Bronchiolitis Treatment: Bronchiolitis, a common respiratory condition primarily affecting infants and young children, presents a significant challenge in pediatric healthcare.
This comprehensive guide aims to elucidate the nuances of diagnosis and treatment strategies, offering valuable insights for healthcare professionals and caregivers alike.
What is Bronchiolitis?
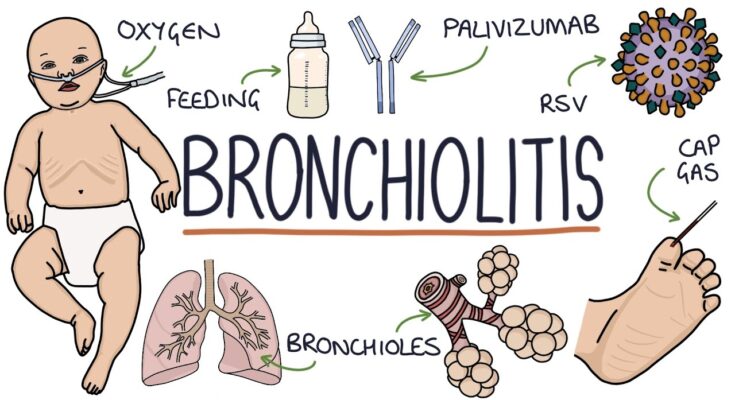
Bronchiolitis is a common respiratory infection affecting young children, primarily infants. It’s characterized by inflammation and congestion in the smallest airways of the lungs, known as bronchioles. This condition often results from a viral infection, most frequently the Respiratory Syncytial Virus (RSV). Bronchiolitis typically manifests with symptoms resembling a common cold, such as a runny nose and cough, but can progress to more severe symptoms like wheezing and difficulty breathing.
Statistics on Prevalence and Demographics Affected
Bronchiolitis is a widespread condition, especially in children under two years of age. It accounts for a significant number of hospital admissions among infants. The majority of children will have encountered an RSV infection by the age of two, with a considerable percentage developing bronchiolitis. The peak incidence of bronchiolitis occurs during the winter months.
Demographically, bronchiolitis tends to affect young infants more severely, with the highest risk group being those under six months of age. Premature infants, children with congenital heart or lung diseases, and those with compromised immune systems are at greater risk of severe bronchiolitis. Additionally, environmental factors like exposure to tobacco smoke and overcrowded living conditions can increase the susceptibility to bronchiolitis.
It’s important for parents and caregivers to be aware of the signs and symptoms of bronchiolitis, especially in high-risk groups, to ensure timely medical intervention. While there is no specific cure, supportive care and symptom management are key to helping affected infants recover.
Causes and Risk Factors of Bronchiolitis
Understanding the causes and risk factors of bronchiolitis is crucial for parents, caregivers, and healthcare providers. This respiratory condition predominantly affects infants and young children, and awareness can lead to better prevention and management strategies.
Common Causes of Bronchiolitis
Bronchiolitis is primarily caused by viral infections. The most common virus responsible is the Respiratory Syncytial Virus (RSV). This virus leads to inflammation and congestion in the small airways (bronchioles) of the lungs, making breathing difficult.
Other viruses that can cause bronchiolitis include:
- Human metapneumovirus.
- Adenoviruses.
- Influenza (flu) virus.
- Parainfluenza virus.
These viruses are highly contagious and spread through droplets when an infected person coughs or sneezes. They can also survive on surfaces, making indirect contact another mode of transmission.
Risk Factors for Developing Bronchiolitis
Certain factors increase the risk of developing bronchiolitis. These include:
Age: Infants between 3 to 6 months old are at the highest risk.
Premature Birth: Babies born prematurely have underdeveloped lungs and immune systems, making them more susceptible.
Weak Immune System: Infants with weakened immune systems, due to a medical condition or treatment, are more vulnerable.
Exposure to Smoke: Exposure to tobacco smoke or other environmental pollutants can increase susceptibility.
Congenital Heart and Lung Diseases: Babies with underlying heart or lung conditions are at increased risk.
Lack of Breastfeeding: Breastfeeding helps to strengthen the immune system. Infants not breastfed may have a higher risk.
Crowded Living Conditions: Living in crowded conditions can facilitate the spread of viruses.
Contact with Multiple Children: Infants in daycare or with older siblings who attend school may have a higher exposure to infectious agents.
By understanding these causes and risk factors, steps can be taken to reduce the likelihood of bronchiolitis in susceptible infants. Preventative measures include regular hand washing, avoiding exposure to sick individuals, and keeping infants away from smoke and crowded places. If you suspect your child has bronchiolitis, it is important to consult a healthcare provider for proper diagnosis and treatment.
Symptoms of Bronchiolitis
Understanding its symptoms is crucial for early detection and timely medical intervention. This guide will outline the common symptoms of bronchiolitis and advise when to seek medical attention.
