to help combat the spread of COVID-19.
Risk Factors for Severe Illness from COVID-19
Navigating the landscape of COVID-19, understanding the risk factors associated with severe illness is crucial. As we delve into the complexities of how age, underlying medical conditions, and lifestyle choices influence COVID-19 severity, it’s important to arm ourselves with knowledge that can guide us towards healthier decisions and better outcomes.
Age and COVID-19 Risks
One of the most significant determinants of COVID-19 severity is age. Studies and data have consistently shown that older adults are at a higher risk for severe illness from COVID-19. The risk increases substantially for those over the age of 60, and even more so for individuals over 80 years old. This heightened risk is due to the natural weakening of the immune system with age, making it harder for the body to fight off infections.
However, it’s important to note that while older adults are at increased risk, younger individuals are not immune to severe outcomes. Cases of serious illness have been reported across all age groups, indicating that while age is a strong factor, it is not the sole determinant of COVID-19 severity.
Underlying Medical Conditions that Increase Severity
Underlying medical conditions play a pivotal role in the severity of COVID-19. Conditions such as heart disease, diabetes, chronic lung disease, cancer, and obesity have been identified as factors that can significantly increase the risk of severe illness from COVID-19. These conditions can compromise the body’s ability to fight off the virus, leading to more severe symptoms and complications.
The presence of multiple underlying conditions further escalates the risk, underscoring the importance of managing these health issues to mitigate COVID-19 severity. It is crucial for individuals with chronic health conditions to follow their healthcare provider’s guidance and take all necessary precautions to protect themselves.
Impact of Lifestyle Choices on COVID-19 Severity
Lifestyle choices, including diet, physical activity, smoking, and alcohol consumption, can also influence the severity of COVID-19. A healthy lifestyle can bolster the immune system and reduce the risk of chronic diseases, thereby potentially decreasing the severity of COVID-19 if infected.
For instance, regular physical activity and a balanced diet rich in fruits, vegetables, and lean proteins can support overall health and immune function. On the other hand, smoking and excessive alcohol consumption can weaken the immune system and exacerbate underlying health conditions, increasing the risk of severe illness from COVID-19.
However, the risk of severe illness from COVID-19 is influenced by a combination of factors, including age, underlying medical conditions, and lifestyle choices. By understanding these risk factors, individuals can take proactive steps to protect themselves and reduce the likelihood of severe outcomes. It’s important to follow public health guidelines, maintain a healthy lifestyle, and consult with healthcare providers to manage health risks effectively.
Preventing COVID-19 Infection: Guidelines and Best Practices
As we continue to navigate the challenges posed by the COVID-19 pandemic, staying informed about the most current prevention guidelines is crucial for safeguarding our health and the well-being of those around us. This article outlines the latest recommendations for preventing COVID-19 infection, emphasizing the importance of hand hygiene and respiratory etiquette.
Current Guidelines on COVID-19 Prevention
1. Vaccination
The foremost step in preventing COVID-19 is to get fully vaccinated, including booster doses as recommended by health authorities. Vaccination significantly reduces the risk of severe illness, hospitalization, and death.
2. Mask-Wearing
In areas with high transmission rates or crowded spaces, wearing masks, especially in indoor settings or when physical distancing cannot be maintained, is advised. Masks should cover both the nose and mouth to be effective.
3. Hand Hygiene
Regular and thorough hand washing with soap and water for at least 20 seconds is essential. If soap and water are not readily available, use a hand sanitizer with at least 60% alcohol. Avoid touching your face, especially your eyes, nose, and mouth, with unwashed hands.
4. Physical Distancing
Maintain at least 6 feet of distance from others who are not from your household, particularly in crowded or poorly ventilated settings.
5. Respiratory Etiquette
Always cover your mouth and nose with a tissue or the inside of your elbow when you cough or sneeze. Dispose of used tissues immediately and wash your hands right after.
6. Avoid Crowded Places
Limit time spent in crowded or indoor environments as much as possible. Opt for outdoor activities where the risk of transmission is lower.
7. Stay Home When Sick
If you feel unwell, exhibit COVID-19 symptoms, or have been in contact with someone who tested positive, stay home and seek medical advice.
