Acute Kidney Failure Treatment: Acute Kidney Failure, often referred to as Acute Kidney Injury (AKI), is a medical condition where there is a rapid decrease in kidney function within a short period.
This can lead to an accumulation of waste products in the blood, causing complications that can affect other organs. Timely diagnosis and treatment are paramount to prevent any permanent damage.
What is Acute Kidney Failure?
Acute Kidney Failure, also commonly referred to as Acute Kidney Injury (AKI), is a sudden and temporary loss of kidney function. This condition can develop within a few hours to a few days, and it means that the kidneys aren’t filtering out waste, excess fluids, and electrolytes from the blood as efficiently as they should. Common causes include certain medications, dehydration, severe infections, and certain chronic conditions. Early detection and appropriate medical treatment can help in restoring kidney function.
Differences Between Acute and Chronic Kidney Failure
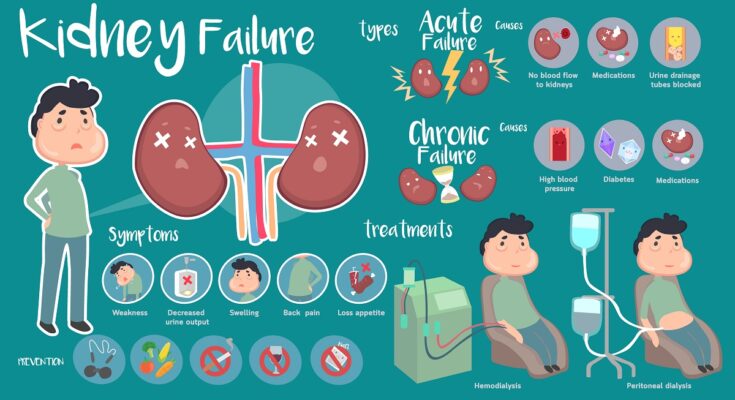
Duration and Onset: Acute Kidney Failure is sudden and often reversible, developing within hours to days. In contrast, Chronic Kidney Failure, also known as Chronic Kidney Disease (CKD), develops gradually over a period of months to years and is often irreversible.
Causes: While both types can have overlapping causes, AKI often results from an abrupt injury or insult to the kidneys such as trauma, dehydration, or specific medications. CKD, on the other hand, frequently results from long-standing health issues like hypertension, diabetes, or prolonged use of certain medications.
Symptoms: Symptoms of AKI might manifest more abruptly and can include fluid retention, fatigue, and confusion. CKD symptoms tend to develop gradually and might include anemia, bone pain, and changes in urination patterns.
Treatment: The treatment for AKI is often focused on treating the underlying cause and supporting kidney function until it can recover. Chronic Kidney Failure treatments might involve managing underlying conditions, slowing the progression of the disease, and addressing complications.
Understanding the distinctions between acute and chronic kidney failure can aid in timely diagnosis and optimal management. Regular health check-ups and being aware of risk factors can be beneficial for kidney health.
Primary Causes of Acute Kidney Failure
Understanding its primary causes can help in both prevention and early detection. Here’s a simplified breakdown:
1. Decreased Blood Flow to the Kidneys
Significant blood loss: Injuries or surgeries can lead to a substantial loss of blood, affecting the kidneys’ ability to function properly.
Severe dehydration: Not drinking enough water, excessive sweating, or conditions like diarrhea can lead to dehydration. When severe, it reduces the blood flow to the kidneys.
Low blood pressure: Chronic low blood pressure can harm the kidneys. Sudden drops, even if temporary, can also be detrimental.
2. Direct Damage to the Kidneys
Certain medications and toxins: Some drugs, like non-prescription pain meds, can be toxic to the kidneys. Similarly, being exposed to certain toxins can lead to acute kidney damage.
Infections: Kidney infections, when severe, can lead to acute failure if not treated promptly.
Reduction in urine flow due to obstructions: Stones or tumors can block the flow of urine, causing damage to the kidneys.
3. Glomerulonephritis
Explanation: Glomerulonephritis is an inflammation of the tiny filters in the kidneys called glomeruli. These filters help remove excess fluid, electrolytes, and waste from the bloodstream. When inflamed, they can’t function optimally.
Impact on kidney function: This inflammation can cause the kidneys to leak important proteins from the blood into the urine. Over time, it can reduce the kidneys’ ability to clean the blood efficiently, leading to acute kidney failure.
Being aware of these primary causes can be instrumental in taking preventive measures and seeking timely medical attention. Remember, the kidneys play a crucial role in our overall health; keeping them in good shape should be a priority.
Acute Kidney Failure Symptoms
Acute kidney failure is a serious condition that can manifest in several noticeable symptoms. Detecting these signs early can be crucial for timely medical intervention.
Early Warning Signs
Decreased urine output: One of the primary symptoms is producing less urine than usual.
Swelling in legs, ankles, and feet: Reduced kidney function can lead to fluid retention causing noticeable swelling in the lower extremities.
Shortness of breath: Fluid buildup in the body might pressure the lungs, leading to difficulty breathing.
Moderate to Severe Symptoms
Nausea and vomiting: The body’s inability to filter out waste can cause feelings of nausea and episodes of vomiting.
Fatigue and confusion: Accumulation of toxins in the blood can result in feeling constantly tired and may lead to confusion.
Chest pain or pressure: The heart and kidneys are closely linked; compromised kidney function can stress the heart.
Seizures or coma: In extreme cases, untreated kidney failure might lead to seizures or even a coma.
Other Notable Indicators
Abnormal urine color: Changes in urine, such as it becoming bloody or foamy, can signal kidney issues.
Feeling drowsy or overly tired: Apart from fatigue, a continuous feeling of drowsiness can also indicate poor kidney function.
If you or someone you know experiences any of these symptoms, it’s essential to seek medical advice promptly. Detecting kidney problems early can make a significant difference in treatment outcomes.
Diagnostic Procedures of Acute Kidney Failure
Prompt diagnosis is crucial for appropriate treatment. Here’s a brief overview of the diagnostic procedures employed to detect acute kidney failure:
1. Initial Assessment: Patient History and Physical Examination
Before diving into advanced diagnostics, a thorough initial assessment is paramount. This involves:
Patient History: Doctors will inquire about symptoms, previous medical conditions, and any medications or treatments the patient might be on. This helps in identifying potential causes or risk factors.
Physical Examination: Checking for signs such as swelling, changes in skin color, or blood pressure can provide clues about kidney function and overall health.
2. Lab Tests
Laboratory tests provide measurable data about kidney function:
Blood Tests: These are vital in assessing kidney health. Elevated levels of creatinine and urea in the blood often indicate reduced kidney function.
Urine Tests: Analyzing a urine sample can reveal abnormalities, like the presence of blood or protein, which might suggest kidney problems.
3. Imaging
Modern imaging techniques can offer a clear view of the kidneys and their surrounding structures:
Ultrasound: A non-invasive procedure using sound waves to create images of the kidneys. It can show size, position, and any obstructions.
CT (Computed Tomography): This detailed imaging technique provides cross-sectional images of the kidneys, aiding in spotting any abnormalities.
MRI (Magnetic Resonance Imaging): An advanced imaging method that gives a detailed view of the kidneys and can detect issues that other imaging methods might miss.
4. Kidney Biopsy: When and Why It’s Needed
Sometimes, to determine the exact cause of kidney malfunction, a small tissue sample from the kidney (a biopsy) is needed. This procedure involves inserting a needle into the kidney to retrieve a sample. It’s particularly useful when:
+ The cause of the kidney issue remains unclear after other diagnostic tests.
+ A kidney biopsy is not always necessary, but when done, it provides invaluable insights into the nature and severity of the kidney issue at hand.
However, diagnosing acute kidney failure involves a combination of patient history, physical examinations, lab tests, imaging, and sometimes a biopsy. Early detection and understanding the cause are vital for effective treatment and recovery.
Acute Kidney Failure Treatment Options
Prompt and effective treatment is essential to prevent long-term complications. Here are the key treatment options available:
1. Fluids and Medications:
IV Fluids for Dehydration: One of the primary treatments for acute kidney failure is the administration of intravenous (IV) fluids. This helps in rehydrating the body and ensuring that the kidneys have an adequate supply of blood.
Medications to Balance Electrolytes: The kidneys play a vital role in balancing electrolytes in the body. When they fail, this balance is disrupted. Medications can be administered to help restore this balance and prevent complications.
Medications to Treat Underlying Causes: Depending on the cause of the kidney failure, specific medications may be prescribed. For instance, antibiotics may be given for an infection, or certain drugs might be discontinued if they’re found to be the cause.
2. Dialysis:
Dialysis is a procedure that mimics the kidney’s function by filtering and cleaning the blood.
Hemodialysis: In this method, blood is drawn out of the body, cleaned by a machine, and then returned to the body.
Peritoneal Dialysis: Here, a fluid is introduced into the abdomen. This fluid captures waste products from the blood passing through vessels in the abdominal wall and is then drained out.
The choice between hemodialysis and peritoneal dialysis depends on the patient’s medical condition, lifestyle, and personal preferences.
3. Treating Underlying Causes:
It’s essential to address the root causes of kidney failure for effective treatment. This could involve:
Management of Infections: Infections can be a significant cause of acute kidney failure. They need to be diagnosed and treated promptly with appropriate antibiotics or antiviral medications.
Adjusting Nephrotoxic Medications: Some medications can harm the kidneys. If these drugs are identified as the cause of the kidney problem, they may be discontinued or adjusted.
4. Preventative Measures:
Monitoring Medications: Regularly reviewing and adjusting medications that are known to affect the kidneys is essential to prevent further damage.