Common Symptoms of Bronchiolitis
Persistent Coughing: A frequent, dry cough is one of the earliest signs of bronchiolitis. It can last for several days or even weeks.
Wheezing: Wheezing, a high-pitched whistling sound when breathing out, is a hallmark of bronchiolitis. This sound results from narrowed airways due to inflammation.
Fever: Although not always present, a mild fever can accompany bronchiolitis, indicating the body’s effort to fight the infection.
Rapid Breathing: Increased respiratory rate is common. The child may appear to be working harder to breathe, with noticeable use of chest and abdominal muscles.
Nasal Congestion and Runny Nose: These symptoms typically precede the cough and wheezing, and can contribute to breathing difficulties.
Reduced Appetite: Infants and young children may eat less due to difficulty breathing while feeding.
Fatigue and Irritability: Due to the strain on the body from struggling to breathe, children may appear unusually tired or irritable.
When to Seek Medical Attention
Prompt medical evaluation is essential if you observe any of the following:
Difficulty Breathing: If your child is struggling to breathe, breathing rapidly, or you notice a sucking in of muscles around their ribs or neck, seek immediate medical care.
Poor Feeding: In infants, inability to feed or less than half of normal intake over 24 hours, combined with respiratory symptoms, warrants a medical assessment.
Signs of Dehydration: Look for reduced wet diapers, dry mouth, or tearless crying as signs of dehydration.
Persistent High Fever: A fever above 100.4°F (38°C) lasting more than a day should be evaluated by a healthcare provider.
Change in Skin Color: Bluish color around the lips, tongue, or skin indicates a severe lack of oxygen and requires immediate emergency care.
Lethargy or Unresponsiveness: If your child is unusually sleepy, difficult to wake, or unresponsive, seek immediate medical attention.
However, recognizing the symptoms of bronchiolitis and understanding when to seek medical help are key to managing this respiratory condition effectively. Early detection and prompt medical care can significantly improve outcomes for affected children.
Diagnosing Bronchiolitis
Diagnosing bronchiolitis, a common lung infection in young children, involves a combination of clinical evaluation and specific diagnostic methods. Understanding these processes is crucial for parents and caregivers.
List of Diagnostic Methods
Clinical Evaluation: The first step in diagnosing bronchiolitis is a thorough clinical evaluation by a healthcare professional. Symptoms like wheezing, coughing, and difficulty breathing are key indicators.
Physical Examination: During the physical examination, doctors listen to the child’s lungs for signs of wheezing or crackling, which are typical in bronchiolitis.
Oxygen Saturation Test: This non-invasive test measures the oxygen levels in the child’s blood. Low oxygen levels can indicate the severity of bronchiolitis.
Viral Testing: Swab tests from the nose or throat can identify the specific virus causing bronchiolitis, such as the Respiratory Syncytial Virus (RSV).
Chest X-ray: While not always necessary, a chest X-ray can help rule out other conditions, such as pneumonia.
Blood Tests: Occasionally, blood tests are used to assess the overall health and to rule out bacterial infections.
Pulse Oximetry: This test measures how well oxygen is being sent to parts of the body furthest from the heart, like the arms and legs.
The Role of Healthcare Professionals in Diagnosis
Healthcare professionals play a pivotal role in the diagnosis of bronchiolitis. Their expertise is essential in:
Assessing Symptoms: They distinguish between bronchiolitis and other respiratory conditions.
Evaluating Medical History: Understanding a child’s medical history, including any pre-existing conditions, is crucial for accurate diagnosis.
Determining Severity: Based on clinical findings, healthcare professionals can assess the severity of the infection.
Guiding Treatment: After diagnosis, they provide or recommend appropriate treatment and care measures.
Monitoring Progress: Regular follow-ups are important to monitor the child’s recovery and to address any complications.
By collaborating closely with healthcare professionals and understanding the diagnostic process, parents and caregivers can ensure timely and effective treatment for bronchiolitis.
Treatment Options for Bronchiolitis
The treatment of bronchiolitis primarily focuses on relieving symptoms and supporting breathing.
Home Care and Remedies
Home care plays a crucial role in managing bronchiolitis, especially since the condition often resolves on its own. Key home remedies include:
Hydration: Ensuring the child stays well-hydrated is essential, as fluids help loosen mucus in the lungs.
Rest: Adequate rest is vital for recovery.
Humidified Air: Using a cool-mist humidifier can help ease breathing by moistening the dry air.
Nasal Suction: Using a bulb syringe or nasal aspirator to clear nasal congestion can be particularly helpful before feeding and bedtime.
Parents and caregivers should closely monitor the child’s breathing and feeding, and consult a healthcare provider if symptoms worsen.
