Atelectasis Treatment: Atelectasis, a common yet often misunderstood respiratory condition, involves the partial collapse or incomplete inflation of the lungs.
This condition can be both alarming and complex, impacting patients in varying degrees from mild to severe.
What is Atelectasis?
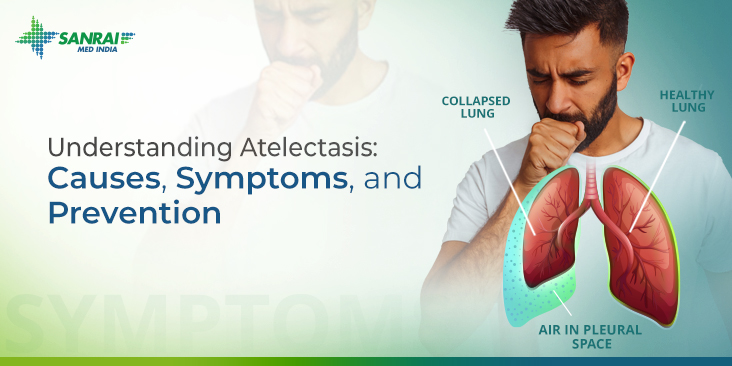
Atelectasis is a medical condition characterized by the partial or complete collapse of one or more areas of the lungs. This condition arises when the tiny air sacs (alveoli) within the lung become deflated, hindering efficient gas exchange. It’s not a disease in itself, but rather a sign of an underlying issue. Atelectasis can occur as a result of a blocked airway or due to pressure from outside the lung. The condition can vary from mild to severe and affects oxygenation and overall lung function.
Common Causes and Risk Factors
Several factors can lead to the development of atelectasis. Common causes include:
- Airway Obstruction: Blockage of the airways due to mucus plugs, foreign bodies, or tumors.
- Pressure on the Lung: This can be due to a buildup of fluid, air, or blood between the lung and chest wall (pleural space).
- Lung Diseases and Conditions: Conditions like pneumonia, chronic obstructive pulmonary disease (COPD), or asthma can predispose an individual to atelectasis.
- Postoperative Complications: It’s commonly seen after surgeries, particularly those involving general anesthesia and abdominal or chest surgeries.
- Immobility: Prolonged bed rest or lack of movement can lead to poor lung expansion, causing atelectasis.
Risk factors enhancing the likelihood of developing atelectasis include advanced age, smoking, obesity, and pre-existing lung conditions.
Types of Atelectasis
Atelectasis can be classified into different types, each with unique characteristics:
- Obstructive Atelectasis: Caused by a blockage in the airways.
- Non-Obstructive Atelectasis: Results from pressure on the lung or by a loss of contact between the lung and chest wall.
- Compression Atelectasis: Occurs when something, like a tumor or fluid, presses on the lung.
- Adhesive Atelectasis: Arises when the surface tension of the alveoli is altered, often due to surfactant deficiency.
Understanding atelectasis is crucial as it helps in the timely diagnosis and management of this condition, which is essential for maintaining optimal lung health and function.
Symptoms of Atelectasis
Recognizing these symptoms early is crucial for timely intervention and treatment. Common signs include:
- Shortness of Breath: One of the primary symptoms, it occurs as the lung’s ability to expand is compromised.
- Rapid, Shallow Breathing: As the body attempts to compensate for reduced lung function, breathing may become quicker and shallower.
- Coughing: A persistent cough can be a sign, especially if it’s non-productive.
- Chest Pain or Discomfort: This symptom, typically occurring on the affected side, can range from mild to severe.
- Fever and General Malaise: In cases where atelectasis is caused by infection or contributes to it, fever and a general feeling of unwellness may be present.
Understanding When to Seek Medical Advice
While some cases of atelectasis are mild and resolve without extensive treatment, it’s essential to know when to seek medical attention. Consult a healthcare professional if you experience:
- Persistent or Worsening Symptoms: If symptoms like shortness of breath or chest pain persist or worsen, it’s important to get medical help.
- Difficulty Breathing: Any breathing difficulties should be evaluated promptly.
- High Fever: A high fever, especially if accompanied by other symptoms of atelectasis, may indicate an infection.
- Sudden Onset of Symptoms: Sudden and severe symptoms can signify a more serious underlying condition and require immediate medical attention.
Early diagnosis and treatment of atelectasis are vital for preventing complications. If you experience any of these symptoms, particularly if you have a history of lung issues or recent surgery, seek medical advice promptly. Remember, your health and well-being are paramount.
Diagnosing Atelectasis: A Comprehensive Guide
Diagnosing Atelectasis involves a combination of clinical assessment and various diagnostic methods. Understanding these methods is crucial for accurate detection and effective treatment of this lung condition.
List of Diagnostic Methods
- Physical Examination: The initial step in diagnosing atelectasis. Doctors listen for abnormal breathing sounds using a stethoscope.
- Chest X-ray: An essential tool, chest X-rays help in identifying areas of collapsed lung tissue.