8. Regular Cleaning
Frequently clean and disinfect surfaces that are often touched, such as door handles, mobile phones, and keyboards, to reduce the risk of virus transmission.
Importance of Hand Hygiene and Respiratory Etiquette
Hand hygiene and respiratory etiquette are cornerstones in the fight against COVID-19. These practices not only protect you but also reduce the spread of the virus to others. Hand hygiene removes germs and prevents them from entering your body or being passed on to surfaces or individuals. Similarly, practicing good respiratory etiquette by covering coughs and sneezes prevents the projection of virus-laden droplets into the air, where they can be inhaled by others or contaminate surfaces.
However, adhering to the current guidelines for COVID-19 prevention is essential for protecting yourself and others. Vaccination, mask-wearing, hand hygiene, physical distancing, respiratory etiquette, avoiding crowded places, staying home when sick, and regular cleaning are key strategies in mitigating the spread of COVID-19. By incorporating these practices into our daily routines, we can all contribute to a safer and healthier community.
Testing and Diagnosis of COVID-19
Early and accurate testing is crucial for managing and controlling the spread of the virus. This article outlines the testing options for COVID-19 and provides guidance on when and how to seek testing.
List of Testing Options for COVID-19
COVID-19 testing has evolved, offering various methods to determine if you’re currently infected or have been infected in the past. Here are the primary types of tests available:
- PCR Tests: Polymerase Chain Reaction (PCR) tests are considered the gold standard for detecting the presence of SARS-CoV-2, the virus that causes COVID-19. These tests are highly accurate and are performed using a nasal or throat swab. Although they typically require processing in a laboratory, which can take a few days, some rapid PCR tests provide results in as little as a few hours.
- Antigen Tests: Often referred to as rapid tests, antigen tests detect specific proteins from the virus. They are faster, providing results in minutes, but can be less accurate than PCR tests. These tests are also performed using a nasal or throat swab.
- Antibody Tests: Antibody tests, also known as serology tests, help determine if you’ve had a past infection by detecting antibodies to SARS-CoV-2 in your blood. These tests cannot diagnose an active infection but can indicate past exposure to the virus.
When and How to Seek Testing
When to Seek Testing:
- Symptomatic Individuals: If you exhibit symptoms of COVID-19, such as fever, cough, difficulty breathing, or loss of taste or smell, you should seek testing immediately.
- Close Contact: If you’ve been in close contact with someone confirmed to have COVID-19, consider getting tested regardless of symptoms.
- Post-Travel: Testing is recommended after travel, especially if you’ve been to areas with high infection rates.
- Preventative Screening: Regular testing might be advised for people in high-risk settings or those participating in large gatherings.
How to Seek Testing:
- Contact Your Healthcare Provider: Your primary care physician or local healthcare provider can advise on whether you should be tested and where testing is available.
- Local Health Departments: Visit the website or contact your local health department for information on testing locations and requirements.
- Pharmacies and Community Testing Sites: Many pharmacies and dedicated COVID-19 testing sites offer testing by appointment or walk-in. Check online resources or call ahead for information.
- At-Home Testing Kits: At-home test kits are available for purchase online or at pharmacies. Follow the instructions carefully to ensure accurate results.
Testing is a critical tool in the fight against COVID-19. By understanding the types of tests available and knowing when and how to seek testing, you can contribute to your health and the health of your community. Always stay informed about the latest guidelines from health authorities as the situation evolves.
Treatment and Managing Symptoms of COVID-19
As the world continues to navigate the COVID-19 pandemic, understanding the most effective ways to treat and manage symptoms of the virus is crucial for individuals and healthcare providers alike. This article provides an overview of current approaches to treating COVID-19, home care tips for managing mild symptoms, and guidance on when it is necessary to seek hospital care.
Current Approaches to Treating COVID-19
Treatment for COVID-19 varies based on the severity of the symptoms and the health status of the individual. For confirmed cases, healthcare providers are utilizing a combination of supportive care and antiviral or immunomodulating medications to help patients combat the virus. Supportive care may include oxygen therapy and fluid management to relieve symptoms and prevent complications. Antiviral drugs and steroids are used to reduce viral load and inflammation, particularly in more severe cases.
In addition to these treatments, vaccination remains a key preventive measure to protect against COVID-19 and reduce the severity of symptoms should infection occur. Public health agencies worldwide recommend vaccination for all eligible individuals as a critical component of COVID-19 management.
