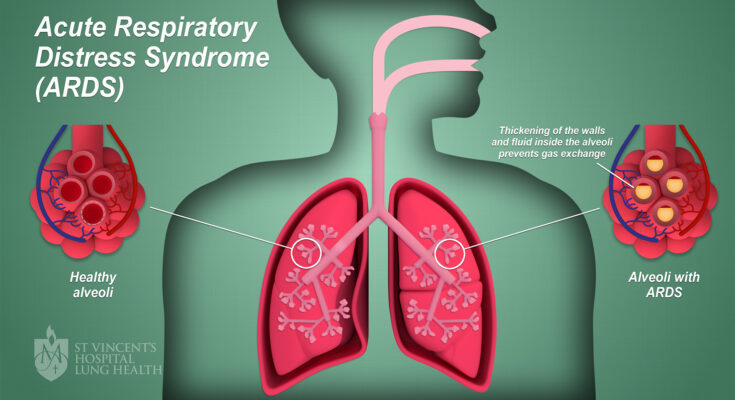
Acute Respiratory Distress Syndrome Treatment: Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition that occurs when fluid fills up the air sacs in the lungs.
This condition not only impedes oxygen from reaching the bloodstream but also makes breathing laboriously difficult.
The complexity of ARDS requires a multidisciplinary approach for diagnosis and treatment, which is critical for patient survival and recovery.
Understanding Acute Respiratory Distress Syndrome (ARDS)
Acute Respiratory Distress Syndrome (ARDS) is a severe lung condition that can be life-threatening. It occurs when fluid builds up in the tiny, elastic air sacs in your lungs, reducing the amount of oxygen that reaches your bloodstream. Understanding ARDS’s pathophysiology, its risk factors, causes, and recognizing the signs and symptoms is crucial for prompt and effective treatment.
A. Pathophysiology of ARDS
The pathophysiology of ARDS involves an intense inflammatory response to an injury or infection. This response leads to increased permeability of the pulmonary capillary endothelium—the thin layer of cells lining the blood vessels in your lungs. As a result, fluid leaks into the alveolar spaces, causing pulmonary edema. The fluid accumulation not only hampers oxygen transfer but also leads to a decrease in lung compliance, making it harder for the lungs to expand. Surfactant dysfunction also occurs, causing the alveoli to collapse and further worsening oxygenation.
B. Risk Factors and Causes
Several factors and causes can precipitate ARDS. The risk factors include:
- Sepsis: The most common cause, where an infection leads to widespread inflammation.
- Inhalation of harmful substances: Including smoke inhalation or chemical fumes.
- Severe pneumonia: Bacterial or viral pneumonia can escalate to ARDS.
- Trauma: Accidents that lead to lung contusions or the aspiration of vomit can trigger ARDS.
- Preexisting chronic diseases: Such as chronic liver or kidney disease.
It’s important to note that not everyone with these risk factors will develop ARDS. The syndrome typically occurs in conjunction with another serious illness or injury.
C. Signs and Symptoms to Watch For
The signs and symptoms of ARDS can develop rapidly and may include:
- Severe shortness of breath: Often the first and most common symptom.
- Labored and rapid breathing: As the body attempts to get more oxygen.
- Hypoxemia: Low blood oxygen levels, which can lead to cyanosis (a bluish cast to the skin and nails).
- Cough and chest discomfort: Sometimes accompanied by frothy sputum.
- Fatigue and weakness: Due to decreased oxygen supply to the muscles.
- Confusion and agitation: Resulting from low oxygen levels to the brain.
If you notice these symptoms, especially after a recent illness or injury, seek medical attention immediately. Early recognition and treatment can improve the prognosis for ARDS patients.
By understanding the complexities of ARDS, its causes, risk factors, and being vigilant for symptoms, better outcomes can be achieved. For those at risk or suffering from the condition, knowledge is not just power—it’s breath.
Diagnosis of Acute Respiratory Distress Syndrome (ARDS)
Understanding the diagnostic criteria and tests for ARDS can lead to better patient outcomes. This guide covers the essentials of diagnosing ARDS, including the criteria, tests, and procedures involved, and how it differs from other respiratory conditions.
A. Diagnostic Criteria for ARDS
The diagnostic criteria for ARDS are primarily based on the Berlin Definition, which includes:
- Timing: Acute onset within one week of a known clinical insult or new or worsening respiratory symptoms.
- Chest imaging (X-ray or CT scan): Showing bilateral opacities not fully explained by effusions, lobar/lung collapse, or nodules.