Medications and Medical Interventions
In more severe cases, medical interventions may be necessary:
Bronchodilators: Though not routinely recommended, bronchodilators like albuterol may be used in some cases to open up airways.
Steroids: Not typically recommended for bronchiolitis, but may be considered in certain situations.
Oxygen Therapy: For children with significant breathing difficulty, supplemental oxygen might be required.
Hospitalization: In severe cases, particularly for infants, hospitalization might be necessary to provide supportive care such as hydration and oxygen therapy.
It’s important to note that antibiotics are not effective against bronchiolitis unless there is a coexisting bacterial infection.
Discussion on the Effectiveness of Different Treatments
The effectiveness of bronchiolitis treatments varies:
Home Remedies: Often sufficient for mild cases and are crucial for comfort and symptom management.
Medications: The use of medications like bronchodilators is debated among professionals. They may provide temporary relief in some cases but are not a cure.
Medical Interventions: Necessary for severe cases, and their effectiveness is generally high in terms of supporting vital functions and preventing complications.
Overall, the treatment of bronchiolitis is supportive and symptomatic, with a focus on ensuring the child is comfortable, well-hydrated, and able to breathe effectively. Parents and caregivers should consult healthcare professionals for guidance tailored to the child’s specific needs.
Prevention Strategies for Bronchiolitis
There are several effective strategies to prevent this illness. This section highlights the importance of vaccinations and hygiene practices in safeguarding children against bronchiolitis.
1. Understanding the Significance of Vaccinations: Vaccinations play a pivotal role in preventing bronchiolitis, especially for infants and young children. The Synagis vaccine, for example, is specifically designed to protect high-risk infants from severe respiratory syncytial virus (RSV), a leading cause of bronchiolitis. Parents should consult with their pediatrician to ensure their child’s vaccinations are up-to-date.
2. Rigorous Hygiene Practices: The transmission of viruses that cause bronchiolitis can be significantly reduced through diligent hygiene practices. Key measures include:
- Regular Hand Washing: Frequent and thorough hand washing is crucial. Parents, caregivers, and children should wash hands with soap and water for at least 20 seconds, especially after coughing, sneezing, or touching public surfaces.
- Avoiding Exposure to Sick Individuals: Keep infants and young children away from people who are sick. Viruses that cause bronchiolitis are highly contagious and can easily spread from person to person.
- Cleaning and Disinfecting Surfaces: Regularly clean and disinfect toys, doorknobs, and other frequently touched surfaces to prevent the spread of germs.
3. Maintaining a Healthy Environment: A clean and smoke-free environment is essential. Exposure to tobacco smoke can increase the risk of developing bronchiolitis and other respiratory infections.
4. Breastfeeding When Possible: Breastfeeding can strengthen an infant’s immune system, providing added protection against respiratory infections like bronchiolitis.
By implementing these prevention strategies, parents and caregivers can significantly reduce the risk of bronchiolitis in young children. It’s important to stay informed and proactive in safeguarding the health of our little ones. Remember, prevention is always better than cure.
Complications and Long-Term Effects of Bronchiolitis
Understanding these potential complications and the long-term outlook for patients is crucial for caregivers and healthcare professionals.
Potential Complications of Untreated or Severe Bronchiolitis
Respiratory Distress: Severe bronchiolitis can cause significant breathing difficulties, necessitating medical interventions like oxygen therapy or mechanical ventilation.
Dehydration: Infants with bronchiolitis might eat and drink less due to breathing difficulties, leading to dehydration, a condition requiring prompt medical attention.
Secondary Infections: Untreated bronchiolitis can make children more susceptible to secondary infections like pneumonia, which can further complicate their health status.
Apnea: Particularly in very young infants, bronchiolitis can lead to apnea, a condition where the child experiences pauses in breathing.
Chronic Respiratory Problems: There’s a risk that severe bronchiolitis in infancy could lead to long-term respiratory issues, such as asthma or chronic obstructive pulmonary disease (COPD) in later life.
Long-Term Outlook for Patients with Bronchiolitis
The majority of children with bronchiolitis recover completely with no long-term health effects. However, some may experience recurrent wheezing or develop asthma-like symptoms, particularly if they had severe bronchiolitis or required hospitalization. Regular follow-ups with a pediatrician can help monitor and manage any ongoing or emerging respiratory issues.
Early intervention and appropriate treatment are key in minimizing the risks associated with bronchiolitis. Parents and caregivers should seek medical advice if they notice any signs of breathing difficulties, dehydration, or other concerning symptoms in their child.
Recent Advances in Bronchiolitis Treatment
Let’s delves into the latest breakthroughs and future directions in the care and management of bronchiolitis, offering valuable insights for healthcare professionals, researchers, and families alike.
Breakthroughs in Treatment and Research
Innovative Medications: Recent years have witnessed the development of new medications that target specific pathways involved in bronchiolitis. These include antiviral drugs and novel anti-inflammatory agents, which have shown promise in reducing the severity and duration of the illness.