Home Care for Mild Symptoms
Most individuals with COVID-19 experience mild symptoms and can recover at home with appropriate care. If you have been diagnosed with COVID-19 and have mild symptoms, such as fever, cough, or sore throat, it is important to:
- Stay hydrated: Drink plenty of fluids like water, herbal teas, or broth to stay hydrated and help ease symptoms.
- Rest: Adequate rest is vital for recovery, so ensure you’re getting enough sleep and resting when you need to.
- Isolate: To prevent the spread of the virus to others, stay in a separate room from other household members if possible and use a separate bathroom.
- Monitor your symptoms: Keep track of your symptoms, and be alert to any changes or worsening of your condition.
- Practice good hygiene: Regularly wash your hands with soap and water for at least 20 seconds, cover your mouth and nose with your elbow or a tissue when you cough or sneeze, and clean and disinfect frequently touched surfaces daily.
When to Seek Hospital Care
While most cases of COVID-19 can be managed at home, there are certain situations where medical intervention is necessary. Seek immediate hospital care if you or someone you’re caring for experiences:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
These symptoms may indicate a more severe infection or complications requiring advanced medical treatment. Early intervention can be crucial in preventing more serious outcomes.
By following current treatment protocols, taking appropriate measures for home care, and recognizing the signs that indicate a need for hospitalization, individuals can contribute to their own health and safety as well as the wellbeing of their communities. Always consult with healthcare professionals for advice and treatment tailored to your specific condition.
FAQs: Understanding COVID-19 Symptoms and Causes
What are the common symptoms of COVID-19?
COVID-19 symptoms can vary widely among individuals, but the most common signs include fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea. Symptoms may appear 2-14 days after exposure to the virus.
How does COVID-19 spread?
COVID-19 spreads mainly from person to person, primarily through respiratory droplets produced when an infected person coughs, sneezes, or talks. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. Spread is more likely when people are in close contact with one another (within about 6 feet).
Can COVID-19 be transmitted by asymptomatic individuals?
Yes, individuals infected with COVID-19 can transmit the virus to others even if they do not show symptoms (asymptomatic) or before they start showing symptoms (pre-symptomatic). This is why wearing masks, practicing physical distancing, and hand hygiene are essential to controlling the spread.
What are the severe symptoms that require immediate medical attention?
Severe symptoms of COVID-19 that warrant immediate medical attention include trouble breathing, persistent pain or pressure in the chest, new confusion, inability to wake or stay awake, and bluish lips or face. If you or someone you know exhibits these symptoms, seek emergency medical care immediately.
Can COVID-19 cause long-term health effects?
Some individuals who have recovered from COVID-19, referred to as “long-haulers,” experience persistent health problems or long-term effects, including fatigue, shortness of breath, joint pain, chest pain, and cognitive issues like brain fog. These symptoms can last for months after recovering from the acute illness.
How can I protect myself from COVID-19?
To protect yourself from COVID-19, follow these guidelines: get vaccinated and boosted as recommended, wear masks in public settings and when around people who don’t live in your household, maintain at least 6 feet distance from others, avoid crowded places and poorly ventilated spaces, wash your hands often with soap and water for at least 20 seconds or use hand sanitizer with at least 60% alcohol, and clean and disinfect frequently touched surfaces daily.
Can children get COVID-19?
Yes, children can get COVID-19. While children and adolescents are generally at a lower risk of becoming severely ill compared to adults, they can still become infected, show symptoms, and spread the virus to others. Vaccination is recommended for children of eligible age groups to protect against COVID-19.
Conclusion
The significance of staying informed cannot be overstated. With the situation evolving rapidly, accessing and sharing accurate information becomes paramount. It is through our collective efforts in adhering to the guidelines set forth by public health authorities that we can make a difference. These guidelines, including wearing masks, practicing social distancing, and getting vaccinated, are designed to curb the spread of the virus and safeguard public health.
Hence, we call upon each individual to remain vigilant and informed. By doing so, you contribute to a larger community effort to combat COVID-19. Let’s continue to support each other by following public health guidelines, getting vaccinated, and staying informed about the latest developments. Together, we can emerge stronger and more resilient in the face of this global challenge.