Atrial Fibrillation Treatment: Atrial fibrillation, commonly known as AFib, is an irregular and often rapid heart rhythm condition. This anomaly can lead to a myriad of complications, including stroke and heart failure, significantly impacting the quality of life for those affected.
As the most prevalent type of heart arrhythmia, it’s witnessed in millions globally. It’s not merely the prevalence that’s concerning, but also the potential hazards if left unchecked.
This underscores the immense importance of understanding its diagnosis and treatment. A well-informed approach to AFib can make the difference between leading a normal life or facing serious health setbacks.
In this guide, we will delve deep into AFib, arming you with knowledge to navigate this condition with confidence.
What is Atrial Fibrillation?
This condition can lead to heart-related complications and occurs when the two upper chambers of the heart, known as the atria, beat chaotically and out of sync with the two lower chambers, called the ventricles.
Differences between AFib and Regular Heart Rhythms:
1. Rhythm: While a regular heart rhythm, known as sinus rhythm, showcases a consistent and predictable pattern, AFib results in an erratic and inconsistent heartbeat.
2. Heart Rate: In sinus rhythm, the heart rate typically ranges from 60 to 100 beats per minute. In AFib, however, the rate can exceed 100 beats per minute, leading to a sensation of palpitations.
3. Origination: Regular heart rhythms originate from the sinoatrial (SA) node in a coordinated manner. In contrast, in AFib, the electrical signals become chaotic, emerging from various locations in the atria.
4. Symptoms: While regular heart rhythms might not cause any noticeable symptoms, AFib can lead to feelings of dizziness, shortness of breath, and tiredness.
5. Health Risks: A regular heartbeat ensures optimal blood flow throughout the body. However, AFib can potentially lead to stroke or heart failure due to the irregular circulation and pooling of blood in the heart chambers.
However, understanding the distinction between AFib and regular heart rhythms is essential for prompt diagnosis and treatment. Recognizing the signs of AFib can lead to timely medical intervention, reducing associated risks and improving overall heart health.
Causes and Risk Factors of Atrial Fibrillation (AFib)
The exact causes can be diverse, but understanding the common culprits and risk factors can be pivotal for prevention and management.
Common Causes of AFib:
1. High Blood Pressure: Often cited as the leading cause of AFib, uncontrolled hypertension can damage the heart’s electrical system.
2. Heart-related issues: Conditions like heart valve problems, coronary artery disease, or congenital heart defects can lead to AFib.
3. Thyroid Problems: An overactive or underactive thyroid can prompt AFib.
4. Excessive Alcohol Use: Binge drinking or chronic overconsumption can trigger the condition, sometimes referred to as “holiday heart syndrome.”
5. Other Causes: Sleep apnea, viral infections, and exposure to stimulants like medications, caffeine, or tobacco can also be contributors.
Risk Factors Associated with its Development:
1. Age: The risk increases with age, especially for individuals over 60.
2. Heart Disease: Those with heart conditions, such as heart valve problems or a history of heart attack, are at higher risk.
3. Family History: Genetics can play a role. If a family member has AFib, your risk might be elevated.
4. Chronic Conditions: Diabetes, chronic kidney disease, or metabolic syndrome can enhance the likelihood of developing AFib.
5. Obesity: Being overweight significantly increases the risk.
6. Drinking and Substance Use: Excessive alcohol consumption or drug use can be potential risk factors.
However, understanding the causes and risk factors of AFib is crucial. Regular check-ups, managing existing health conditions, maintaining a balanced lifestyle, and avoiding excessive alcohol or stimulant consumption can aid in minimizing the risk.
Symptoms of Atrial Fibrillation
Let’s dive into the common signs and symptoms of AFib and understand why it’s crucial to recognize them as soon as they arise.
Common Signs and Symptoms
Atrial Fibrillation, often abbreviated as AFib, manifests through various noticeable symptoms. Understanding these symptoms can lead to early detection and management:
1. Irregular Heartbeat: Unlike the rhythmic beating of a healthy heart, those with AFib might experience erratic heart rhythms.