Enhanced Respiratory Support: Advances in respiratory support techniques, such as high-flow nasal cannula (HFNC) oxygen therapy, have significantly improved the management of severe bronchiolitis cases. This non-invasive method enhances oxygen delivery and reduces the need for mechanical ventilation.
Vaccine Development: Though still in the experimental phase, vaccines against the common causes of bronchiolitis, like Respiratory Syncytial Virus (RSV), are under development. This preventive approach could drastically reduce the incidence and severity of bronchiolitis in the future.
Genetic and Biomarker Research: Cutting-edge research is focusing on identifying genetic markers and biomarkers that can predict the severity of bronchiolitis in individual patients. This personalized approach could lead to more tailored and effective treatments.
Telemedicine and Home Monitoring: The rise of telemedicine has enabled remote monitoring and consultation for bronchiolitis patients, reducing the burden on healthcare facilities and allowing for timely interventions.
Future Directions in Bronchiolitis Care
Personalized Medicine: The future of bronchiolitis treatment lies in personalized medicine. Utilizing genetic information and individual health profiles, treatments can be customized for more effective and efficient patient care.
Integrated Care Pathways: Developing integrated care pathways that encompass prevention, early detection, and comprehensive treatment strategies is key to improving outcomes in bronchiolitis patients.
Community Awareness and Education: Enhancing community awareness and education about bronchiolitis, its prevention, and early signs is crucial. This can lead to earlier detection and treatment, thereby reducing complications.
Advanced Immunotherapy: Research into advanced immunotherapies, focusing on modulating the immune response in bronchiolitis, is a promising area that could lead to breakthrough treatments.
Global Collaboration in Research: Fostering global collaboration in bronchiolitis research can accelerate the development of new treatments and share best practices across different healthcare systems.
However, the landscape of bronchiolitis treatment is evolving rapidly, with new research and treatment methods offering hope for better management and outcomes. The future direction of bronchiolitis care is geared towards more personalized, efficient, and preventive strategies, paving the way for a significant impact on child health worldwide.
Frequently Asked Questions About Bronchiolitis
1. What is Bronchiolitis?
Bronchiolitis is a common respiratory infection in infants and young children. It’s typically caused by a virus and affects the small airways in the lungs, leading to symptoms like coughing, wheezing, and difficulty breathing.
2. How is Bronchiolitis Transmitted?
The infection spreads through respiratory droplets when an infected person coughs or sneezes. It can also be transmitted by touching contaminated surfaces and then touching the face, especially the nose or mouth.
3. What Are the Symptoms of Bronchiolitis?
Symptoms include a runny nose, cough, mild fever, and wheezing. In severe cases, the child might experience difficulty breathing and decreased appetite.
4. When Should I Seek Medical Attention for Bronchiolitis?
Consult a healthcare provider if your child has difficulty breathing, is not drinking enough fluids, or if symptoms worsen. Immediate medical attention is crucial if the child shows signs of severe respiratory distress.
5. How is Bronchiolitis Diagnosed?
A healthcare provider will diagnose bronchiolitis based on the child’s symptoms and a physical examination. In some cases, tests like a chest X-ray or a nasal swab may be necessary.
6. What are the Treatment Options for Bronchiolitis?
Treatment mainly focuses on relieving symptoms. This may include hydration, nasal suctioning, and in some cases, hospitalization for oxygen therapy or more intensive care.
7. Can Bronchiolitis be Prevented?
Preventive measures include frequent handwashing, avoiding close contact with sick individuals, and cleaning and disinfecting surfaces. Vaccinations for certain viruses can also reduce the risk.
8. Is Bronchiolitis Contagious?
Yes, bronchiolitis is contagious. It’s most commonly spread during the cold and flu season.
9. Can Adults Get Bronchiolitis?
While it’s more common in infants and young children, adults, especially those with weakened immune systems, can also contract bronchiolitis.
10. How Long Does Bronchiolitis Last?
The illness usually peaks around the third to fifth day after symptoms begin and gradually improves over the next week. However, some children may have a lingering cough for several weeks.
Conclusion
While this guide provides a comprehensive overview, it’s crucial to remember that it cannot replace professional medical advice. Each child is unique, and their response to treatment may vary. Therefore, if you suspect your child is showing symptoms of bronchiolitis, or if you have any concerns about their respiratory health, it is imperative to consult a healthcare professional. They can provide personalized advice and treatment plans suited to your child’s specific needs.
In conclusion, being well-informed about bronchiolitis, its symptoms, diagnosis, and treatment options, is invaluable. However, the cornerstone of managing this condition lies in professional medical consultation and following their expert guidance. Stay vigilant, stay informed, and always prioritize your child’s health by seeking professional advice when needed.