- Origin of edema: Respiratory failure not fully explained by cardiac failure or fluid overload.
- Oxygenation impairment: Assessed by the PaO2/FiO2 ratio with three categories of severity based on the level of hypoxemia.
B. Key Diagnostic Tests and Procedures
1. Imaging Tests
Imaging tests like chest X-rays and CT scans are crucial for diagnosing ARDS. They help visualize the lungs and detect abnormalities. For ARDS, these images typically show bilateral pulmonary infiltrates that are consistent with pulmonary edema and are not attributed to other forms of lung pathology.
2. Blood Tests
Blood tests are vital in ruling out other causes of lung inflammation and assessing the overall health of the patient. Arterial blood gas analysis is particularly important in ARDS, as it measures the levels of oxygen and carbon dioxide, helping to determine the severity of gas exchange impairment.
3. Pulmonary Function Tests
While not typically used in the acute setting, pulmonary function tests can be instrumental during the recovery phase to assess the long-term impact of ARDS on lung function.
C. The Role of Clinical Evaluation in Diagnosis
Clinical evaluation by healthcare professionals is critical in diagnosing ARDS. A thorough medical history and physical examination are performed to evaluate symptoms such as difficulty breathing, rapid breathing, and low blood pressure. Clinicians also assess risk factors like recent infections, trauma, or inhalation injuries that may lead to ARDS.
D. Differentiating ARDS from Other Respiratory Conditions
Distinguishing ARDS from other respiratory conditions is essential for appropriate management. Conditions such as cardiogenic pulmonary edema, pneumonia, and chronic obstructive pulmonary disease (COPD) can present with similar symptoms. However, ARDS is characterized by the rapid onset of severe hypoxemia and bilateral infiltrates on chest imaging that are not explained by heart failure or volume overload, setting it apart from other conditions.
However, diagnosing ARDS involves a combination of clinical judgment and specific diagnostic tests that assess respiratory function and imaging. Early recognition and differentiation from other respiratory conditions are critical steps towards the effective management of ARDS. Medical professionals must rely on a comprehensive evaluation that integrates clinical findings with test results to confirm the presence of this life-threatening syndrome.
Acute Respiratory Distress Syndrome Treatment
Managing Acute Respiratory Distress Syndrome (ARDS) is a critical and delicate process. Successful treatment hinges on a multifaceted strategy that prioritizes patient stabilization and lung protection. Below, we explore the primary goals and the multidisciplinary approach characterizing ARDS management.
A. The Goals of ARDS Treatment
The primary objectives in treating ARDS are twofold:
- Maintaining Adequate Oxygenation: Ensuring that the body’s tissues receive sufficient oxygen is paramount. This involves precise oxygen therapy, which may include mechanical ventilation to alleviate the burden on the lungs and guarantee efficient gas exchange.
- Addressing the Underlying Cause: ARDS is often a symptom of a broader health issue. Identifying and treating the root cause, whether it’s an infection, trauma, or other medical conditions, is essential to recovery.
These goals underscore the necessity of a nuanced treatment plan that adapts to the severity and progression of ARDS, as well as the individual needs of the patient.
B. The Multidisciplinary Treatment Approach
A collaborative, multidisciplinary team is key in managing ARDS. This team typically includes:
- Pulmonologists and critical care specialists who guide the respiratory management of ARDS.
- Nurses with critical care expertise, providing round-the-clock care and monitoring.
- Respiratory therapists to administer and adjust oxygen therapy and mechanical ventilation.
- Infectious disease experts if the ARDS is related to an infection.
- Pharmacists to manage medication regimens.
- Nutritionists to support recovery with appropriate nutritional plans.
- Physical therapists to aid in the prevention of muscle weakness due to prolonged immobilization.
This comprehensive team works in concert to tailor treatment strategies to each patient, aiming for the best possible outcomes.
However, treating ARDS requires a meticulous blend of supportive care and targeted medical intervention. By combining the efforts of various healthcare professionals, the treatment of ARDS can be optimized, offering hope and improved recovery rates for those affected by this challenging condition.
Initial Management and Supportive Care in ARDS
Acute Respiratory Distress Syndrome (ARDS) requires immediate and effective initial management to improve patient outcomes. This guide highlights the supportive care strategies essential for treating ARDS, including oxygen therapy, ventilation strategies, fluid management, hemodynamic support, and nutritional support.
A. Oxygen Therapy and Ventilation Strategies
Effective oxygen delivery and maintaining proper ventilation are critical components of ARDS management. Here’s how these can be optimized:
- High-Flow Nasal Cannula (HFNC): HFNC therapy delivers warm, humidified oxygen at a high flow rate through nasal prongs, which can reduce the need for intubation. It allows for better oxygenation and comfort, making it a front-line treatment in mild to moderate ARDS cases.
- Mechanical Ventilation: For more severe cases of ARDS, mechanical ventilation is often required. The aim is to ensure adequate oxygenation while minimizing lung injury by using lung-protective ventilation strategies. This involves setting a low tidal volume and applying positive end-expiratory pressure (PEEP) to prevent alveolar collapse.
- Prone Positioning: Placing patients in a prone (face down) position can improve oxygenation by redistributing blood flow and enhancing lung mechanics. This strategy, often used in conjunction with mechanical ventilation, has been shown to reduce mortality in severe ARDS.
B. Fluid Management and Hemodynamic Support
The approach to fluid management in ARDS is a delicate balance. It’s crucial to maintain adequate perfusion while avoiding fluid overload, which can exacerbate lung edema. Diuretics and vasopressors may be employed to maintain this balance and support the patient’s blood pressure. Regular monitoring of hemodynamic status with tools like echocardiography or invasive pressure monitoring is essential for guiding treatment.
C. Nutritional Support and Its Importance in ARDS
Nutrition is a pivotal part of supportive care in ARDS. The metabolic demands of patients with ARDS are high, and meeting these demands with proper nutritional support is vital for recovery. Enteral nutrition, preferably started within 48 hours of ICU admission, can help maintain gut integrity and immune function. Tailoring caloric intake to avoid underfeeding or overfeeding is equally important to support the healing process and potentially improve clinical outcomes.
However, a structured approach to initial management and supportive care is fundamental in the treatment of ARDS. Oxygen therapy and ventilation, prudent fluid management, and adequate nutritional support form the triad of essential care practices that can contribute to better recovery and survival rates in affected patients. Clinicians must stay abreast of evolving guidelines and individualize treatment for optimal patient care.
Pharmacological Treatments for ARDS
Acute Respiratory Distress Syndrome (ARDS) presents a formidable challenge in critical care, necessitating a multifaceted approach to management. Within this framework, pharmacological treatments play a pivotal role in patient recovery.
A. Corticosteroids: Uses and Considerations
Corticosteroids have emerged as a cornerstone in ARDS management, primarily due to their potent anti-inflammatory properties. These drugs can help reduce lung inflammation, which is a hallmark of ARDS. However, the use of corticosteroids must be carefully weighed against potential side effects, such as increased risk of infection and impact on blood sugar levels. Physicians often consider the timing, dosage, and duration of corticosteroid therapy to optimize patient outcomes while minimizing risks.
B. Antibiotics and Infection Control
Infection control is critical in ARDS, especially since bacterial infections can exacerbate lung damage. Antibiotics are therefore commonly administered when an infectious etiology is suspected or confirmed. The selection of antibiotics should be guided by the pathogen profile, patient history, and local antimicrobial resistance patterns. Timely and appropriate antibiotic therapy is crucial for preventing further lung complications and promoting recovery.
C. Experimental and Adjunctive Therapies
1. Anti-inflammatory Agents
Beyond corticosteroids, other anti-inflammatory agents are being explored for their potential benefits in ARDS. These experimental treatments aim to modulate the body’s immune response, thus reducing lung inflammation and injury. However, the effectiveness and safety of these agents are still under investigation through clinical trials.
2. Pulmonary Vasodilators
Pulmonary vasodilators are used to alleviate high blood pressure in the lungs’ arteries, which is a common issue in ARDS. By dilating these blood vessels, they can improve oxygenation and reduce strain on the heart. However, their use is complex and requires careful monitoring due to the risk of causing systemic hypotension.
3. ECMO (Extracorporeal Membrane Oxygenation)
For severe ARDS cases where conventional treatments are inadequate, ECMO stands as a lifesaving intervention. ECMO acts as an external lung that oxygenates the blood outside the body, giving the patient’s lungs time to heal. This advanced therapy requires a specialized team and facility, and is typically considered when other treatments have failed to improve the patient’s condition.
However, the pharmacological treatment of ARDS involves a combination of established and emerging therapies tailored to the individual’s needs. Medical professionals continuously adapt to the evolving landscape of ARDS treatment, ensuring the best possible outcomes for their patients.
Advanced Treatment Strategies for Acute Respiratory Distress Syndrome
Acute Respiratory Distress Syndrome (ARDS) presents a critical challenge in critical care. With the advances in medical science, innovative strategies have enhanced the management of ARDS, offering hope and improved outcomes for patients. Below, we delve into advanced treatment strategies that are reshaping the approach to this serious condition.
Innovative Ventilation Techniques
The cornerstone of ARDS treatment is ventilatory support. However, traditional ventilation methods can sometimes lead to further lung injury. Innovative ventilation techniques have emerged to circumvent this issue. High-frequency oscillatory ventilation (HFOV) and airway pressure release ventilation (APRV) are two such methods that have shown promise. These techniques aim to improve oxygenation and reduce the risk of ventilator-induced lung injury by using lower tidal volumes and allowing spontaneous breathing, which can lead to better outcomes.
Surgical Interventions and When They Are Indicated
Surgical intervention in ARDS is less common but may be indicated in certain situations. For example, when ARDS is complicated by pneumothorax or significant pleural effusions, surgical procedures like thoracostomy or pleural drainage can be life-saving. Additionally, in cases of severe ARDS where conventional therapies fail, extracorporeal membrane oxygenation (ECMO) can be a last-resort option. ECMO acts as an artificial lung, providing oxygenation outside of the body, and it has been shown to increase survival rates in severe cases.
Long-term Treatment Considerations
The journey of ARDS recovery often extends beyond the acute phase. Long-term treatment considerations focus on rehabilitation and the management of residual lung damage. Pulmonary rehabilitation programs are crucial, as they help patients regain lung function and improve their quality of life. Nutritional support, psychological counseling, and regular monitoring for potential complications like pulmonary fibrosis or secondary infections also play a significant role in the holistic care of ARDS survivors.
However, the advanced treatment strategies for ARDS require a multidisciplinary approach, integrating innovative ventilation techniques, timely surgical interventions, and comprehensive long-term care. Continuous research and personalized treatment plans are essential for improving the prognosis of ARDS patients, allowing them to achieve the best possible outcomes.
Complications and Monitoring in ARDS Management
Understanding potential complications and implementing effective monitoring strategies is crucial for patient outcomes.
A. Potential Complications of ARDS and Its Treatments
ARDS and its treatments can lead to a range of complications. The nature of the condition often necessitates intensive care and invasive procedures, which inherently carry risks:
Ventilator-Associated Lung Injury (VALI): Patients with ARDS may require mechanical ventilation. This life-saving measure can sometimes exacerbate lung damage due to the high pressure and oxygen levels needed.
Infections: Prolonged hospital stays and the use of catheters or ventilators increase the risk of bacterial and viral infections, which can further complicate the patient’s condition.
Barotrauma: The pressure exerted by mechanical ventilation can lead to air leaks from the lungs into the chest cavity, a condition known as pneumothorax.
Fluid Imbalance and Organ Failure: The delicate balance of fluids in the body can be disrupted, leading to issues such as kidney failure or heart problems.
Sedation-Related Issues: Long-term sedation, often necessary for comfort and treatment compliance, can lead to muscle weakness and prolonged recovery times.
B. Strategies for Monitoring and Mitigating Complications
Timely and effective monitoring is key to mitigating the complications associated with ARDS:
Regular Assessment of Ventilator Settings: Adjusting ventilator settings to the lowest effective levels can reduce the risk of VALI and barotrauma.
Infection Control Protocols: Rigorous infection control measures, including hand hygiene and sterilization practices, are essential in preventing secondary infections.
Hemodynamic Monitoring: Careful monitoring of fluid balance and cardiovascular status helps prevent fluid overload and supports organ function.
Nutritional Support: Adequate nutrition supports healing and can help prevent muscle wasting associated with prolonged sedation and immobility.
Physical Therapy and Mobilization: Early physical therapy can mitigate muscle weakness and improve long-term functionality.
By anticipating these complications and employing thorough monitoring techniques, healthcare professionals can significantly enhance the prognosis for ARDS patients. Staying vigilant and responsive to the changing needs of ARDS patients is fundamental for improved recovery rates and better health outcomes.
Rehabilitation and Recovery After ARDS
The Road to Recovery Post-ARDS
Recovery from Acute Respiratory Distress Syndrome (ARDS) is a gradual process that requires patience, determination, and specialized care. The journey to regain health and well-being after ARDS can vary significantly from person to person, depending on the severity of the condition and the individual’s overall health. It’s essential to understand that while the road to recovery can be lengthy and sometimes challenging, with the right support and resources, patients can work towards rebuilding their lives. Embracing a multidisciplinary approach to recovery is crucial. This includes consistent medical follow-up, lifestyle adjustments, and psychological support to address the wide-ranging effects of the syndrome.
Physical and Pulmonary Rehabilitation Programs
Physical and pulmonary rehabilitation programs are central to the recovery process for ARDS survivors. These specialized programs are designed to improve lung function, enhance physical strength, and increase endurance, helping individuals regain their ability to perform daily activities. Pulmonary rehabilitation typically includes exercise training, education on lung health and breathing strategies, as well as nutritional counseling. Tailored to each individual’s needs, these programs often involve a team of health professionals, including physical therapists, respiratory therapists, and nutritionists, working together to provide a comprehensive plan for recovery. The goal is not only to restore physical capabilities but also to boost confidence and promote independence.
Coping with Long-Term Effects and Quality of Life Issues
Long-term effects of ARDS, such as persistent fatigue, muscle weakness, and psychological impacts like anxiety or depression, can pose significant challenges to patients’ quality of life. It’s imperative for survivors and their caregivers to recognize and address these issues early on. Strategies to cope with long-term effects may include:
- Emotional Support: Access to mental health professionals who can provide counseling and treatment for emotional distress.
- Community Resources: Involvement in support groups where experiences are shared and peer support is available.
- Adaptive Strategies: Learning new ways to manage daily tasks that accommodate the individual’s current abilities.
- Education: Understanding the potential long-term effects of ARDS can empower patients and families to advocate for their needs and seek out appropriate care.
Incorporating these coping mechanisms is key to enhancing the quality of life for ARDS survivors. It’s also beneficial to maintain open communication with healthcare providers to continuously adjust care plans as recovery progresses. By acknowledging the challenges and systematically approaching rehabilitation and recovery, individuals can work towards reclaiming their lives post-ARDS.
Prevention and Prognosis of ARDS
Navigating through Acute Respiratory Distress Syndrome (ARDS) involves understanding its prevention and the prognosis for affected individuals. Here, we’ll explore effective strategies to reduce the risk of developing ARDS, factors that influence outcomes, and the future of ARDS treatment.
A. Strategies to Reduce the Risk of Developing ARDS
Preventing ARDS starts with addressing the underlying causes. Here are key strategies:
- Infection Prevention: Practicing good hygiene and staying current with vaccinations can thwart infections that may escalate into ARDS.
- Smoke-Free Environment: Avoiding smoking or exposure to secondhand smoke is crucial, as tobacco smoke can damage the lungs and increase ARDS risk.
- Safety Measures: Implementing safety protocols to prevent trauma and injury can reduce the number of ARDS cases resulting from accidents.
- Prompt Treatment: Early intervention in diseases like pneumonia or sepsis can prevent progression to ARDS.
Adhering to these strategies can significantly diminish the incidence of ARDS and promote lung health.
B. Prognosis and Factors Influencing Outcomes
The prognosis for ARDS patients varies, influenced by:
- Age: Younger patients generally have better recovery rates.
- Severity of Illness: The extent of lung injury and the patient’s overall health condition play a role.
- Medical Care Quality: Timely, high-quality medical intervention can improve survival rates.
- Preexisting Conditions: Patients without prior lung or heart conditions tend to have more favorable outcomes.
Awareness of these factors is vital for healthcare providers and patients in managing expectations and treatment plans.
C. Research and Future Directions in ARDS Treatment
The horizon for ARDS treatment is expanding with ongoing research:
- Personalized Medicine: Studies are looking into genetic markers that influence ARDS risk and response to treatment, aiming for tailored therapies.
- Innovative Therapies: Research on stem cell therapy and bioengineered lungs holds promise for reparative treatments.
- Enhanced Mechanical Ventilation: Refining ventilation strategies to minimize lung injury could transform patient management.
Keeping abreast of these developments is essential for healthcare professionals and offers hope for improved treatment and survival rates.
Conclusion
In conclusion, ARDS is a multifaceted disease that requires a comprehensive approach to diagnosis and treatment. Early recognition, appropriate ventilation strategies, judicious fluid management, and meticulous supportive care are the pillars of ARDS management.
Through a combination of advanced medical interventions and personalized patient care, the morbidity and mortality associated with ARDS can be significantly reduced.