2. Heart Palpitations: This feels like a rapid, fluttering, or pounding heart and is often the most recognized sign of AFib.
3. Fatigue: People with AFib may feel unusually tired, even without exertion.
4. Dizziness: This can be accompanied by a feeling of light-headedness or even fainting spells.
5. Shortness of Breath: Breathing might become difficult, especially after physical activity.
6. Chest Pain or Pressure: Although this isn’t as common, it is a significant symptom that demands immediate medical attention.
The Significance of Recognizing Them Early
Early detection of AFib symptoms is crucial for several reasons:
1. Reduced Complications: Recognizing and treating AFib early can reduce the risk of severe complications like stroke or heart failure.
2. Effective Management: The earlier AFib is detected, the more treatment options are available, leading to better management and outcomes.
3. Prevention of Progression: When caught early, interventions can prevent the condition from worsening or becoming chronic.
4. Improved Quality of Life: Timely diagnosis and treatment can ensure that individuals lead a more comfortable and symptom-free life.
Awareness and understanding of these symptoms can play a pivotal role in the proactive management of AFib, ensuring a healthier and longer life for patients.
Diagnostic Procedures of Atrial Fibrillation
Atrial fibrillation (AFib) is a common heart rhythm disorder that needs precise diagnostic tools to determine its presence and guide treatment. The following are the main diagnostic procedures used to detect AFib:
Electrocardiogram (EKG or ECG)
- What is it? An EKG is a non-invasive test that measures the electrical activity of your heart.
- Why is it used? It can identify irregularities in your heart’s rhythm and structure. If AFib is present, the EKG will show rapid and erratic electrical impulses.
Holter Monitor
- What is it? A portable EKG device worn for 24 to 48 hours, tracking your heart’s activity continuously.
- Why is it used? This is beneficial for detecting AFib episodes that might not occur during a standard EKG, providing a more comprehensive picture of your heart’s activity over a longer period.
Event Recorder
- What is it? A wearable device used to record the heart’s electrical activity over extended periods, sometimes weeks.
- Why is it used? It allows patients to press a button and record their heart rhythm when they feel symptoms. This can help correlate symptoms with heart rhythm irregularities.
Echocardiogram
- What is it? A non-invasive ultrasound test that produces images of the heart’s size, structure, and motion.
- Why is it used? It can reveal any structural heart problems or blood clots and provides insights about the pumping efficiency of the heart.
Blood Tests
- What is it? Laboratory tests using a blood sample.
- Why is it used? Blood tests can rule out thyroid problems or other substances in your blood that might lead to AFib. They also help in assessing any damage to the heart or the presence of other conditions that may require treatment.
Each of these diagnostic procedures plays a crucial role in detecting and managing atrial fibrillation. If you suspect you have AFib, it’s essential to see a healthcare provider who can recommend the appropriate tests.
Importance of Accurate Atrial Fibrillation Diagnosis
Delving into the significance of this matter, let’s explore the potential risks associated with untreated or undiagnosed AFib and how a proper diagnosis can shape effective treatment strategies.
Potential Risks of Untreated or Undiagnosed AFib
AFib, when left untreated or undiagnosed, can lead to severe health complications. Some of the potential risks include:
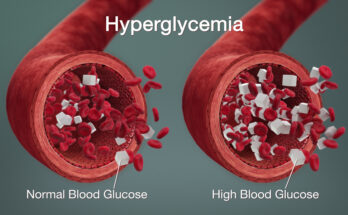
1. Stroke: AFib can cause blood to pool in the heart, leading to the formation of blood clots. If a clot breaks off and travels to the brain, it can cause a stroke. It’s crucial to note that individuals with AFib have a five times higher risk of suffering a stroke than those without the condition.
