Atelectasis Symptoms: Atelectasis, a medical condition often overshadowed by its more notorious counterparts like pneumonia or bronchitis, warrants a closer examination due to its intricate pathology and potential impact on overall health.
This article delves into the depths of atelectasis, explicating its symptoms, causes, and the intricate mechanisms behind its development.
What is Atelectasis?
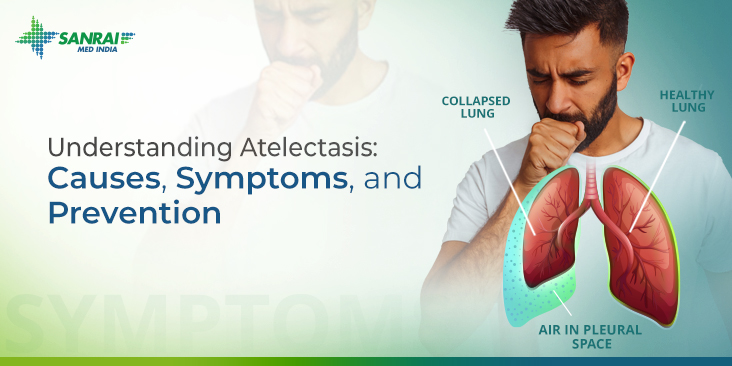
Atelectasis is a lung condition characterized by the partial collapse or incomplete inflation of one or more areas of the lung. This medical issue can result from a variety of causes, ranging from blockages in the airways to pressure from outside the lung. When atelectasis occurs, the affected lung tissue is unable to fully expand, leading to reduced oxygen exchange and potential complications.
Types of Atelectasis
There are several types of atelectasis, each with distinct causes and characteristics:
1. Obstructive Atelectasis: This type occurs when something blocks the airways, such as mucus plugs, foreign bodies, or tumors. The obstruction prevents air from reaching the alveoli, leading to their collapse.
2. Non-Obstructive Atelectasis: This category includes several forms:
- Compression Atelectasis: Caused by external pressure on the lung, such as from a tumor, fluid, or air in the pleural space (the area between the lungs and the chest wall).
- Adhesive Atelectasis: Due to a lack of surfactant, a substance that helps keep the alveoli open. This type is more common in newborns, particularly premature infants.
- Cicatricial Atelectasis: Resulting from scarring or fibrosis in the lung tissue.
- Relaxation Atelectasis: Occurs when there is space around the lung due to a condition like pneumothorax or pleural effusion, leading to lung collapse.
Understanding the specific type of atelectasis is crucial for effective treatment, which may involve addressing the underlying cause, respiratory therapy, medications, or in some cases, surgery. Early diagnosis and intervention can significantly improve outcomes and reduce complications associated with this condition.
Symptoms of Atelectasis: A Comprehensive Guide
These symptoms is crucial for early detection and effective treatment. This article provides a detailed exploration of the common symptoms associated with atelectasis, and how they differ from other respiratory conditions.
Common Symptoms of Atelectasis
- Shortness of Breath: Often the first and most noticeable symptom. Patients may feel unable to breathe deeply or catch their breath.
- Rapid, Shallow Breathing: Due to the reduced lung capacity, breathing may become faster and shallower than normal.
- Coughing: A persistent cough is common, but it may not be productive, meaning it typically does not bring up mucus.
- Chest Pain or Discomfort: Patients may experience a sharp or aching pain on the affected side of the chest, which may worsen with deep breaths.
- Low Oxygen Levels: In severe cases, the reduction in lung function can lead to decreased oxygen levels in the blood, resulting in symptoms like cyanosis (bluish skin tone).
Differentiating Atelectasis from Other Respiratory Conditions
While some symptoms of atelectasis overlap with other respiratory issues, certain aspects help differentiate it:
- Onset and Duration: Symptoms of atelectasis often develop quickly, particularly after surgery or a chest injury. This sudden onset differs from conditions like chronic obstructive pulmonary disease (COPD), where symptoms develop gradually.
- Type of Cough: Unlike conditions like bronchitis or pneumonia, the cough associated with atelectasis is usually dry and non-productive.
- Breathing Pattern: Rapid, shallow breathing is more characteristic of atelectasis, as opposed to the prolonged expiratory phase seen in conditions like asthma.
- Chest Pain: The localized pain in atelectasis is distinct from the diffuse chest discomfort seen in diseases like pneumonia.
