Amyotrophic Lateral Sclerosis Symptoms: Amyotrophic Lateral Sclerosis (ALS), often known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that affects nerve cells in the brain and the spinal cord. It leads to the gradual deterioration and death of motor neurons, which are essential for controlling voluntary muscle movement.
Understanding ALS is crucial because it helps in early detection and management of the disease. This overview highlights the importance of familiarizing oneself with the symptoms and causes of ALS, paving the way for better treatment approaches and supportive care for those affected.
Knowledge of ALS not only aids in medical intervention but also fosters a supportive environment for patients and their families, underlining the significance of awareness in combating this challenging condition.
Symptoms of Amyotrophic Lateral Sclerosis
1. Early Symptoms of Amyotrophic Lateral Sclerosis:
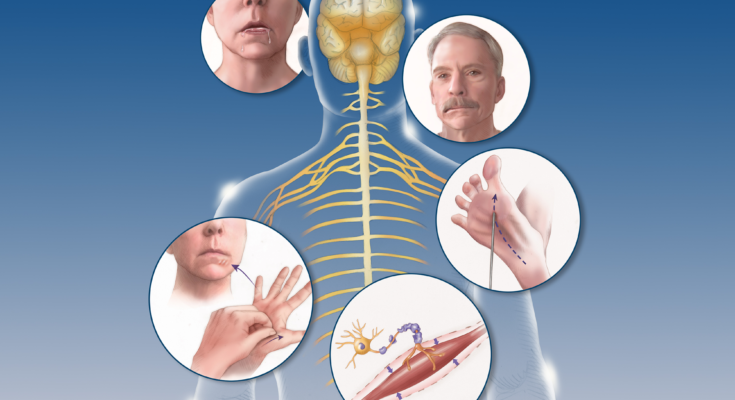
Amyotrophic Lateral Sclerosis (ALS) often begins subtly, but these initial symptoms are critical indicators. The early signs include:
- Muscle Weakness: It usually starts in the hands, feet, or limbs, and gradually progresses. This weakness often leads to clumsiness, difficulty with fine motor skills, and trouble performing everyday tasks.
- Muscle Twitching and Cramps: Before significant weakness sets in, patients may notice twitching and cramping of muscles, particularly in the hands and feet.
- Speech Changes: Some people experience slurred speech or difficulty projecting their voice.
- Difficulty Swallowing or Chewing: As the muscles around the mouth and throat weaken, swallowing can become a challenge.
2. Progression of Amyotrophic Lateral Sclerosis Symptoms:
As ALS progresses, symptoms become more pronounced and widespread:
- Increased Muscle Weakness: This can lead to difficulties in walking, moving the arms, and performing daily activities.
- Breathing Difficulties: As respiratory muscles weaken, breathing becomes labored, leading to a need for ventilatory support in advanced stages.
- Eating and Nutrition Challenges: Swallowing difficulties may require dietary modifications or feeding tubes in later stages.
- Communication Barriers: Speech may become increasingly difficult, necessitating alternative communication methods.
3. Variability of Amyotrophic Lateral Sclerosis Symptoms:
ALS symptoms can vary significantly from person to person:
- Onset Location Variability: While some might experience initial weakness in the limbs, others might start with speech or swallowing difficulties.
- Symptom Progression Rate: The rate at which ALS progresses can vary widely, with some experiencing rapid progression and others having a slower course.
- Differences in Symptom Severity: The severity of symptoms like muscle weakness, respiratory issues, and communication challenges can differ greatly among individuals.
By understanding the symptoms of Amyotrophic Lateral Sclerosis in detail, patients and caregivers can better manage the condition and prepare for its progression. Each symptom of ALS plays a critical role in the overall impact of the disease, making awareness and early recognition vital for effective management and care.
Causes of Amyotrophic Lateral Sclerosis
While the exact cause of ALS remains largely unknown, research has identified several factors that may contribute to its development.
Genetic Factors: In about 5-10% of cases, ALS is inherited, known as familial ALS. This form of the disease is caused by mutations in specific genes, such as the C9orf72, SOD1, FUS, and TARDBP genes. Understanding these genetic mutations can offer valuable insights into the mechanisms of ALS.
Environmental Triggers: While the majority of ALS cases are sporadic, meaning they occur at random with no identifiable cause, some environmental factors may increase the risk. These include smoking, exposure to certain chemicals or heavy metals, and possibly viral infections.
Age and Gender: ALS is more common in people aged between 40 and 70 years, with a slightly higher prevalence in men compared to women. However, it can occur at any age.
Cellular Dysfunction: Researchers are exploring how cellular processes like protein mishandling, mitochondrial dysfunction, and glutamate toxicity contribute to the death of neurons in ALS.
Immune System Involvement: There is growing evidence that the immune system may play a role in ALS, possibly through inflammation that damages neurons.
Lifestyle Factors: Some studies suggest that certain lifestyle factors, such as physical activity or dietary habits, might influence the risk of developing ALS, though more research is needed in this area.
However, ALS is a complex condition with multiple potential causes. Ongoing research continues to explore these factors to better understand the disease and develop effective treatments.
