Brugada Syndrome Treatment: Brugada Syndrome, a life-threatening heart rhythm disorder, has long been a subject of medical intrigue and concern.
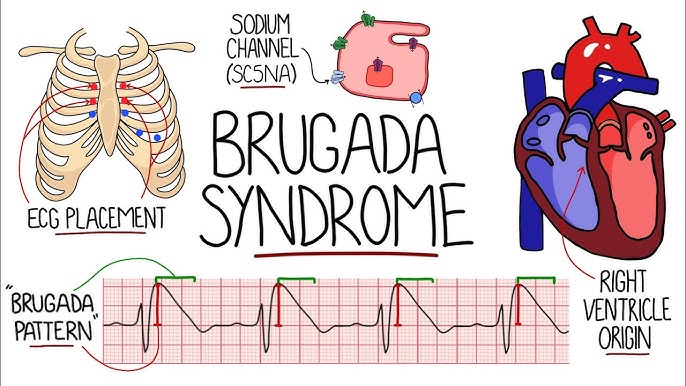
Characterized by abnormal electrocardiogram (ECG) findings and an increased risk of sudden cardiac death, this condition poses significant challenges in both diagnosis and treatment.
This comprehensive article delves into the nuances of Brugada Syndrome, offering vital insights into its management and therapeutic interventions.
What is Brugada Syndrome?
Brugada Syndrome is a rare yet notable cardiac disorder characterized by abnormal electrocardiogram (ECG) findings and an increased risk of sudden cardiac death. It primarily affects the heart’s electrical system, leading to irregular heart rhythms, which can be life-threatening. This condition is often undetected until it manifests in potentially dangerous arrhythmias or is inadvertently discovered during routine ECG screenings.
Prevalence and Demographics: A Statistical Insight
Statistically, Brugada Syndrome is relatively uncommon, but its exact prevalence varies globally. Estimates suggest it affects about 1 in 2,000 individuals worldwide. However, its occurrence is more prevalent in certain regions, particularly in Southeast Asia. It tends to manifest more frequently in males, with a higher incidence observed in men than in women. The syndrome is most commonly diagnosed in adults, often in their thirties or forties, although it can affect individuals of any age, including children.
Genetic Factors and Triggers: The Underlying Causes
The genetic underpinnings of Brugada Syndrome are significant, with a notable proportion of cases linked to mutations in the SCN5A gene. This gene plays a critical role in the function of heart cells, particularly in the conduction of electrical impulses. Approximately 20-30% of patients with Brugada Syndrome have a family history of the condition, indicating a strong hereditary component.
Besides genetic factors, certain triggers can exacerbate the risk of arrhythmias in individuals with Brugada Syndrome. These include:
- Fever: A high body temperature can induce arrhythmic events in those with the syndrome.
- Alcohol and drug consumption: Certain substances can interfere with the heart’s electrical activity, increasing the risk of arrhythmias.
- Electrolyte imbalances: Imbalances in bodily minerals essential for heart function can trigger symptoms.
- Medications: Some drugs, especially those that affect cardiac conduction, can increase the risk of life-threatening arrhythmias in Brugada Syndrome patients.
However, Brugada Syndrome is a significant cardiac condition with unique characteristics, affecting individuals globally but with varying prevalence. Understanding its genetic basis and potential triggers is crucial for managing and reducing the risks associated with this syndrome. Early detection through ECG and genetic testing, especially in those with a family history, is vital for effective management and prevention of serious cardiac events.
Symptoms and Early Signs of Brugada Syndrome
Recognizing its symptoms and early signs is crucial for timely diagnosis and treatment. Here, we explore the most common symptoms associated with Brugada Syndrome, the potential for misdiagnosis, and the importance of early detection.
Common Symptoms of Brugada Syndrome
Abnormal Heart Rhythms (Arrhythmias): One of the primary symptoms of Brugada Syndrome is an irregular heartbeat. Patients might experience palpitations, where the heart beats too fast, too slow, or irregularly.
Fainting (Syncope): Sudden fainting episodes can occur due to the heart’s inability to pump blood effectively.
Seizures: In some cases, the disrupted heart rhythm can lead to seizures.