- Response to Treatment: Atelectasis may improve with certain maneuvers like deep breathing exercises, which are less effective in conditions like asthma or COPD.
Recognizing these differences is key for healthcare providers to diagnose and manage atelectasis effectively. If you experience any of these symptoms, especially after surgery or a chest injury, consult a healthcare professional for a proper evaluation and treatment plan.
Causes of Atelectasis
Understanding these causes is crucial for both prevention and treatment. In this section, we’ll delve into the common causes of atelectasis and explain how they lead to this lung condition.
1. Airway Obstruction
Airway obstruction is a primary cause of atelectasis. Obstructions can occur due to:
- Inhaled foreign bodies: Small objects inhaled into the airways can block airflow.
- Mucus plugs: Accumulation of mucus, often in patients with respiratory conditions, can obstruct airways.
- Tumor growth: Tumors in the airways can impede the flow of air.
When an airway is blocked, the air distal to the blockage is absorbed by the blood, causing the lung tissue to collapse.
2. Compression
Compression atelectasis happens when something outside the lung exerts pressure on it, such as:
- Pleural effusion: Fluid accumulation between the lung and chest wall.
- Pneumothorax: Air in the pleural space exerting pressure on the lung.
- Tumor or enlarged heart: These can compress the lung from the outside.
This external pressure prevents the lung from fully expanding, leading to atelectasis.
3. Postoperative Atelectasis
Postoperative atelectasis is common after surgery, especially chest or abdominal surgery. Causes include:
- Anesthesia: It can reduce normal lung expansion, leading to areas of collapse.
- Pain: Post-surgical pain can lead to shallow breathing, which doesn’t fully inflate the lungs.
4. Sedentary Lifestyle
Prolonged bed rest or limited mobility can lead to atelectasis because of:
- Inadequate lung expansion: Without regular movement or deep breathing, the lungs may not expand fully.
- Mucus accumulation: Reduced movement can lead to mucus buildup, causing blockages.
5. Lung Diseases
Certain lung diseases, such as asthma or cystic fibrosis, can increase the risk of atelectasis due to:
- Chronic mucus production: This can lead to blockages in the airways.
- Inflammation and scarring: These can restrict airway patency and lung expansion.
Understanding these causes and how they contribute to atelectasis is vital for effective management and treatment of this condition. Early recognition and intervention can significantly improve outcomes for patients suffering from atelectasis.
Diagnosis of Atelectasis
Diagnosing atelectasis accurately is crucial for effective treatment and management. This section provides a comprehensive overview of the methods used for diagnosing atelectasis, emphasizing the role of symptoms in its identification.
Methods Used for Diagnosing Atelectasis
- Chest X-ray: The most common and initial diagnostic tool for atelectasis. It helps in identifying areas of lung collapse.
- Computed Tomography (CT) Scan: Offers a more detailed image of the lungs than a chest X-ray, allowing for a clearer view of the collapsed areas.
- Bronchoscopy: Used to view the airways and check for blockages that might lead to atelectasis.
- Pulmonary Function Tests (PFTs): Assess lung function and help in determining the impact of atelectasis on lung capacity.
- Oximetry or Blood Gas Analysis: Measures the oxygen levels in the blood, which can be affected by atelectasis.
- Ultrasound: Sometimes used to diagnose atelectasis, especially in patients where radiation exposure is a concern.
The Role of Symptoms in Diagnosing Atelectasis
Recognizing the symptoms of atelectasis plays a pivotal role in its diagnosis:
- Breathlessness: Difficulty in breathing or shortness of breath can indicate atelectasis, especially if it occurs suddenly.
- Cough: A persistent cough may be a sign of atelectasis.
- Chest Pain: Pain or discomfort in the chest area, particularly when breathing in, can be associated with atelectasis.
- Fever: In some cases, atelectasis can lead to fever, especially if it results in infection.
It is important to note that atelectasis can sometimes be asymptomatic, particularly in smaller cases. Therefore, regular medical check-ups and attention to lung health are essential, especially for individuals at higher risk, such as those undergoing surgery or with lung diseases.
Timely and accurate diagnosis of atelectasis is vital for effective treatment. By combining various diagnostic methods and paying close attention to symptoms, healthcare professionals can identify and manage this condition effectively. Patients experiencing symptoms indicative of lung issues should seek medical advice promptly for a thorough evaluation.
