Epilepsy Symptoms: Epilepsy stands as a central nervous system (neurological) disorder where brain activity becomes abnormal, causing seizures or periods of unusual behavior, sensations, and sometimes loss of awareness.
Anyone can develop epilepsy; it affects both males and females of all races, ethnic backgrounds, and ages.
Understanding Epilepsy
Epilepsy stands as a neurological condition characterized by recurring seizures. These seizures are the result of sudden, excessive electrical discharges in the brain’s neurons. This can lead to various symptoms, including convulsions, sensory disturbances, or loss of consciousness. Epilepsy affects individuals across all age groups, ethnic backgrounds, and geographical locations, marking it as a universal health concern.
Definition and Overview
Epilepsy is more than just a single condition; it is a spectrum of disorders with seizures that vary from brief lapses of attention or muscle jerks to severe and prolonged convulsions. Seizures can also vary in frequency, from less than one per year to several per day. It is important to note that having a single seizure does not necessarily mean one has epilepsy—typically, at least two unprovoked seizures are required for diagnosis.
The causes of epilepsy are diverse and can include genetic factors, brain trauma, stroke, infections, and more. In many cases, however, the exact cause remains unknown, making diagnosis and treatment a challenge for healthcare professionals.
Statistics on Prevalence and Demographics Affected
Epilepsy is a widespread condition, affecting approximately 50 million people worldwide, according to the World Health Organization (WHO). It’s one of the most common neurological diseases globally, touching the lives of men and women equally. While epilepsy can manifest at any age, it is most commonly diagnosed in children and individuals over the age of 65, suggesting a pattern linked to the developmental and degenerative processes of the brain.
In the United States alone, about 3.4 million people live with epilepsy, with an estimated 150,000 new cases diagnosed each year, highlighting its significant impact on public health. The prevalence of epilepsy is slightly higher in developing countries, which could be attributed to the increased risks of endemic diseases, such as malaria and neurocysticercosis, that can lead to seizures.
Epilepsy does not discriminate—it affects individuals of all racial and ethnic backgrounds. However, the incidence rates, access to treatment, and outcomes can vary significantly across different demographic groups, influenced by socio-economic factors, healthcare availability, and cultural stigmas associated with the condition.
However, understanding epilepsy is crucial for demystifying the condition, improving the lives of those affected, and advancing towards more effective treatments. Awareness and education can foster a more supportive environment for individuals living with epilepsy, encouraging early diagnosis and proper management of the condition.
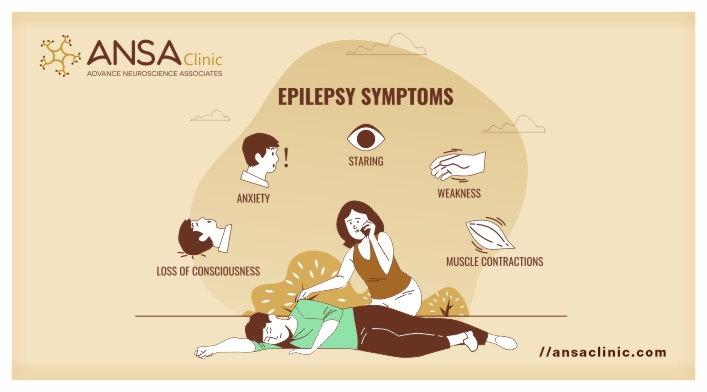
Symptoms of Epilepsy
Symptoms can vary significantly among individuals, depending on the type of epilepsy and the area of the brain affected. Recognizing the symptoms is crucial for early diagnosis and effective management of the condition. This article delves into the primary symptoms of epilepsy, highlights less common symptoms, and explores the differences in symptoms between children and adults.
Primary Symptoms of Epilepsy
The primary symptom of epilepsy is recurrent seizures. However, the nature of these seizures can vary, including:
- Generalized Seizures: These affect both sides of the brain and can cause muscle spasms, loss of consciousness, or falls.
- Focal Seizures: Originating in just one part of the brain, these seizures may involve involuntary jerking of a body part, changes in sensation, dizziness, or even emotional changes without loss of consciousness.
- Absence Seizures: Often mistaken for daydreaming, absence seizures cause brief lapses in awareness, typically in children.
Understanding that seizures manifest in various forms is key to recognizing epilepsy. Some individuals may experience staring spells, while others may have violent shaking or loss of bladder control.
Recognizing Less Common Symptoms
Beyond the primary symptoms, epilepsy can manifest through less common signs that are often overlooked, including:
- Auras: These are sensory changes that precede a seizure, such as a feeling of déjà vu, unusual smells, or a rising sensation in the stomach.
- Postictal Symptoms: After a seizure, individuals may experience confusion, fatigue, headache, or mood changes, known as postictal symptoms.
