Choroid Plexus Carcinoma Treatment: Choroid Plexus Carcinoma (CPC) is a rare and aggressive form of cancer that originates in the choroid plexus, the part of the brain that produces cerebrospinal fluid (CSF).
This fluid is crucial for cushioning the brain and spinal cord, as well as for removing waste products. Given its rarity and severity, understanding the symptoms and causes of Choroid Plexus Carcinoma is paramount for early detection and treatment.
What is Choroid Plexus Carcinoma?
Choroid Plexus Carcinoma (CPC) is a rare and aggressive type of brain cancer that originates in the choroid plexus. The choroid plexus is a network of cells that produce cerebrospinal fluid (CSF), a critical fluid that surrounds and cushions the brain and spinal cord, playing a key role in protecting these vital structures and maintaining the brain’s environment. CPC is most commonly diagnosed in young children and infants, though it can occur at any age.
Statistics on Prevalence and Demographics Affected by CPC
CPC is exceedingly rare, accounting for less than 1% of all brain tumors. The majority of cases are diagnosed in children under the age of 5, with a higher incidence in the first year of life. This rarity means that comprehensive statistics on prevalence are limited, but studies suggest that there is no significant gender bias in CPC occurrence. Due to its aggressive nature, early diagnosis and treatment are crucial to improving outcomes for those affected.
The Role of the Choroid Plexus in the Brain and How CPC Affects It
The choroid plexus plays a fundamental role in the central nervous system by producing cerebrospinal fluid (CSF). This fluid not only cushions the brain, preventing damage from impact, but also delivers nutrients and removes waste from the brain’s environment. CPC disrupts this essential system. The cancerous growth within the choroid plexus can lead to an overproduction of CSF, resulting in hydrocephalus (an accumulation of fluid in the brain), or it can block the flow of CSF, causing increased intracranial pressure. These conditions can result in a variety of symptoms, including headaches, nausea, vomiting, vision problems, and cognitive or developmental delays in children.
CPC’s impact on the brain’s fluid system underscores the importance of the choroid plexus in maintaining cerebral homeostasis and the severe consequences when its function is impaired by cancerous growths. Treatment often involves surgery to remove the tumor, possibly followed by chemotherapy and radiation therapy, especially in cases where complete surgical removal is not possible or if the cancer is particularly aggressive.
Understanding CPC, its rarity, and its impact on the choroid plexus highlights the importance of ongoing research and specialized care to improve diagnosis, treatment, and outcomes for those affected by this challenging condition.
Symptoms and Early Detection of Choroid Plexus Carcinoma
Recognizing the symptoms and understanding the importance of early detection are crucial steps in managing this condition effectively. In this section, we will delve into the common symptoms associated with CPC, emphasize the significance of early detection for effective treatment outcomes, and discuss risk factors along with potential early screening options.
Common Symptoms Associated with Choroid Plexus Carcinoma
The symptoms of Choroid Plexus Carcinoma primarily stem from increased intracranial pressure due to the tumor blocking the flow of cerebrospinal fluid, leading to hydrocephalus. Patients, especially children since CPC more commonly affects the pediatric population, may exhibit several symptoms, including:
- Headaches: Often severe and worsening over time.
- Nausea and Vomiting: Especially in the morning or worsening with head position changes.
- Changes in Vision: Blurred or double vision due to pressure on the optic nerve.
- Balance and Coordination Difficulties: Problems with walking or clumsiness.
- Seizures: In some cases, seizures can occur.
- Cognitive Changes: Including confusion, irritability, or a decline in school performance.
Importance of Early Detection
Early detection of Choroid Plexus Carcinoma is paramount for improving treatment outcomes. The earlier the diagnosis, the more effective the treatment can be, potentially reducing the need for aggressive treatments and minimizing long-term side effects. Early diagnosis allows for timely surgical intervention, which is often the first line of treatment, followed by chemotherapy or radiation therapy, depending on the patient’s age and the tumor’s characteristics.
Risk Factors and Early Screening Options
While the exact cause of CPC is not well understood, and specific risk factors may not be clearly defined, genetic conditions like Li-Fraumeni syndrome have been associated with a higher risk of developing this cancer. For individuals with known genetic predispositions, regular neurological examinations and imaging studies, such as MRI or CT scans, may be recommended as part of an early screening strategy.
Early screening options for those at risk include:
- Neurological Examinations: Regular check-ups with a neurologist to detect any changes in brain function.
- Imaging Studies: MRI or CT scans can detect tumors in the brain, even at an early stage.
- Genetic Counseling: For families with a history of Li-Fraumeni syndrome or other genetic conditions associated with CPC, genetic counseling can provide guidance on risk management and screening.
For individuals with risk factors or genetic predispositions, engaging in early screening programs and maintaining regular communication with healthcare providers is essential for early diagnosis and effective management of this rare condition.
Diagnosing Choroid Plexus Carcinoma
Early and accurate diagnosis is crucial for effective treatment and management of this condition. In this guide, we will explore the various diagnostic procedures used to identify CPC, emphasizing the significance of medical imaging, biomarkers, and genetic testing.
List of Diagnostic Procedures for CPC
The journey to diagnosing CPC involves a series of sophisticated tests and evaluations. Here’s a rundown of the primary diagnostic procedures:
- Neurological Examination: This initial assessment checks for signs of brain or nervous system issues, focusing on motor skills, reflexes, and cognitive functions.
- Magnetic Resonance Imaging (MRI): MRI is pivotal in diagnosing CPC, providing detailed images of the brain’s structure. It helps in pinpointing the location and size of the tumor within the choroid plexus.
- Computed Tomography (CT) Scan: Though less detailed than MRI, CT scans are used to detect abnormalities and assist in the surgical planning process.
- Lumbar Puncture (Spinal Tap): This procedure involves collecting and examining cerebrospinal fluid to detect tumor cells or markers indicative of cancer.
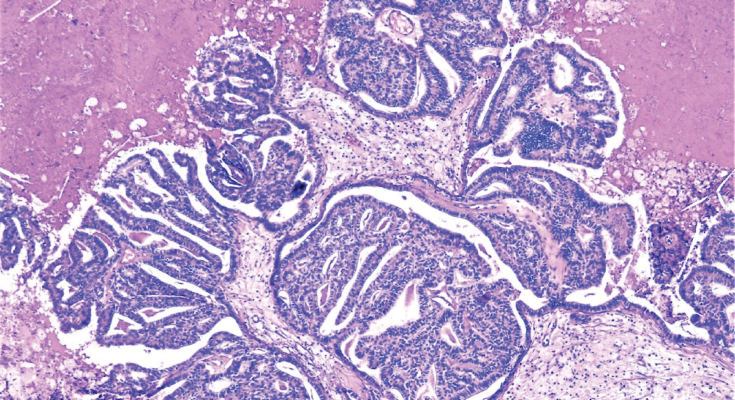
- Biopsy: A definitive diagnosis of CPC requires a biopsy, where a sample of the tumor tissue is removed surgically and examined under a microscope. This helps in determining the malignancy level of the tumor.
The Role of Medical Imaging in Identifying Tumor Characteristics
Medical imaging, especially MRI, plays a critical role in the diagnosis and management of CPC. These imaging techniques offer invaluable insights into the tumor’s characteristics, such as its exact location, size, and the extent of its growth or spread. By providing a clear picture of the tumor’s anatomy, medical imaging facilitates precise surgical planning and helps in evaluating the effectiveness of treatment strategies.
Biomarkers and Genetic Testing as Tools for Diagnosis
Advancements in molecular biology have introduced biomarkers and genetic testing as significant tools in diagnosing CPC. Biomarkers are substances found in the blood, other body fluids, or tissues that can be an indicator of a disease condition. Identifying specific biomarkers related to CPC can help in confirming the diagnosis and assessing the patient’s prognosis.
Genetic testing plays a crucial role in understanding the genetic mutations associated with CPC. It helps in identifying hereditary conditions that may increase the risk of developing CPC, providing crucial information for family members and guiding targeted therapies. Genetic profiling of the tumor can also reveal specific pathways that the cancer exploits to grow, paving the way for personalized treatment approaches.
Treatment Options for Choroid Plexus Carcinoma
Treating CPC can be challenging due to its aggressive nature and the critical area it affects. However, advancements in medical science have paved the way for various treatment options that offer hope and improved outcomes for patients. Here’s a comprehensive guide to understanding the treatment options available for choroid plexus carcinoma.
Surgical Intervention
Surgical removal of the tumor is often the first line of treatment for CPC. The primary goal of surgery is to remove as much of the tumor as possible without compromising the surrounding brain tissue. This approach can alleviate symptoms, reduce tumor burden, and improve the efficacy of subsequent treatments. The complexity of the surgery depends on the tumor’s location and size, and it requires skilled neurosurgeons to perform the procedure. Post-surgery, patients are closely monitored for any signs of recurrence and to manage any potential complications.
Radiation Therapy
Radiation therapy is a treatment option typically considered after surgical intervention, especially if the tumor cannot be entirely removed or if there’s a high risk of recurrence. This therapy uses high-energy rays to target and destroy cancer cells, preventing them from multiplying. For children under three years of age, doctors may try to avoid or delay radiation therapy due to the potential for long-term side effects on the developing brain. However, when necessary, advanced techniques like proton beam therapy are used to minimize exposure to healthy tissues.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells or stop them from growing. It can be administered orally, intravenously, or directly into the cerebrospinal fluid, depending on the case specifics. Chemotherapy is often used in conjunction with surgery and radiation therapy to improve treatment outcomes. It’s particularly useful in managing CPC that has spread or cannot be fully removed surgically. The specific drugs and treatment regimen depend on various factors, including the patient’s overall health and the tumor’s characteristics.
Innovative Treatments and Clinical Trials
The fight against choroid plexus carcinoma is ongoing, and research is continuously uncovering new treatment avenues. Innovative treatments, such as targeted therapy and immunotherapy, are being explored for their potential to more precisely attack cancer cells while sparing healthy tissue. Additionally, clinical trials play a crucial role in advancing CPC treatment. These trials test new drugs, treatment strategies, and technologies that could offer better results with fewer side effects. Patients interested in participating in clinical trials should discuss this option with their healthcare team to understand the potential benefits and risks.
However, the treatment of choroid plexus carcinoma requires a multifaceted approach tailored to the individual’s specific condition. Collaboration among a team of specialists, including neurosurgeons, oncologists, and radiologists, is essential to devising an effective treatment plan. With ongoing research and the development of new treatment modalities, the outlook for CPC patients continues to improve. It’s crucial for patients and their families to discuss all available options with their medical team to make informed decisions about their care.
Challenges in Choroid Plexus Carcinoma Treatment
Treating Choroid Plexus Carcinoma (CPC) presents a unique set of complexities and challenges that require a nuanced understanding of the condition and a collaborative approach to care. This rare and aggressive brain tumor, typically found in children, demands a highly specialized treatment strategy that addresses both the immediate concerns of tumor removal and the long-term considerations of neurological development and quality of life.
Understanding the Complexities
CPC’s rarity contributes to the first layer of complexity in its treatment. The limited number of cases means there is less collective experience and fewer established protocols to guide treatment decisions. Moreover, the tumor’s aggressive nature and potential for rapid growth add urgency to the treatment process, complicating decision-making and often necessitating immediate intervention.
The anatomical location of CPC in the choroid plexus, an area of the brain responsible for producing cerebrospinal fluid, introduces additional challenges. Surgical removal, the primary treatment option, is fraught with risks, including potential damage to surrounding brain tissue and the delicate balance of cerebrospinal fluid production. These risks underscore the need for surgical precision and expertise.
Chemotherapy and radiation therapy, while effective in reducing tumor size or managing residual disease, carry their own set of complications. In pediatric patients, these treatments can have profound long-term effects on cognitive and physical development, necessitating a careful balancing act between effectively treating the tumor and preserving quality of life.
The Importance of a Multidisciplinary Approach
Given the complexities involved in CPC treatment, a multidisciplinary approach is not just beneficial; it’s essential. This approach brings together specialists from neurosurgery, oncology, radiology, neurology, and pediatric care to collaboratively develop and implement a treatment plan tailored to the individual patient’s needs.
A multidisciplinary team (MDT) can navigate the intricacies of CPC treatment, ensuring that all aspects of the patient’s health are considered. For instance, neurosurgeons bring their expertise in safely removing the tumor, while oncologists determine the most effective, least harmful chemotherapy and radiation therapy protocols. Pediatric specialists play a crucial role in monitoring development and implementing strategies to support cognitive and physical growth post-treatment.
Moreover, this collaborative approach facilitates innovative thinking and problem-solving, which are crucial in treating rare and complex conditions like CPC. It allows for the sharing of insights and experiences, potentially leading to more effective and personalized treatment strategies.
The treatment of Choroid Plexus Carcinoma is fraught with challenges, from its rarity and aggressive nature to the potential impacts on a patient’s development and quality of life. Addressing these challenges requires a deep understanding of the condition and a committed, multidisciplinary team capable of providing comprehensive and compassionate care. Through collaboration and expertise, it’s possible to navigate the complexities of CPC treatment, offering hope and improved outcomes for those affected by this daunting condition.
Recovery and Post-treatment Care of Choroid Plexus Carcinoma
The journey doesn’t end with surgery; recovery and post-treatment care are crucial for enhancing quality of life and managing long-term effects. This article explores essential aspects of post-surgery care, the potential long-term impacts of treatment, and the support resources available for patients and their families.
Post-Surgery Care and Monitoring
After the surgical removal of a Choroid Plexus Carcinoma, patients will require careful monitoring to manage immediate postoperative needs and detect any signs of recurrence. Recovery in the hospital involves regular neurological assessments, pain management, and possibly physical therapy to aid in regaining strength and mobility. Once discharged, follow-up appointments are critical. These appointments often include MRI scans every few months for the first year, then less frequently depending on the patient’s condition. Rehabilitation services, including occupational therapy, physical therapy, and speech therapy, may be recommended to address specific needs arising from surgery.
Long-term Effects of Treatment and Quality of Life Considerations
The treatment for CPC, including surgery, chemotherapy, and radiation, can have long-term effects on patients. These may include neurocognitive challenges, physical disabilities, and emotional difficulties. It’s important for survivors and their families to be aware of and prepared for these potential outcomes. Quality of life considerations are paramount, with emphasis on holistic care that addresses physical, emotional, and social health. Regular assessments with healthcare providers can help manage any long-term effects of treatment. Participation in cognitive rehabilitation programs and support groups can also play a significant role in improving the quality of life.
Support Resources for Patients and Families
Navigating the journey of CPC recovery requires a robust support system. Various resources are available to assist patients and their families, including:
- Patient Advocacy Groups: Organizations such as the Brain Tumor Network offer guidance, information, and support to those affected by brain tumors.
- Online Forums and Communities: These platforms allow patients and families to connect, share experiences, and provide mutual support.
- Financial Assistance Programs: The cost of cancer treatment can be overwhelming. Many organizations offer financial aid to help cover the costs of treatment, medication, and related expenses.
- Counseling and Mental Health Services: Professional counseling can help patients and family members cope with the emotional challenges of a cancer diagnosis and treatment.
However, the recovery and post-treatment care of Choroid Plexus Carcinoma encompass a wide range of considerations. From diligent post-surgery monitoring and managing the long-term effects of treatment to leveraging support resources, it’s about fostering resilience and improving the quality of life for patients and their families. With the right care and support, individuals affected by CPC can navigate the challenges of recovery and embrace life beyond cancer.
The Future of Choroid Plexus Carcinoma Treatment
The landscape of Choroid Plexus Carcinoma (CPC) treatment is poised for transformation, fueled by groundbreaking advances in medical research. As we delve into the future of CPC treatment, it’s essential to understand the potential impact of these scientific developments and the critical role of funding and awareness in combating this rare form of cancer.
Advances in Medical Research and Their Potential Impact on CPC Treatment
Recent years have seen remarkable progress in the understanding of Choroid Plexus Carcinoma, a rare and aggressive brain tumor primarily affecting children. Cutting-edge technologies in genomics and molecular biology are at the forefront of this progress, offering new insights into the genetic and molecular mechanisms driving CPC. These advancements hold the promise of personalized medicine, where treatments are tailored to the unique genetic makeup of a patient’s tumor, potentially improving outcomes while minimizing side effects.
Innovative treatment modalities, such as targeted therapy and immunotherapy, are emerging as potential game-changers in the fight against CPC. Targeted therapy aims to attack specific cancer cells based on their genetic characteristics, sparing normal cells and reducing collateral damage. Immunotherapy, on the other hand, harnesses the patient’s immune system to recognize and destroy cancer cells, offering a novel approach to cancer treatment that could be particularly beneficial for CPC patients.
The development of these therapies, however, hinges on the continuous advancement of medical research. Each breakthrough brings us a step closer to more effective and less invasive treatment options, highlighting the importance of sustained investment in CPC research.
The Importance of Funding and Awareness for Rare Cancers Like CPC
Despite the potential of recent scientific advances, the progress in CPC treatment is significantly hampered by a lack of funding and awareness. Rare cancers like CPC often fall into the shadows of more prevalent cancers, struggling to attract the attention of the public and funding bodies. This disparity in resources can slow the pace of research and delay the development of new treatments.
Raising awareness about CPC is crucial for bridging this gap. Increased public understanding can drive fundraising efforts, support advocacy for research funding, and highlight the importance of early detection and treatment. Moreover, fostering a community of support for patients and families affected by CPC can improve quality of life and outcomes.
The future of Choroid Plexus Carcinoma treatment is bright, with scientific advances paving the way for innovative therapies that could revolutionize care for patients. However, realizing this future requires a concerted effort to increase funding and awareness for CPC and other rare cancers. By investing in research and fostering a supportive community, we can unlock new possibilities in the fight against this challenging disease, offering hope to patients and their families.
Conclusion
In closing, while the journey with choroid plexus carcinoma can be daunting, the collective efforts of the medical community, researchers, patients, and their families pave the way toward a brighter future.
Encouraging conversations about CPC, supporting research, and ensuring patients receive personalized, compassionate care are essential steps in this journey. Together, we can make a difference in the lives of those touched by this challenging condition.