Staying Hydrated: Drinking adequate water supports kidney function and helps prevent dehydration.
Maintaining Blood Pressure: Keeping blood pressure in check can prevent further strain on the kidneys and reduce the risk of additional complications.
However, the treatment for acute kidney failure is multifaceted and tailored to the individual’s needs. Regular medical checks and adhering to medical advice are crucial for recovery and long-term kidney health.
Complications and Long-term Outlook of Acute Kidney Failure
Below, we delve into the potential complications of this ailment and provide insights into its long-term prognosis.
Potential Complications
Chronic Kidney Disease (CKD): One of the severe complications arising from acute kidney failure is the progression to chronic kidney disease. When the kidneys are damaged abruptly but don’t recover fully, it can set the stage for a long-term decline in kidney function.
End-Stage Renal Disease (ESRD): If chronic kidney disease continues to progress, it may lead to end-stage renal disease. At this stage, the kidneys have lost nearly all their functional capabilities, and the affected person might require lifelong dialysis or a kidney transplant.
Death: Acute kidney failure is a severe condition, and if not addressed promptly or if complications arise, it can unfortunately lead to fatality.
Prognosis and Factors Influencing Recovery
The prognosis for acute kidney failure varies from one person to another. Several factors can influence the recovery outcome:
Timely Treatment: Early diagnosis and immediate medical intervention can significantly improve the chances of full recovery.
Underlying Causes: The prognosis often depends on the root cause of the kidney failure. Conditions that are treatable or reversible often have a better prognosis compared to those that are not.
Overall Health: Individuals with pre-existing health conditions or those who have compromised immune systems might face a more challenging recovery path.
Age: Younger individuals tend to recover faster and better than older adults, though age alone isn’t the only determinant.
However, while acute kidney failure poses significant health threats, with prompt treatment and medical care, many individuals can recover. However, the potential complications emphasize the importance of early diagnosis, awareness, and proactive management of this condition.
FAQs about Acute Kidney Failure Treatment
When faced with a diagnosis of acute kidney failure, also known as acute renal failure, patients and their loved ones often have numerous questions about the condition, its diagnosis, and the available treatment options. Below are some of the most frequently asked questions to help you understand this medical emergency better.
What Are the First Signs That Suggest I Might Have Acute Kidney Failure?
Acute kidney failure can manifest through various symptoms such as decreased urine output, fluid retention causing swelling in your legs, ankles or feet, shortness of breath, fatigue, confusion, nausea, and chest pain or pressure. If you notice any of these symptoms, it is crucial to seek medical attention promptly.
How Is Acute Kidney Failure Diagnosed?
Acute kidney failure is diagnosed through several tests and procedures. These may include:
- Blood tests: These can determine the level of waste products such as creatinine and urea in your blood, which are indicators of kidney function.
- Urine tests: Examining a sample of your urine, a process known as urinalysis, can help reveal abnormalities that suggest kidney failure.
- Imaging tests: Diagnostic imaging such as ultrasounds or CT scans can show the size and structure of your kidneys, as well as any blockages.
- Kidney biopsy: In some cases, a sample of kidney tissue may be removed for testing to determine the cause of the kidney failure.
What Are the Treatment Options for Acute Kidney Failure?
The treatment for acute kidney failure typically depends on the underlying cause. Some of the treatments may include:
- Medications: To control blood potassium, restore blood calcium levels, or to remove excess fluid.
- Dialysis: This helps to remove toxins and excess fluids from your body when your kidneys can’t do this effectively.
- Managing underlying causes: Treating the source of the kidney failure, such as controlling blood pressure in cases of hypertension or managing diabetes.
- Lifestyle adjustments: Dietary changes and fluid restrictions can be important to help manage symptoms.
Is Acute Kidney Failure Reversible?
Acute kidney failure is often reversible if it is caught early and treated promptly. The kidneys have a remarkable ability to recover from damage caused by an acute injury or illness. However, the recovery might vary from patient to patient, depending on the severity of the condition and overall health.
How Long Does Treatment for Acute Kidney Failure Last?
The duration of treatment for acute kidney failure depends on the severity of the condition and the patient’s response to therapy. In cases where the kidney failure is due to a blockage, treatment may involve surgery and could resolve quickly. However, if the cause is more complex, such as a disease process, the treatment may be longer and could include regular dialysis.
Understanding your condition and its treatment options is vital in managing acute kidney failure. Always consult your healthcare provider for more personalized information and advice about your specific situation. Remember that early detection and treatment are crucial in improving outcomes for acute kidney failure.
Conclusion
Acute Kidney Failure is a severe condition that warrants immediate attention. Awareness of its symptoms and causes, combined with early diagnosis and treatment, can lead to better outcomes.
By staying informed and making healthy lifestyle choices, one can significantly reduce the risks associated with this condition.