Difficulty Breathing or Chest Pain: Although less common, some individuals may experience these symptoms, particularly during physical exertion.
Brugada Syndrome and Misdiagnosis
Brugada Syndrome can often be mistaken for other conditions, leading to misdiagnosis:
Epilepsy: Due to seizures associated with heart rhythm disturbances, it might be misinterpreted as epilepsy.
Panic Attacks or Anxiety: The symptoms like palpitations and difficulty breathing can be mistaken for anxiety-related conditions.
Other Heart Conditions: Symptoms can overlap with other cardiac issues, making it challenging to pinpoint Brugada Syndrome without specific tests.
3. The Importance of Early Detection
Preventing Sudden Cardiac Arrest: Early recognition of Brugada Syndrome is vital because it can lead to sudden cardiac arrest, particularly in young adults.
Timely Treatment: Early diagnosis allows for appropriate management strategies, like medication or the implantation of a cardioverter-defibrillator (ICD) to prevent arrhythmias.
Genetic Counseling: Since Brugada Syndrome is genetic, early diagnosis can also lead to family screenings and genetic counseling to assess the risk for relatives.
Being aware of the symptoms and early signs of Brugada Syndrome is essential for timely intervention and proper management. Regular check-ups and discussions with a healthcare provider, especially if you have a family history of the condition, can significantly reduce risks and improve outcomes.
Diagnostic Approaches of Brugada Syndrome
Understanding the nuances of its diagnostic procedures is vital for healthcare professionals and patients alike. This article delves into the various diagnostic tests, the significance of medical history and physical examination, and the challenges and advancements in diagnosing Brugada Syndrome.
List of Diagnostic Tests
Electrocardiogram (ECG)
The primary tool for diagnosing Brugada Syndrome is the Electrocardiogram (ECG). This test records the electrical activity of the heart and can detect abnormal patterns characteristic of Brugada Syndrome.
Genetic Testing
Since Brugada Syndrome can be hereditary, genetic testing is recommended. This involves analyzing DNA to identify mutations associated with the syndrome.
Drug Challenge Test
A drug challenge test, typically using medications like ajmaline or flecainide, helps in unmasking the ECG patterns indicative of Brugada Syndrome.
Electrophysiological Study (EPS)
In some cases, an Electrophysiological Study (EPS) may be performed. This invasive test studies the heart’s electrical signals and assesses the risk of arrhythmias.
The Role of Medical History and Physical Examination
Medical history and physical examination play a crucial role in diagnosing Brugada Syndrome. A thorough medical history can reveal symptoms like fainting or family history of sudden cardiac death, which are critical in suspecting Brugada Syndrome. The physical examination, although often normal, helps rule out other causes of the symptoms.
Challenges and Advancements in Diagnosing Brugada Syndrome
Challenges
Variable ECG Findings: The ECG patterns in Brugada Syndrome can be intermittent, making diagnosis challenging.
Asymptomatic Patients: Many patients with Brugada Syndrome show no symptoms, delaying diagnosis until a serious event occurs.
Advancements
Improved Genetic Testing: Advances in genetic testing have made it possible to identify more people at risk.
Better Risk Stratification: New research and techniques in risk stratification help in identifying patients who may benefit from preventive measures like implantable cardioverter-defibrillators (ICDs).
Treatment Strategies for Brugada Syndrome
Understanding the current treatment options available is vital for both patients and healthcare professionals. This comprehensive guide will delve into the various strategies employed in treating Brugada Syndrome, emphasizing the role of medication, and exploring advanced treatments like implantable cardioverter-defibrillators (ICDs).
Comprehensive Overview of Current Treatment Options
The management of Brugada Syndrome is multi-faceted, tailored to individual patient needs and the severity of the condition. Treatment strategies primarily aim to prevent sudden cardiac arrest, a major risk associated with this syndrome. Key approaches include:
Lifestyle Adjustments: Patients are advised to avoid certain drugs and situations that may trigger arrhythmias.
Regular Monitoring: Continuous monitoring and regular check-ups help in early detection of potential complications.
Role of Medication in Managing Symptoms
Medication plays a crucial role in the management of Brugada Syndrome, particularly in symptom control. The primary objectives of medical treatment include:
Stabilizing Heart Rhythms: Certain anti-arrhythmic drugs are prescribed to maintain a stable heart rhythm.
Preventing Complications: Medications may also be used to prevent complications associated with arrhythmias.
Advanced Treatments: Implantable Cardioverter-Defibrillators (ICDs) and Their Effectiveness
For patients at high risk of sudden cardiac arrest, advanced treatment options are considered:
Implantable Cardioverter-Defibrillators (ICDs): These devices monitor heart rhythms and deliver electrical shocks when necessary to restore normal rhythm.
Effectiveness of ICDs: ICDs are highly effective in preventing sudden death in high-risk patients, making them a cornerstone in the management of Brugada Syndrome.
However, the treatment of Brugada Syndrome involves a combination of lifestyle modifications, medications, and, in some cases, the use of advanced devices like ICDs. Continuous research and development in this field promise more innovative and effective treatments in the future, enhancing patient care and outcomes.
Lifestyle Considerations and Preventive Measures for Brugada Syndrome
1. Lifestyle Adjustments for Patients with Brugada Syndrome
Living with Brugada Syndrome necessitates certain lifestyle changes to manage the condition effectively. These modifications aim to reduce triggering events and maintain overall health.
Avoid Triggers: Key to managing Brugada Syndrome is avoiding known triggers. This includes certain medications, high fever, and excessive alcohol consumption. Patients should consult their healthcare provider for a comprehensive list of triggers to avoid.
Stay Hydrated and Healthy: Adequate hydration and a balanced diet are crucial. These simple measures can help maintain electrolyte balance, which is essential for heart health.
Exercise Moderation: While regular physical activity is important, intense exercise might pose risks. Patients should discuss safe exercise levels with their physician.
Stress Management: Stress can adversely affect heart health. Engaging in relaxation techniques such as yoga, meditation, or gentle exercises can be beneficial.
2. Preventive Strategies to Reduce Risks and Complications
Implementing preventive strategies can significantly lower the risk of serious complications associated with Brugada Syndrome.
Regular Cardiac Evaluations: Routine check-ups with a cardiologist are vital. These may include ECGs, stress tests, and genetic counseling.
Emergency Plan: Patients should have a clear plan in case of a cardiac event. This includes understanding when and how to seek emergency medical assistance.
Family Screening: Since Brugada Syndrome can be hereditary, screening family members is recommended.
Avoiding Risky Behaviors: Refraining from activities that increase the risk of arrhythmias, such as binge drinking or using recreational drugs, is essential.
3. Importance of Regular Monitoring and Check-Ups
Consistent monitoring plays a pivotal role in the management of Brugada Syndrome.
Routine Health Assessments: Regular health check-ups help in early identification of potential issues and adjustments in treatment plans.
Monitoring Symptoms: Awareness of symptoms like fainting spells, irregular heartbeats, or chest pain is crucial. Any new symptoms should be reported to a healthcare provider immediately.
Device Checks: For patients with implanted devices like pacemakers or defibrillators, regular checks are necessary to ensure proper functioning.
Collaboration with Healthcare Providers: Maintaining open communication with healthcare professionals allows for personalized care and timely adjustments in management strategies.
Adopting these lifestyle considerations and preventive measures can significantly improve the quality of life and reduce risks for individuals with Brugada Syndrome. Regular check-ups and open communication with healthcare providers are essential to manage this condition effectively.
Emerging Research and Future Directions in Brugada Syndrome Treatment
Recent advancements and ongoing research paint a hopeful picture for future treatment methodologies. This article delves into the cutting-edge developments and potential therapeutic approaches that are reshaping the landscape of Brugada Syndrome management.
Recent Advancements in Brugada Syndrome Research
The world of medicine is constantly evolving, and Brugada Syndrome is no exception. Recent years have seen significant breakthroughs in understanding the genetic and molecular basis of this condition. These insights have opened doors to more targeted treatment options. For instance, the identification of specific gene mutations associated with Brugada Syndrome has led to the development of genetic therapies aimed at correcting these anomalies.
Advancements in imaging and diagnostic technologies have also played a crucial role. Enhanced imaging techniques enable earlier and more accurate diagnosis, which is critical for effective treatment. Moreover, the integration of artificial intelligence in diagnostics is proving to be a game-changer, offering faster and more precise analysis of cardiac abnormalities.