- Psychogenic Non-Epileptic Seizures (PNES): These seizures mimic epileptic seizures but are not caused by electrical disruptions in the brain and can be a symptom of underlying psychological issues.
Identifying these less common symptoms can aid in diagnosing epilepsy and differentiating it from other conditions.
Symptoms in Children vs. Adults: Are They Different?
The manifestation of epilepsy symptoms can vary significantly between children and adults, influenced by factors such as the developmental stage of the brain and the type of epilepsy.
- Children: Symptoms in children may include sudden falls (atonic seizures), staring spells (absence seizures), or rapid jerking movements (myoclonic seizures). Children may also exhibit behavioral changes, such as becoming unusually irritable or experiencing learning difficulties.
- Adults: While adults can experience similar types of seizures, they are more likely to report auras or postictal confusion. In adults, focal seizures are more common, and seizures may be triggered by stress, lack of sleep, or alcohol consumption.
Understanding these age-related differences is crucial for accurate diagnosis and treatment. Early recognition and intervention can significantly improve the quality of life for individuals with epilepsy.
Furthermore, acknowledging the differences in symptoms between children and adults can aid in tailoring treatment approaches. If you or someone you know is experiencing symptoms of epilepsy, it’s important to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
Causes of Epilepsy: Understanding the Factors
Understanding these causes is crucial for effective diagnosis and treatment. Below, we delve into the major factors contributing to epilepsy, including genetic influences, brain conditions, infectious diseases, developmental disorders, and other potential triggers.
Genetic Influences: When Epilepsy Runs in Families
Research shows that genetics play a pivotal role in many cases of epilepsy. When epilepsy runs in families, it indicates a genetic predisposition to the condition. Genetic epilepsy often arises from mutations or alterations in genes responsible for the functioning of neurons in the brain. These genetic variations can affect the brain’s electrical activity, leading to seizures. However, it’s important to note that having a family member with epilepsy does not guarantee that others in the family will inherit the condition, but it does increase the risk.
Brain Conditions: Tumors, Strokes, and Traumatic Brain Injuries
Brain conditions such as tumors, strokes, and traumatic brain injuries are significant contributors to the onset of epilepsy. These conditions can cause damage to the brain’s structure, leading to the development of abnormal electrical activity that results in seizures. Strokes, for instance, are a leading cause of epilepsy in adults over the age of 35. Similarly, traumatic brain injuries from accidents or physical trauma can disrupt the normal functioning of brain cells and increase the likelihood of epilepsy.
Infectious Diseases: Meningitis, Viral Encephalitis, and Their Impact
Infectious diseases like meningitis (an inflammation of the membranes surrounding the brain and spinal cord) and viral encephalitis (inflammation of the brain caused by a virus) can also cause epilepsy. These infections can lead to brain damage, making the brain more susceptible to seizures. Early treatment of these infectious diseases is critical in reducing the risk of developing epilepsy.
Developmental Disorders and Epilepsy: Autism Spectrum Disorder and Neurofibromatosis
Developmental disorders, including autism spectrum disorder (ASD) and neurofibromatosis, have been linked to an increased risk of epilepsy. These conditions involve abnormal brain development, which can contribute to the onset of seizures. For example, individuals with neurofibromatosis, a genetic disorder that causes tumors to form on nerve tissue, may experience seizures as a symptom of the disease.
Other Potential Triggers: Lifestyle and Environmental Factors
In addition to genetic and medical conditions, lifestyle and environmental factors can act as triggers for epilepsy. These may include sleep deprivation, alcohol intake, stress, and exposure to certain chemicals or pollutants. While not direct causes of epilepsy, these factors can exacerbate the condition or increase the frequency of seizures in individuals who are already predisposed to epilepsy.
From genetic predispositions and brain conditions to infectious diseases and developmental disorders, the causes of epilepsy are diverse. Recognizing these factors is crucial for diagnosis, treatment, and management of the condition. If you or someone you know is experiencing symptoms of epilepsy, it’s important to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Diagnosing Epilepsy: A Comprehensive Guide
Understanding the steps involved in diagnosing epilepsy is crucial for individuals experiencing seizures and their families. This article outlines the critical stages of epilepsy diagnosis, including medical history evaluation, symptom analysis, and advanced diagnostic tests.
Medical History and Symptom Analysis
The initial step in diagnosing epilepsy involves a detailed review of the patient’s medical history and a thorough analysis of their symptoms. This process is pivotal as it helps healthcare professionals distinguish epileptic seizures from other conditions that might mimic epilepsy, such as fainting spells or panic attacks. Patients are encouraged to provide comprehensive information about their seizure episodes, including:
- The frequency and duration of seizures.
- Specific triggers that might provoke seizures, such as lack of sleep or stress.
- Any noticeable signs that precede the seizures, known as aura.
- Family history of epilepsy or other neurological disorders.