Complications Associated with Atelectasis
Let’s delves into the potential risks associated with untreated atelectasis and underscores the importance of timely medical intervention.
Potential Complications of Untreated Atelectasis
- Infection: A major concern with atelectasis is the risk of developing infections. When the lung collapses, it creates an environment conducive to bacterial growth, leading to conditions such as pneumonia, a serious lung infection that can further complicate the patient’s health.
- Respiratory Failure: Atelectasis can progress to respiratory failure if a significant portion of the lung is affected. This critical condition occurs when the lungs cannot supply enough oxygen to the body or remove carbon dioxide effectively, necessitating urgent medical care.
Importance of Timely Medical Intervention
Timely medical intervention is crucial in managing atelectasis. Early diagnosis and treatment can prevent the progression of the condition, reducing the risk of severe complications. Treatment strategies may include:
- Physical Therapy: Techniques like chest physiotherapy can help expand the lungs and clear mucus, which is essential in preventing infections.
- Breathing Exercises: Simple exercises can significantly improve lung function and prevent the recurrence of atelectasis.
- Medical Procedures: In some cases, medical procedures may be necessary to re-expand the collapsed lung tissue.
However, understanding the complications associated with atelectasis and the importance of prompt medical attention cannot be overstated. Patients experiencing symptoms should seek medical advice without delay to mitigate risks and ensure effective treatment.
Treatment and Management of Atelectasis: An In-depth Guide
Let’s delves into the various treatment options and lifestyle changes that can effectively manage and treat atelectasis.
Treatment Options for Atelectasis
1. Physical Therapy: One of the primary treatment approaches for atelectasis includes respiratory therapies, such as:
- Chest Physiotherapy: Techniques like percussion and vibration help loosen mucus in the lungs.
- Deep Breathing Exercises: Encouraging deep breaths through incentive spirometry aids in expanding the lungs.
2. Bronchoscopy: This procedure is essential for:
- Clearing Obstructions: A bronchoscope can remove mucus plugs or foreign objects causing lung collapse.
- Direct Visualization: It allows doctors to view the airways and assess the extent of lung collapse.
3. Medications:
- Mucolytics: Medicines that thin mucus, making it easier to cough up.
- Bronchodilators: These drugs help open up the airways, improving airflow.
Lifestyle Changes and Home Remedies
- Smoking Cessation: Smoking can exacerbate lung conditions, so quitting is crucial.
- Increased Fluid Intake: Hydration helps thin mucus, facilitating easier clearance.
- Regular Exercise: Engaging in light exercise improves overall lung function.
- Positional Changes: Changing positions frequently can help improve lung expansion and mucus clearance.
- Controlled Coughing Techniques: Learning effective coughing methods can assist in clearing mucus from the lungs.
Effective management of atelectasis involves a combination of medical treatments and lifestyle adjustments. Regular follow-ups with healthcare providers are essential to monitor progress and make necessary adjustments to the treatment plan. Always consult a medical professional before making significant changes to your health regimen.
Prevention of Atelectasis
This condition can lead to various health complications, especially in high-risk groups such as post-operative patients, individuals with chronic respiratory conditions, or those with limited mobility. Preventing atelectasis is crucial for maintaining optimal lung health and overall well-being.
Tips and Strategies for Prevention
- Deep Breathing Exercises: Regular deep breathing exercises can significantly reduce the risk of atelectasis. These exercises help in expanding the lungs, ensuring that air reaches all parts of the lung tissues.
- Frequent Movement: For individuals with limited mobility, such as bedridden patients or those with sedentary lifestyles, frequent changes in position can help prevent lung collapse. Encouraging movement or providing assistance for mobility can make a substantial difference.
- Use of Incentive Spirometry: Incentive spirometry is a device used to help patients improve the functioning of their lungs. It is particularly useful for patients recovering from surgery or those with lung diseases.
- Pulmonary Rehabilitation: Pulmonary rehabilitation programs that include physical exercises, breathing techniques, and educational information can be highly beneficial for individuals prone to atelectasis.
Role of Regular Medical Check-Ups and Healthy Habits
Regular medical check-ups play a pivotal role in preventing atelectasis. Health professionals can monitor lung function and identify any early signs of lung collapse, enabling timely intervention.
- Healthy Lifestyle: Maintaining a healthy lifestyle that includes regular exercise, a balanced diet, and avoiding smoking can significantly lower the risk of developing atelectasis.
- Post-Operative Care: For individuals who have undergone surgery, especially thoracic or abdominal surgery, following post-operative care instructions is crucial. This includes pain management, deep breathing exercises, and sometimes, the use of a spirometer.
- Early Mobilization: Encouraging early mobilization after surgery or during long hospital stays is essential in preventing the development of atelectasis.
- Avoiding Environmental Pollutants: Exposure to environmental pollutants like smoke, dust, and chemical fumes should be minimized as they can aggravate the lungs and increase the risk of lung collapse.
Preventing atelectasis involves a combination of lifestyle changes, regular medical check-ups, and specific strategies for high-risk groups. By adopting these measures, individuals can significantly reduce their risk of developing this lung condition, leading to better respiratory health and overall quality of life.
FAQs on Atelectasis: Symptoms and Causes
1. What is Atelectasis?
Atelectasis is a condition where a part or the whole of a lung collapses, preventing normal oxygen absorption to healthy tissues. It can occur for various reasons, including blockages in the airways or pressure from outside the lung.
2. What are the most common symptoms of Atelectasis?
Symptoms of atelectasis can vary depending on its severity and cause. Common symptoms include difficulty breathing, rapid shallow breathing, coughing, and a bluish skin color due to lack of oxygen. In some cases, there may be no noticeable symptoms, especially in small-scale lung collapses.
3. How does Atelectasis occur?
Atelectasis can occur due to several factors. Blockage of airways by mucus, foreign bodies, or tumor growths are common causes. Other causes include chest injuries, pleural effusion (fluid accumulation around the lungs), and conditions that limit lung expansion like pneumonia or surgery complications.
4. Who is at risk of developing Atelectasis?
Individuals undergoing major surgeries, especially abdominal or chest surgeries, are at higher risk. Other risk factors include lung diseases, such as asthma or cystic fibrosis, a history of smoking, being bedridden, and having a weak cough due to other health conditions.
5. Can Atelectasis lead to other health issues?
If not addressed, atelectasis can lead to serious complications, including pneumonia, respiratory failure, and in severe cases, hypoxemia (low oxygen levels in the blood). Early detection and treatment are crucial to prevent these complications.
6. How is Atelectasis diagnosed?
Atelectasis is commonly diagnosed through physical examination, listening to the lungs, and imaging tests such as chest X-rays or CT scans. These tests help identify the location and extent of the collapse.
7. What treatments are available for Atelectasis?
Treatment focuses on re-expanding the collapsed lung tissue. This may include respiratory therapies like deep breathing exercises, medications to clear airways, chest physiotherapy, and in some cases, surgery to remove blockages.
8. Can Atelectasis be prevented?
Preventative measures include avoiding smoking, maintaining good lung health, and following breathing exercises, especially after surgery. In hospitals, measures like changing the patient’s position and encouraging movement can help prevent atelectasis in bedridden patients.
9. Is Atelectasis a chronic condition?
Atelectasis itself is not typically chronic, but it can recur, especially in individuals with chronic lung conditions or those frequently undergoing surgeries. Managing underlying conditions is key to preventing recurrence.
10. When should I see a doctor for Atelectasis?
If you experience symptoms like difficulty breathing, chest pain, or a persistent cough, especially after surgery or injury, it’s important to see a healthcare provider for proper diagnosis and treatment.
Conclusion
In this comprehensive overview, we delved into the essential aspects of atelectasis, focusing on its symptoms and causes. To recapitulate, atelectasis is a lung condition characterized by the collapse of air sacs, leading to reduced oxygen exchange. Key symptoms include difficulty breathing, rapid breathing, coughing, and, in severe cases, chest pain and bluish skin coloration. As for its causes, they range from blockages in the airways, like mucus plugs or inhaled foreign objects, to pressure exerted on the lung due to tumors or fluid buildup.
It’s crucial to acknowledge that recognizing these symptoms early plays a vital role in effective management and treatment. If you or someone you know is experiencing any of these signs, it’s imperative to seek medical advice promptly. Timely consultation with a healthcare professional can lead to a faster diagnosis, appropriate treatment, and a better outcome. Remember, your health should always be a top priority, and addressing concerns like atelectasis early can make a significant difference in your overall well-being.