Diagnosing Amyotrophic Lateral Sclerosis (ALS)
Diagnosing Amyotrophic Lateral Sclerosis (ALS), a progressive neurodegenerative disease, is a complex process.
Diagnostic Criteria for ALS
Understanding the diagnostic criteria for ALS is crucial. Doctors primarily look for signs of progressive muscle weakness and atrophy, typically starting in one part of the body and spreading. They also consider the presence of upper and lower motor neuron signs during neurological examinations. It’s important to note that ALS is often diagnosed by ruling out other conditions, as there is no single test for it. This section should delve into the specific symptoms and signs that healthcare professionals watch for, such as difficulty in speaking, swallowing, and muscle cramps.
Tests and Procedures Used in Diagnosing ALS
There are several tests and procedures commonly used to diagnose or rule out ALS. These include:
- Electromyography (EMG) and Nerve Conduction Studies: These tests measure the electrical activity of muscles and the nerves that control them.
- Magnetic Resonance Imaging (MRI): An MRI can reveal spinal cord and brain abnormalities that might suggest other diseases.
- Blood and Urine Tests: These help rule out other potential causes of symptoms.
- Lumbar Puncture (Spinal Tap): This test checks the fluid surrounding the brain and spinal cord for abnormalities.
- Muscle Biopsy: Although less common, a muscle biopsy can help rule out other muscle diseases.
Detailing these tests helps readers understand the comprehensive approach taken to diagnose ALS accurately.
Challenges in Diagnosing ALS
Diagnosing ALS can be challenging due to several factors:
- Symptom Overlap with Other Conditions: Symptoms of ALS often resemble those of other neurological disorders, which can lead to misdiagnosis.
- No Definitive Test: Since there is no single test for ALS, diagnosis is often a process of elimination.
- Variable Progression: The rate at which ALS progresses can vary greatly among individuals, complicating the diagnostic process.
This section should emphasize the importance of seeking a specialist, such as a neurologist, for accurate diagnosis and the potential for misdiagnosis due to these challenges.
Living with Amyotrophic lateral sclerosis (ALS)
Living with Amyotrophic Lateral Sclerosis (ALS) presents unique challenges and requires significant adjustments to one’s lifestyle. ALS, often referred to as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that affects nerve cells in the brain and spinal cord, leading to muscle weakness and atrophy.
Daily Life Adjustments
Those living with ALS will need to make several adjustments to their daily life. This can include:
- Mobility Assistance: As muscle weakness increases, mobility aids like wheelchairs or walkers become necessary.
- Speech Therapy: Difficulty in speaking may arise, making speech therapy an important aspect of ALS care.
- Dietary Changes: Swallowing difficulties might require dietary modifications or the use of feeding tubes in advanced stages.
- Home Modifications: To accommodate mobility issues, homes may need to be modified for easier access and safety.
Emotional and Mental Health
Living with ALS can be emotionally challenging. Patients and their families often face anxiety, depression, and stress. Seeking support from mental health professionals, support groups, and counseling can be beneficial.
Medical Care
There is no cure for ALS, but treatments can slow its progression and manage symptoms. Medications like Riluzole can extend survival and quality of life. Regular check-ups with neurologists and other specialists are crucial.
Support Systems
A strong support system is vital. This includes family, friends, healthcare professionals, and ALS support groups. These networks provide emotional support, practical help, and information about living with ALS.
Staying Active and Engaged
Remaining engaged in activities and hobbies as much as possible is important for mental health. Adapting hobbies to fit physical abilities can help maintain a sense of normalcy and fulfillment.
Planning for the Future
Advance care planning is essential. This involves discussing and documenting healthcare preferences and making legal arrangements for future care and decision-making.
Living with ALS is challenging, but with the right support and adjustments, individuals can maintain quality of life. It’s important to focus on what can be done, seek help when needed, and cherish every moment.
Preparing for your appointment
Your primary care provider may be the first to recognize the symptoms of ALS. Your provider will likely refer you to a doctor trained in nervous system conditions, known as a neurologist, to establish a diagnosis.
What you can do
You might need many tests to diagnose your condition. The diagnosis process can be stressful and frustrating. These strategies might give you a greater sense of control.
- Keep a symptom diary. Before you see a neurologist, start using a calendar or notebook to jot down when and how you notice symptoms. Record information about your problems with walking, hand coordination, speech, swallowing or involuntary muscle movements. Your notes might show a pattern that’s helpful for your diagnosis.
- Find a neurologist and care team. An integrated care team led by your neurologist usually is most appropriate for ALS care. Your team typically communicates with each other and is familiar with your needs.
What to expect from your doctor
Your primary care provider will likely review your family’s medical history and your symptoms. Your neurologist and your primary care provider might conduct a physical and neurological exam. This might include testing your:
- Reflexes.
- Muscle strength.
- Muscle tone.
- Senses of touch and sight.
- Coordination.
- Balance.
Conclusion
ALS is a complex condition with significant physical and emotional impacts. Understanding the symptoms and causes, coupled with a robust support system and ongoing research, is vital for those affected by this disease. While the journey with ALS is challenging, advancements in care and treatment continue to offer hope.