This information is critical for doctors to form a preliminary understanding of the patient’s condition and decide on further diagnostic steps.
Tests and Procedures: EEG, MRI, and Beyond
Following the initial evaluation, several diagnostic tests and procedures are employed to confirm the presence of epilepsy and to determine its type and cause. The most common diagnostic tools include:
Electroencephalogram (EEG)
An EEG is the most commonly used test for diagnosing epilepsy. This non-invasive procedure records the electrical activity of the brain. Patients may be asked to perform specific tasks or be exposed to certain stimuli during the EEG to provoke brain activity that might reveal patterns indicative of epilepsy. In some cases, a prolonged EEG monitoring over several days might be necessary.
Magnetic Resonance Imaging (MRI)
An MRI scan provides detailed images of the brain, helping doctors identify structural abnormalities that could be causing seizures. This high-resolution imaging test is particularly useful in detecting conditions such as brain tumors, cysts, or scars, which could be at the root of epileptic seizures.
Beyond EEG and MRI
While EEG and MRI are pivotal in the epilepsy diagnostic process, additional tests might be required to gather more information:
- Blood tests can help identify signs of infections, genetic conditions, or metabolic disorders that might be contributing to seizures.
- Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT) scans are specialized imaging tests that can highlight areas of the brain that are not functioning normally.
- Neuropsychological tests assess the impact of epilepsy on cognitive functions and help tailor treatment plans to address these challenges.
However, diagnosing epilepsy is a multifaceted process that requires a combination of medical history evaluation, symptom analysis, and specialized diagnostic tests. Understanding this process can empower patients and their families as they navigate the path to an accurate diagnosis and effective treatment. With advances in medical technology and diagnostics, the accuracy of epilepsy diagnosis continues to improve, offering hope for better management and outcomes for those affected by this condition.
Treatment Options for Epilepsy
Managing epilepsy effectively involves a multifaceted approach tailored to each patient’s specific needs. This article explores the primary treatment options for epilepsy, including medications, surgical interventions, lifestyle adjustments, and the promising future of epilepsy research.
Medications: First-line Treatments and Considerations
Antiepileptic drugs (AEDs) are the cornerstone of epilepsy treatment. These medications aim to reduce the frequency and severity of seizures by stabilizing electrical activity in the brain. The choice of AED depends on several factors, including the type of seizures, the patient’s age, potential side effects, and whether the patient is pregnant or planning to become pregnant. While many individuals achieve seizure control with their first or second medication, others may require a combination of drugs. It’s crucial for patients to work closely with their healthcare provider to find the most effective and tolerable medication regimen.
Surgical Interventions: When Medication Isn’t Enough
For approximately 20-30% of patients, medications alone do not adequately control seizures. In such cases, surgical intervention may be considered. Surgical options include resective surgery, which involves removing the brain area where seizures originate, and neurostimulation, which uses devices to alter electrical activity in the brain. The candidacy for epilepsy surgery is determined after a comprehensive evaluation, including detailed imaging and monitoring of brain activity. Surgery can offer a significant improvement in quality of life for those who are eligible.
Lifestyle Adjustments and Alternative Therapies
In addition to medical and surgical treatments, lifestyle adjustments can play a crucial role in managing epilepsy. Patients are advised to maintain a regular sleep schedule, avoid known triggers, and limit alcohol consumption. Stress-reducing techniques such as yoga and meditation may also benefit some individuals. Dietary therapies, like the ketogenic diet, have shown efficacy in reducing seizures, especially in children. While alternative therapies can complement traditional treatments, they should not replace them. Patients should discuss all lifestyle changes and alternative therapies with their healthcare provider.
The Future of Epilepsy Treatment: Research and New Horizons
The future of epilepsy treatment is bright, with ongoing research exploring innovative therapies and technologies. Advances in genetic research are helping to identify the underlying causes of epilepsy, paving the way for personalized medicine approaches. Novel drug therapies and improvements in neurostimulation devices continue to emerge, offering hope to those for whom traditional treatments have been unsuccessful. Additionally, the exploration of regenerative medicine and cell therapy holds the potential to repair or replace damaged brain cells, representing a frontier in epilepsy treatment.
However, managing epilepsy requires a comprehensive treatment strategy that may include medications, surgical interventions, lifestyle adjustments, and alternative therapies. With ongoing research and the development of new treatments, the outlook for individuals with epilepsy continues to improve. Patients should work closely with their healthcare team to determine the most effective treatment plan for their unique situation.
Managing Life with Epilepsy
Living with epilepsy presents unique challenges, but with the right coping strategies and support systems, individuals can lead fulfilling lives. This guide explores practical tips for managing epilepsy, its impact on daily life, and the resources available for patients and their families.