Potential Future Treatments for Brugada Syndrome
Looking ahead, the future of Brugada Syndrome treatment is bright with possibilities. One of the most promising areas is gene therapy. As our understanding of the genetic underpinnings of the syndrome improves, so does the potential for therapies that can directly address these genetic issues.
Another area of potential lies in the development of novel pharmacological treatments. Researchers are actively exploring drugs that can more effectively manage the symptoms and prevent the life-threatening cardiac events associated with Brugada Syndrome. These include new anti-arrhythmic drugs and medications that can stabilize heart function.
The Evolving Landscape of Brugada Syndrome Management
The management of Brugada Syndrome is undergoing a transformative phase. The shift is towards a more personalized approach to treatment. Precision medicine, which tailors treatment based on individual genetic makeup, is becoming increasingly relevant. This approach not only improves the efficacy of treatments but also minimizes potential side effects.
In addition to medical treatments, there’s a growing emphasis on lifestyle and dietary modifications as part of the management strategy. Patients are increasingly being advised on specific lifestyle changes that can reduce the risk of triggering the symptoms of Brugada Syndrome.
The field of Brugada Syndrome treatment is on the cusp of significant breakthroughs. With ongoing research and emerging treatments, there’s renewed hope for patients suffering from this challenging condition. The future directions in therapy and management are geared towards more personalized, effective, and safer treatment options, promising a better quality of life for those affected by Brugada Syndrome.
Patient Support and Resources for Brugada Syndrome
Living with this condition can be challenging for patients and their families. However, with the right support and resources, managing this condition becomes more manageable.
1. Support Groups: A Pillar of Strength
Local and Online Communities: These groups offer a platform for sharing experiences, tips, and emotional support. Patients and families can connect with others facing similar challenges, fostering a sense of community and understanding.
Expert-Led Forums: Some support groups are facilitated by healthcare professionals. These forums provide reliable information and guidance on managing Brugada Syndrome.
2. Counseling and Mental Health Support: Essential for Holistic Care
Emotional Well-Being: Counseling services play a vital role in treatment. They address the psychological impact of living with a chronic condition, helping patients cope with anxiety, depression, and stress.
Family Support: Counseling extends to family members, assisting them in understanding the condition and supporting their loved one effectively.
3. Navigating Healthcare Systems for Optimal Care
Coordination of Care: Understanding how to navigate the healthcare system is crucial. This includes knowing how to access specialists, understanding insurance coverage, and managing medical appointments.
Patient Advocacy: Advocacy services can help patients and families voice their needs and rights within the healthcare system, ensuring they receive appropriate and timely care.
4. Educational Resources: Empowering Patients with Knowledge
Informative Literature: Brochures, books, and online articles about Brugada Syndrome help patients and families understand the condition better.
Workshops and Seminars: Educational events led by experts provide deeper insights into treatment options, lifestyle adjustments, and recent advancements in care.
Living with Brugada Syndrome is a journey that requires a network of support. By leveraging support groups, mental health resources, and educational materials, patients and families can navigate this path more confidently. Always remember, you are not alone in this journey.
Conclusion
Effective treatment, typically involving the implementation of an Implantable Cardioverter Defibrillator (ICD), plays a crucial role. This device continually monitors the heart rhythm and delivers electrical shocks when necessary to restore a normal heartbeat. Moreover, pharmacological interventions and lifestyle adjustments contribute significantly to managing this condition.
In addition to these medical interventions, there’s a profound need for heightened awareness and education about Brugada Syndrome. Due to its relatively low prevalence and often asymptomatic nature, many might be unaware of its existence or the risks it poses. Educating the public, healthcare providers, and at-risk individuals about the symptoms, diagnostic procedures, and treatment options is essential. This awareness can lead to early detection, which is instrumental in preventing sudden cardiac arrests and other severe complications.
In summary, the significance of early diagnosis and effective treatment in Brugada Syndrome cannot be overstated. Coupled with increased awareness and education, these measures forge a path toward improved outcomes and the safeguarding of heart health. As we advance in our understanding and management of this condition, it is imperative to remain vigilant and proactive in our approach to combating Brugada Syndrome.