- Computed Tomography (CT) Scan: Provides a more detailed image than X-rays, helping in detecting smaller areas of lung collapse.
- Oximetry: Measures the oxygen level in the blood, which can be lower in atelectasis.
- Blood Tests: Evaluate oxygen and carbon dioxide levels in the blood, offering insights into the lung’s functionality.
Role of Imaging Tests
Imaging tests play a pivotal role in diagnosing atelectasis:
- Chest X-rays are often the first imaging test used. They can quickly reveal areas where lung tissue has collapsed.
- CT Scans provide detailed images and are particularly useful if the X-ray results are inconclusive or if more information is needed.
- Ultrasound may sometimes be employed to assess the lungs, especially in situations where X-rays are not feasible.
Other Diagnostic Procedures
In addition to imaging tests, other procedures might be necessary:
- Bronchoscopy: A procedure where a camera on a flexible tube is inserted into the airways to directly view the lungs and airways.
- Pulmonary Function Tests (PFTs): Measure the lungs’ capacity to move air in and out, helping in assessing the impact of atelectasis on lung function.
However, diagnosing atelectasis requires a multifaceted approach, combining physical assessments, imaging tests, and other diagnostic procedures. Timely and accurate diagnosis is key to effective management and treatment of this condition.
Treatment Options for Atelectasis
Treatment for atelectasis focuses on re-expanding the collapsed lung tissue and addressing the underlying cause. The approach varies based on the severity of the condition and the patient’s overall health. Early detection and intervention are key to preventing complications.
Medical Treatments
- Airway Clearance Techniques: These involve exercises and devices to help clear mucus and open the airways, promoting lung expansion.
- Breathing Exercises: Techniques such as deep breathing and incentive spirometry encourage lung expansion and improve ventilation.
- Medications: Bronchodilators and mucolytics are often prescribed to open airways and thin mucus, respectively. In some cases, antibiotics are required to treat underlying infections.
- Supplemental Oxygen: For patients with low blood oxygen levels, supplemental oxygen therapy can be vital.
Surgical Options
In severe cases or when medical treatments are ineffective, surgical intervention might be necessary:
- Bronchoscopy: A minimally invasive procedure where a tube is inserted into the airways to remove blockages and facilitate lung expansion.
- Thoracentesis: This procedure involves removing fluid or air from the space around the lungs to allow them to re-expand.
- Lung Surgery: In rare cases, surgery might be required to remove non-responsive lung tissue or to address underlying issues causing the atelectasis.
However, the treatment of atelectasis involves a combination of medical therapies and, in some cases, surgical interventions. Collaborating with a healthcare team is essential for a personalized and effective treatment plan.
Non-Surgical Atelectasis Treatment
Embracing Physical Therapy and Breathing Exercises
Physical therapy plays a pivotal role in the non-surgical treatment of atelectasis. It involves a series of specialized exercises and techniques aimed at improving lung function and promoting airway clearance. By incorporating tailored breathing exercises, patients can significantly enhance lung expansion and facilitate the removal of mucus, which is often a contributing factor to atelectasis. These exercises not only improve lung capacity but also strengthen respiratory muscles, making it easier for patients to breathe and reducing the risk of further lung complications.
The Power of Positioning Techniques
Positioning techniques are another cornerstone of non-surgical atelectasis treatment. These methods involve adjusting a patient’s body position to improve lung expansion and promote mucus clearance. By simply changing the patient’s position, gravity can help in draining secretions from different parts of the lung, improving aeration, and reducing atelectasis. These positioning maneuvers are particularly beneficial as they are non-invasive, easy to implement, and can be tailored to each patient’s specific needs and comfort levels.
Harnessing Incentive Spirometry for Lung Health
Incentive spirometry is an invaluable tool in the non-surgical treatment of atelectasis. This simple device encourages patients to take slow, deep breaths, which aids in lung expansion and mucus clearance. Regular use of an incentive spirometer can significantly improve lung function by preventing or reducing the severity of atelectasis. It’s a patient-friendly approach that empowers individuals to actively participate in their treatment and recovery process.
Preventive Measures and Lifestyle Changes for Atelectasis
This guide provides practical tips and insights into the importance of lifestyle changes in managing and preventing Atelectasis.
Tips for Preventing Atelectasis
- Regular Exercise: Engaging in regular physical activity helps improve respiratory function and lung capacity. It is recommended to incorporate a mix of aerobic exercises and breathing exercises into your routine.
- Quit Smoking: Smoking is a major risk factor for Atelectasis. Quitting smoking not only reduces the risk of lung collapse but also improves overall lung health.
- Healthy Diet: A diet rich in antioxidants, vitamins, and minerals can boost the immune system and improve lung health. Focus on consuming fruits, vegetables, lean proteins, and whole grains.
- Stay Hydrated: Adequate hydration is crucial for maintaining healthy lung tissue. Drink plenty of water throughout the day to keep the airways moist and clear.
- Proper Posture: Maintaining good posture, especially for those who sit for long periods, can help in efficient lung functioning and prevent lung collapse.
- Deep Breathing Exercises: Techniques such as diaphragmatic breathing can help expand the lungs and prevent atelectasis.
- Avoid Exposure to Pollutants: Minimize exposure to environmental pollutants and irritants that can harm lung tissue.
Importance of Lifestyle Changes in Management and Prevention
Lifestyle changes play a pivotal role in managing and preventing Atelectasis. A healthy lifestyle not only reduces the risk of lung collapse but also enhances the body’s ability to recover if the condition occurs. By adopting habits like regular exercise, a balanced diet, and quitting smoking, individuals can significantly improve their lung health. These changes are particularly crucial for those at higher risk, such as postoperative patients or people with chronic respiratory conditions.
Atelectasis can be a daunting condition, but with the right preventive measures and lifestyle changes, its risk and impact can be significantly reduced. Embracing a healthier lifestyle is a key step in maintaining optimal lung health and preventing complications associated with Atelectasis. Remember, small changes can lead to significant health benefits.
Complications of Untreated Atelectasis
Let’s delves into the potential risks associated with untreated atelectasis and underscores the importance of timely intervention.
Potential Complications and Risks
- Increased Infection Risk: Atelectasis creates an environment conducive to bacterial growth, significantly heightening the risk of pneumonia, a severe lung infection.
- Impaired Oxygenation: When lung tissue collapses, it can’t exchange gases effectively. This can lead to decreased oxygen levels in the blood, known as hypoxemia, which can affect other organs.
- Chronic Lung Problems: Prolonged atelectasis can cause permanent damage to lung tissue, leading to chronic respiratory issues and reduced lung function.
- Pleural Effusion: Fluid can accumulate between the lung and chest wall (pleural space), leading to pleural effusion, which can complicate breathing further.
Importance of Timely Treatment
- Preventing Progression: Early treatment can prevent complications, reducing the risk of developing more severe conditions like pneumonia or chronic lung diseases.
- Restoring Lung Function: Prompt intervention helps reinflate the collapsed lung tissue, restoring normal lung function and gas exchange.
- Improving Overall Health: Effective management of atelectasis can improve overall health outcomes, especially in patients undergoing surgery or those with underlying health conditions.
- Reducing Hospital Stay: Timely treatment of atelectasis, particularly in hospitalized patients, can reduce the length of hospital stays and the need for more invasive treatments.
However, addressing atelectasis promptly is crucial to avoid serious health complications. It not only helps in restoring lung function but also plays a significant role in improving the overall health outcomes of affected individuals. If you suspect you have symptoms of atelectasis, consult with a healthcare professional immediately for appropriate diagnosis and treatment.
FAQ Section: Understanding Atelectasis and Its Treatment
1. What is Atelectasis?
Atelectasis is a medical condition where a part or the whole lung collapses or doesn’t inflate properly. This can affect oxygen exchange and cause various symptoms.
2. What Causes Atelectasis?
Common causes include blockages in the airways, surgery, especially chest or abdominal surgery, lung diseases, and prolonged bed rest with few deep breaths.
3. What are the Symptoms of Atelectasis?
Symptoms can vary but often include difficulty breathing, cough, and chest pain. In some cases, there may be no noticeable symptoms.
4. How is Atelectasis Diagnosed?
Doctors usually diagnose atelectasis using imaging tests, such as X-rays or CT scans, sometimes supplemented with oxygen level measurements.
5. What are the Treatment Options for Atelectasis?
Treatment aims to re-expand the collapsed lung tissue. Methods include deep breathing exercises, airway clearance techniques, medications to open airways, or surgery in severe cases.
6. Can Atelectasis be Prevented?
Prevention strategies focus on deep breathing exercises, especially after surgery, smoking cessation, and regular movement to prevent fluid and mucus buildup in the lungs.
7. Is Atelectasis a Serious Condition?
It can be serious, especially if left untreated. It may lead to complications like infections or respiratory failure in severe cases.
8. Does Atelectasis Go Away on Its Own?
Some mild forms may resolve without intensive treatment, but medical intervention is often required to address underlying causes and prevent complications.
9. How Long Does Treatment for Atelectasis Take?
The duration varies depending on the cause and severity. It can range from a few days to weeks. Regular follow-up is important to monitor progress.
10. Who is at Risk of Developing Atelectasis?
Individuals at higher risk include those who have had recent surgery, particularly chest or abdominal surgery, people with lung diseases, smokers, and those who are immobile for prolonged periods.
Conclusion
We strongly encourage individuals experiencing symptoms such as shortness of breath, chest pain, or a persistent cough to seek medical attention immediately. Early consultation with healthcare providers can lead to quicker diagnosis and treatment, potentially averting more severe health issues. Remember, prioritizing your respiratory health is a vital step towards maintaining overall well-being.
In essence, understanding the significance of early diagnosis and effective management of Atelectasis is key. It’s a proactive approach that not only addresses the immediate health concerns but also contributes to long-term health preservation. Therefore, do not hesitate to consult with medical professionals if you experience symptoms indicative of Atelectasis, as early intervention can make a substantial difference in your health journey.