Coping Strategies and Support Systems
Develop a Support Network: Building a strong support network of family, friends, and healthcare professionals can provide emotional and practical assistance. Support groups, both in-person and online, connect individuals with epilepsy, offering a platform to share experiences and advice.
Maintain a Healthy Lifestyle: A balanced diet, regular exercise, and sufficient sleep can help manage epilepsy symptoms. Stress reduction techniques such as meditation, yoga, or deep breathing exercises can also be beneficial.
Educate Yourself and Others: Understanding epilepsy can empower you to manage your condition better. Educate those around you to help them understand your condition and how they can support you during a seizure.
Medication Management: Adhering to prescribed medication schedules is crucial. Use reminders or apps to keep track of your medication timings and dosages.
Seizure Tracking and Management: Keeping a seizure diary can help identify triggers and patterns, aiding in better management of the condition. Share this diary with your healthcare provider to adjust treatment plans as necessary.
Impact on Daily Life
Driving: Regulations regarding driving vary by location but generally require a period of being seizure-free. Familiarize yourself with the laws in your area and discuss your condition with healthcare professionals to understand your options.
Employment: People with epilepsy are protected under disability laws in many countries, which means employers must provide reasonable accommodations. Be open about your condition with your employer to ensure your work environment is safe and supportive.
Education: Students with epilepsy may require special accommodations to manage their condition. Schools and universities often provide services like note-taking assistance, extra time for exams, or the ability to record lectures.
Resources and Support for Patients and Families
Epilepsy Foundations and Organizations: Many countries have foundations and organizations dedicated to epilepsy research and support. These organizations offer educational materials, advocacy, and support group information.
Healthcare Providers: Neurologists and epilepsy specialists can provide medical advice, treatment options, and referrals to other resources such as counseling or rehabilitation services.
Online Resources: Websites and online forums offer a wealth of information and support for individuals with epilepsy and their families. These platforms allow for sharing experiences and advice with others facing similar challenges.
Educational Workshops and Seminars: Participating in workshops and seminars can provide valuable information on managing epilepsy, understanding treatment options, and living a healthy lifestyle.
Managing life with epilepsy involves navigating various challenges, but with the right strategies and support, individuals can achieve a high quality of life. By leveraging resources and fostering a supportive network, people with epilepsy can thrive in all aspects of their lives.
FAQs on Epilepsy
What is Epilepsy?
Epilepsy is a chronic disorder of the brain that is marked by an enduring predisposition to generate epileptic seizures. These seizures are episodes of disturbed brain activity that can cause changes in attention, behavior, or consciousness.
What Causes Epilepsy?
Epilepsy can stem from various causes, including genetic predisposition, head trauma, brain conditions like stroke or tumors, infectious diseases, prenatal injury, and developmental disorders. However, for about 50% of cases, the exact cause remains unknown.
How is Epilepsy Diagnosed?
Diagnosis typically involves a thorough medical history review and diagnostic tests such as Electroencephalogram (EEG), Magnetic Resonance Imaging (MRI), and blood tests to help identify seizures and their origins.
Can Epilepsy be Treated?
Yes, epilepsy can be managed with treatment. While not all epilepsies can be cured, many people with epilepsy lead full, unrestricted lives. Treatment options include medications (antiepileptic drugs), surgical procedures, neurostimulation, and dietary changes, tailored to the individual’s needs.
Is Epilepsy Common?
Epilepsy is one of the most common neurological conditions globally. It is estimated that around 50 million people worldwide have epilepsy, with millions more impacted indirectly as family members or caregivers.
Can People with Epilepsy Lead Normal Lives?
Absolutely. With proper diagnosis, treatment, and management, most people with epilepsy can perform daily activities and achieve their personal and professional goals. Adjustments and precautions might be necessary depending on the frequency and severity of seizures.
Are Seizures Always Obvious?
No, seizures manifest in various ways, from convulsions and loss of consciousness to subtle changes like blank staring, lip-smacking, or jerking movements of arms and legs. The type of seizure depends on the area of the brain affected.
Is There a Cure for Epilepsy?
There’s no one-size-fits-all answer to this. Some individuals may outgrow their seizures or achieve seizure freedom through treatment. However, epilepsy is a chronic condition, and while it can be managed, a cure is not available for everyone.
What Should You Do If Someone Is Having a Seizure?
Safety is paramount. Keep the person safe from harm, place them on their side to help keep their airway clear, and stay with them until the seizure ends. Avoid putting anything in their mouth. If a seizure lasts more than 5 minutes, seek emergency medical help.
How Can You Support Someone With Epilepsy?
Support can take many forms: understanding the condition, being aware of seizure first aid, promoting a positive environment, and encouraging adherence to treatment plans. Respect and empathy are key to supporting someone with epilepsy.
Conclusion
In summary, gaining a comprehensive understanding of epilepsy symptoms and causes is paramount for those affected by this neurological condition and their loved ones. