Calciphylaxis Symptoms: Calciphylaxis, a rare and serious condition, often associated with chronic kidney disease, is characterized by calcification of blood vessels, leading to ischemic skin lesions and severe pain.
This article delves into the symptoms and causes of Calciphylaxis, aiming to provide a comprehensive understanding of this complex condition.
What is Calciphylaxis?
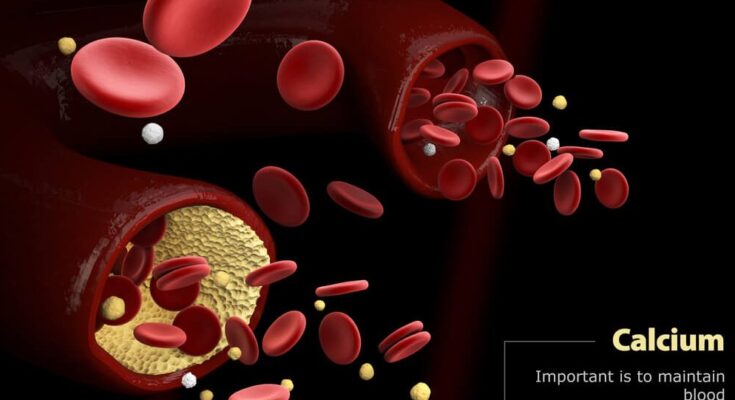
Calciphylaxis, a rare yet serious condition, primarily affects individuals with chronic kidney disease, particularly those undergoing dialysis. This condition, characterized by calcium accumulation in small blood vessels, leads to blood clotting and vessel narrowing. As a result, blood flow is restricted, especially to the skin and fat tissues, causing painful skin ulcers and, in severe cases, leading to infections or tissue death.
Rarity and Seriousness of Calciphylaxis
Calciphylaxis is an extremely rare disorder, affecting a small percentage of individuals, primarily those with end-stage renal disease (ESRD). Despite its rarity, its impact is profound, marked by a high mortality rate. The seriousness of calciphylaxis cannot be overstated, as it often leads to severe complications. Prompt diagnosis and treatment are crucial due to its rapid progression and potentially life-threatening nature.
Demographics Most Commonly Affected by Calciphylaxis
The demographic most commonly affected by calciphylaxis includes middle-aged adults, with a higher prevalence noted among women. Patients with chronic kidney disease, especially those receiving dialysis, are at a significantly higher risk. Additionally, individuals with certain risk factors such as obesity, diabetes, and a history of blood clotting disorders are more susceptible to developing calciphylaxis. Early recognition and management in these high-risk groups are vital for improving outcomes.
Symptoms of Calciphylaxis
Understanding these symptoms is crucial for early detection and effective management. In this detailed exploration, we’ll delve into the primary symptoms of calciphylaxis, providing insights into how these symptoms develop and progress.
Primary Symptoms of Calciphylaxis
- Skin Lesions: The hallmark of calciphylaxis is painful skin lesions. These lesions typically start as small, purplish spots on the skin, often mistaken for bruises or rashes. As the condition progresses, these spots can evolve into larger, ulcer-like wounds that are extremely painful and may have a black or necrotic appearance.
- Severe Pain: Individuals with calciphylaxis often experience significant pain, especially around the affected skin areas. This pain can be persistent and debilitating, affecting the quality of life.
- Skin Hardening: The skin around the lesions may become hard and tender. This is due to the calcification of blood vessels beneath the skin, which leads to reduced blood flow and skin hardening.
- Infection Risk: Open wounds and ulcers associated with calciphylaxis are highly susceptible to infections. Infections can further exacerbate the condition and lead to more serious health complications.
Progression of Symptoms
- Early Stages: Initially, symptoms may be mild, with small, discolored areas on the skin, often accompanied by mild pain or tenderness.
- Intermediate Stages: As the condition progresses, these areas can enlarge, and the pain intensifies. The skin becomes more hardened and may feel warmer or cooler to the touch.
- Advanced Stages: In severe cases, the skin lesions can develop into deep ulcers, exposing the individual to a high risk of infections. The pain becomes more pronounced, and the affected areas can show significant tissue damage.
Importance of Early Detection
Early detection and treatment of calciphylaxis are vital. If you notice any of the symptoms mentioned above, especially if you have risk factors like kidney disease or hyperparathyroidism, seek medical attention immediately. Early intervention can prevent the progression of symptoms and reduce the risk of complications.
Calciphylaxis is a condition with serious implications. Recognizing the symptoms early and understanding their progression is key to managing this condition effectively. Always consult healthcare professionals if you suspect calciphylaxis or experience any related symptoms.
Causes of Calciphylaxis: A Comprehensive Analysis
Our comprehensive analysis delves into the underlying causes and risk factors, offering vital insights for both medical professionals and those seeking to understand this challenging condition.
Primary Causes of Calciphylaxis
- Kidney Disease and Dialysis: Chronic kidney disease, especially in stages requiring dialysis, is a primary risk factor for calciphylaxis. The impaired kidney function leads to mineral imbalances, particularly in calcium and phosphate, which are central to the development of this condition.
- Mineral Imbalance: The disturbed balance of calcium and phosphate in the body plays a crucial role. Elevated phosphate levels, along with increased calcium-phosphate product, contribute significantly to the calcification of blood vessels, a hallmark of calciphylaxis.
- Parathyroid Hormone Levels: Abnormal parathyroid hormone (PTH) levels, often seen in kidney disease, can exacerbate mineral imbalance, further contributing to the risk of calciphylaxis.
Contributing Risk Factors
- Obesity: Individuals with obesity are at a heightened risk. Excess adipose tissue may lead to increased inflammation and changes in blood flow, which can predispose to calciphylaxis.
- Medications: Certain medications, including warfarin, systemic corticosteroids, and calcium-based phosphate binders, have been linked to the development of calciphylaxis. Their role in altering mineral metabolism or blood coagulation may contribute to this risk.
- Gender and Age: Females and older adults are more frequently affected by calciphylaxis. The reasons for these demographic patterns are not entirely clear but may relate to differences in body composition, hormonal factors, and co-morbidities.
Secondary Factors
- Inflammation and Autoimmune Conditions: Chronic inflammation and autoimmune disorders can indirectly increase the risk of calciphylaxis. These conditions may disrupt normal tissue repair and vascular health.
- Genetic Predisposition: While not fully understood, there may be a genetic component that predisposes individuals to calciphylaxis, particularly in non-uremic cases.
Calciphylaxis is a multifaceted condition influenced by a range of factors, from kidney health and mineral imbalances to lifestyle and genetic predispositions. Understanding these causes is crucial for early identification and effective management of this serious condition. This insight not only aids in better patient care but also paves the way for future research in prevention and treatment strategies.
Diagnosing Calciphylaxis: Understanding the Methods and Importance of Early Detection
Calciphylaxis, a rare but serious condition often associated with patients suffering from chronic kidney disease, requires prompt and accurate diagnosis for effective management. Understanding the methodology behind its diagnosis is crucial for healthcare professionals and patients alike.
The Crucial Role of Symptom Recognition in Early Diagnosis
Early detection of calciphylaxis significantly enhances the chances of successful treatment. This begins with the recognition of its symptoms. Commonly, patients exhibit painful, purplish skin lesions that may progress to non-healing ulcers. Healthcare professionals must be vigilant for these signs, especially in high-risk groups like those with end-stage renal disease or on dialysis. Early symptom recognition not only aids in prompt diagnosis but also minimizes the risk of complications, such as infections or skin necrosis.
Comprehensive Diagnostic Methods Beyond Symptom Recognition
While symptom recognition is the first step, diagnosing calciphylaxis extends beyond mere observation. A multifaceted approach is often required:
- Biopsy: A key diagnostic tool is the skin biopsy. By examining tissue samples under a microscope, doctors can identify the characteristic calcification of small blood vessels, confirming the diagnosis of calciphylaxis.
- Blood Tests: These are crucial in identifying abnormalities that may be contributing to calciphylaxis. For instance, elevated levels of parathyroid hormone or abnormalities in calcium and phosphate levels can be indicative.
- Imaging Techniques: Techniques like X-rays, ultrasounds, or CT scans can help in assessing the extent of tissue damage and vascular calcification.
- Differential Diagnosis: It’s vital to differentiate calciphylaxis from other conditions like vasculitis, diabetic ulcers, or warfarin-induced skin necrosis. This ensures accurate treatment and management.
- Collaborative Care: A team approach involving nephrologists, dermatologists, and other specialists is often necessary to accurately diagnose and manage calciphylaxis.
Diagnosing calciphylaxis is a complex process that requires a high degree of suspicion and a comprehensive evaluation strategy. Early symptom recognition plays a pivotal role, but it must be complemented with various diagnostic methods to confirm the presence of this condition. Prompt and accurate diagnosis is the cornerstone of managing calciphylaxis, ultimately improving patient outcomes and quality of life.
Complications Arising from Calciphylaxis
Understanding these complications and their connection to symptoms is crucial for patients and healthcare providers. This section aims to provide a comprehensive overview of the potential complications arising from untreated calciphylaxis and elucidate the relationship between the symptoms and the severity of these complications.
Critical Health Risks Associated with Untreated Calciphylaxis
- Skin and Tissue Damage: The most visible sign of calciphylaxis is the development of painful skin ulcers. Without timely treatment, these ulcers can worsen, leading to extensive tissue damage. This deterioration is not only painful but can also make the skin more susceptible to infections.
- Infections: Open wounds from skin ulcers are a breeding ground for bacteria, increasing the risk of severe infections. These infections can be localized or systemic, potentially leading to life-threatening conditions like sepsis if not promptly addressed.
- Chronic Pain: Individuals with calciphylaxis often experience severe, persistent pain, especially around the ulcerated areas. This pain can be debilitating, impacting the quality of life and leading to additional health complications, such as mental health issues and decreased mobility.
- Impaired Wound Healing: Due to the compromised blood supply in the affected areas, wound healing is significantly slowed down in calciphylaxis patients. This delayed healing process increases the risk of complications, including prolonged pain and the potential for more serious infections.
- Organ Damage: In severe cases, calciphylaxis can lead to calcification in blood vessels beyond the skin, affecting organ function. This can result in complications like heart problems, reduced kidney function, and other critical organ issues.
Link Between Symptoms and Complication Severity
The severity of complications in calciphylaxis is closely linked to the progression and intensity of symptoms. Early symptoms like skin rashes and minor pain, if not treated, can quickly escalate into more severe complications. As the condition advances, the skin lesions deepen, and the risk of infection and organ damage increases. The progression from initial symptoms to severe complications can be rapid, underscoring the importance of early detection and treatment.
However, untreated calciphylaxis can lead to a cascade of severe health issues, from skin and tissue damage to life-threatening infections and organ damage. The progression of symptoms is a key indicator of the severity of complications. Early intervention and continuous management are vital in preventing these serious outcomes and improving the quality of life for those affected by this condition.
Prevention and Management of Calciphylaxis
Understanding its prevention and management is crucial for at-risk populations and healthcare providers. This section provides insights into effective strategies for preventing calciphylaxis and an overview of current management approaches for those already exhibiting symptoms.
Prevention of Calciphylaxis
Identifying and Managing Risk Factors
1. Control of Mineral and Bone Disorder: A key prevention strategy involves managing mineral and bone disorder associated with chronic kidney disease. Regular monitoring and maintaining balanced levels of calcium, phosphorus, and parathyroid hormone (PTH) are critical.
2. Weight Management: Obesity is a known risk factor. Maintaining a healthy weight through diet and exercise can significantly reduce the risk.
3. Medication Review: Certain medications, like warfarin, have been linked to calciphylaxis. Consulting with a healthcare provider to review and potentially modify medication regimens can be a preventive measure.
4. Avoidance of Excessive Calcium and Vitamin D Supplementation: Excessive intake can contribute to the development of calciphylaxis. It’s important to only use these supplements under medical supervision.
Lifestyle Modifications
1. Smoking Cessation: Smoking is a modifiable risk factor, and quitting smoking can reduce the risk of calciphylaxis.
2. Balanced Diet: A diet low in phosphorus and tailored to kidney health can help in preventing calciphylaxis.
Management of Calciphylaxis
Once calciphylaxis symptoms appear, prompt and effective management is crucial.
Medical Treatments
1. Wound Care: Proper care of skin lesions is vital. This includes gentle cleansing, infection prevention, and possibly the use of wound dressings that promote healing.
2. Pain Management: Due to the painful nature of the lesions, effective pain management strategies are essential.
3. Medication Optimization: Adjusting medications to manage calcium, phosphorus, and PTH levels is crucial. Medications like sodium thiosulfate may be used for treatment.
Advanced Treatments
1. Hyperbaric Oxygen Therapy (HBOT): This therapy involves breathing pure oxygen in a pressurized room and has shown promise in the treatment of calciphylaxis.
2. Surgical Interventions: In severe cases, surgical debridement of the affected tissue may be necessary.
Preventing calciphylaxis involves a proactive approach to managing risk factors and making lifestyle modifications. For those with symptoms, a combination of wound care, pain management, medication optimization, and possibly advanced treatments is essential. Regular consultation with healthcare professionals is vital in both preventing and managing this challenging condition.
Understanding the importance of these strategies and implementing them can significantly impact the quality of life for individuals at risk or suffering from calciphylaxis.
FAQ Section: Understanding Calciphylaxis – Symptoms and Causes
1. What is calciphylaxis?
Calciphylaxis, also known as calcific uremic arteriolopathy, is a rare and serious condition characterized by calcium accumulation in small blood vessels, leading to blood clots, skin necrosis, and painful skin ulcers. It primarily affects individuals with kidney disease, especially those on dialysis.
2. What are the main symptoms of calciphylaxis?
The primary symptoms of calciphylaxis include:
- Severe pain in the affected areas.
- Skin lesions or ulcers that may start as small, purple spots and can progress to larger wounds.
- Areas of hardened, discolored skin.
- In severe cases, infection or sepsis due to skin breakdown.
3. Who is at risk for developing calciphylaxis?
Individuals with chronic kidney disease, particularly those undergoing dialysis, are at higher risk. Other risk factors include obesity, diabetes, a history of blood clotting disorders, and an imbalance of minerals such as calcium and phosphate.
4. What causes calciphylaxis?
While the exact cause of calciphylaxis is not fully understood, it is believed to be related to:
- Imbalances in calcium and phosphate levels in the body.
- Chronic inflammation.
- Changes in blood vessels due to chronic kidney disease.
- Use of certain medications, such as blood thinners or steroids.
5. How is calciphylaxis diagnosed?
Diagnosis of calciphylaxis typically involves a combination of medical history review, physical examination, blood tests, and in some cases, a skin biopsy. Imaging studies may also be used to assess blood flow and calcium deposits in tissues.
6. Can calciphylaxis be treated?
Treatment for calciphylaxis is complex and may include:
- Wound care for skin ulcers.
- Medications to control pain and treat infections.
- Adjustments in dialysis treatment.
- Medications to balance calcium and phosphate levels.
- In some cases, surgery may be necessary.
7. Is there a way to prevent calciphylaxis?
Prevention strategies focus on managing risk factors, such as:
- Maintaining a balanced diet to manage mineral levels.
- Regular monitoring and treatment of kidney disease.
- Avoiding medications that may increase the risk.
- Keeping blood pressure and blood sugar levels under control.
8. Where can I find more information about calciphylaxis?
For more information, consult healthcare professionals or visit reputable medical websites. Organizations dedicated to kidney health and research also provide valuable resources about calciphylaxis.
Conclusion
If you or someone you know is experiencing any of the symptoms discussed, it’s imperative to seek medical advice. Remember, while the information provided here is valuable, it is not a substitute for professional medical consultation. A healthcare provider can offer personalized and accurate diagnoses, ensuring that any health concerns are addressed with the most effective and appropriate treatments.
In conclusion, our health is our most valuable asset, and understanding the significance of symptoms and their causes is a powerful tool in our health management arsenal. We encourage everyone to stay informed, remain vigilant about their health, and most importantly, to consult with healthcare professionals when symptoms arise. By doing so, we take an important step towards a healthier, more informed future.