2. Heart Failure: Over time, the heart can weaken due to the irregular rhythms of AFib, leading to heart failure. This means the heart isn’t pumping blood as effectively as it should.
3. Other Cardiac Issues: Apart from stroke and heart failure, AFib can lead to other cardiac problems, such as chronic fatigue, shortness of breath, and decreased endurance during physical activities.
How a Proper Diagnosis Can Guide Treatment
A timely and accurate diagnosis of AFib provides the foundation for tailored treatment options:
1. Personalized Treatment Plans: With a confirmed diagnosis, doctors can recommend the best treatment strategies suited to an individual’s health needs, whether that be medication, lifestyle changes, or surgical procedures.
2. Reduction of Complications: Early diagnosis and subsequent treatment can significantly reduce the risk of complications, like stroke or heart failure.
3. Improved Quality of Life: Managing AFib symptoms can lead to an improved quality of life. Patients often report better sleep, increased energy levels, and fewer disruptions in their daily activities post-diagnosis and treatment.
However, the importance of an accurate atrial fibrillation diagnosis cannot be overstated. It acts as the cornerstone for effective treatment, potentially averting severe health consequences and paving the way for a healthier, more active life.
Atrial Fibrillation Treatment Options
Thankfully, there are several treatment options available to manage and mitigate its symptoms. Here’s an overview:
1. Medications:
The first line of defense against AFib often involves prescription medications.
- Rate Control Drugs: These help in regulating the heart rate, ensuring it doesn’t beat too quickly.
- Rhythm Control Drugs: These aim to restore the heart’s regular rhythm and prevent future episodes of AFib.
- Blood Thinners: These are anticoagulants designed to prevent blood clots, reducing the risk of stroke which can be a complication of AFib.
2. Non-surgical Procedures:
If medications aren’t effective, non-surgical procedures can be a viable option.
- Cardioversion: This involves using electricity or drugs to reset the heart’s rhythm to its regular state.
- Catheter Ablation: Here, tiny areas of the heart causing the erratic rhythms are scarred or destroyed, helping restore normal heart function.
3. Surgical Procedures:
For persistent cases of AFib, surgical interventions might be considered.
- Maze Procedure: Small cuts are made in the heart’s atria. When these heal, they form scar tissue that prevents the abnormal electrical signals causing AFib.
- Atrioventricular (AV) Node Ablation with Pacemaker Placement: The AV node is destroyed, and a pacemaker is implanted to maintain a regular heart rhythm.
4. Lifestyle Changes to Aid Treatment:
Besides medical interventions, making certain lifestyle adjustments can also help in managing AFib.
Adopting a balanced diet, limiting caffeine and alcohol intake, managing stress, maintaining a healthy weight, and avoiding smoking are all beneficial. Regular check-ups and monitoring can also aid in early detection and management.
However, while AFib can be challenging, various treatment options and lifestyle changes can help patients lead a normal and healthy life. It’s always essential to consult with a healthcare professional about the best treatment pathway tailored to individual needs.
Recent Advances in Atrial Fibrillation Treatment
Here, we’ll explore recent advances and potential future treatments in a concise and reader-friendly manner.
New Drugs and Procedures
Recent years have witnessed the introduction of novel drugs and procedures designed to effectively manage AF. These advancements aim to address the irregular heart rhythms associated with the condition and enhance patients’ overall quality of life. Some key developments include:
1. Novel Anticoagulants: Innovative blood-thinning medications, such as apixaban and dabigatran, have proven to be both safer and more convenient than traditional warfarin. They reduce the risk of stroke in AF patients while minimizing the need for constant monitoring.
2. Catheter Ablation: Radiofrequency and cryoablation procedures have gained prominence for treating AF. These minimally invasive techniques target the areas of the heart responsible for abnormal electrical signals, restoring regular heart rhythm and reducing the need for long-term medication.
3. Left Atrial Appendage Closure: For patients who cannot tolerate anticoagulants, left atrial appendage closure devices like the Watchman implant provide an alternative to prevent stroke by blocking off a potential source of blood clots.
Potential Future Treatments
While current advancements have significantly improved AF management, ongoing research promises even more innovative solutions. Potential future treatments on the horizon include:
1. Gene Therapy:
Researchers are exploring gene-based therapies to address the underlying genetic factors that contribute to AF. This personalized approach may pave the way for more effective and targeted treatment options.
2. Artificial Intelligence (AI):
AI-driven algorithms are being developed to better predict AF episodes and optimize treatment plans. These technologies have the potential to enhance AF management by tailoring therapies to individual patient needs.
3. Electroceuticals:
Emerging technologies like neuromodulation devices aim to control heart rhythm through electrical stimulation. These devices may offer a promising avenue for managing AF without the need for medications or invasive procedures.
However, the field of atrial fibrillation treatment is rapidly evolving, offering patients a range of new drugs, procedures, and exciting prospects for the future. These advancements promise to not only enhance the quality of life for AF patients but also provide more effective, personalized, and less invasive options for managing this common cardiac condition. Stay tuned for further breakthroughs in AF treatment as research continues to progress.
Living with Atrial Fibrillation
Here, we’ll explore essential aspects of living with AFib, from daily life adjustments to the importance of routine check-ups and patient education.
Daily Life Adjustments
1. Diet and Nutrition: Maintaining a heart-healthy diet is crucial for AFib patients. Focus on consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Reducing sodium intake can help manage blood pressure, which is often linked to AFib.
2. Physical Activity: Regular exercise is beneficial, but it’s important to consult your healthcare provider before starting any new exercise routine. They can recommend safe and appropriate activities to help manage AFib and improve overall health.
3. Stress Management: Stress can trigger AFib episodes, so finding effective stress-reduction techniques is essential. Practices like meditation, yoga, and deep breathing exercises can help you relax and manage stress.
4. Medication Adherence: If your doctor prescribes medication, it’s crucial to take it as directed. Skipping doses or discontinuing medication without consulting your healthcare provider can lead to complications.
5. Alcohol and Caffeine: Limiting alcohol and caffeine intake can help control AFib symptoms, as they can act as triggers. Moderation is key, and consulting your doctor for personalized advice is recommended.
The Importance of Routine Check-Ups and Patient Education
1. Regular Monitoring: Routine check-ups with your healthcare provider are essential for monitoring your AFib and adjusting your treatment plan as needed. These visits allow your doctor to assess your heart’s rhythm, discuss any concerns, and make necessary changes to your medication or lifestyle recommendations.
2. Patient Education: Understanding your condition is empowering. Take the time to educate yourself about AFib, its triggers, and the management strategies. Knowledge enables you to actively participate in your care and make informed decisions.
3. Support Networks: Joining support groups or seeking emotional support from friends and family can be valuable. Sharing experiences and advice with others who have AFib can provide emotional relief and practical insights.
However, living with atrial fibrillation requires a holistic approach that encompasses lifestyle adjustments, regular medical check-ups, and patient education. By making these important changes, individuals with AFib can enhance their quality of life and better manage their condition. Remember that consulting your healthcare provider is essential for personalized guidance and treatment.
Conclusion
In conclusion, understanding the significance of prompt diagnosis and selecting the most suitable atrial fibrillation (AFib) treatment is paramount for managing this condition effectively. Recent advances in AFib treatment, including the introduction of new drugs and procedures, offer hope for improved outcomes. Moreover, potential future treatments hold the promise of even better options on the horizon.
It’s crucial to emphasize that if you or someone you know suspects they may have AFib, seeking professional medical advice is imperative. A timely diagnosis and the guidance of a healthcare expert can make a world of difference in managing AFib and enhancing your quality of life.
Don’t hesitate to reach out to a healthcare provider to discuss your concerns and explore the most suitable treatment options for your unique situation. Your well-being is worth the investment in proper care and attention.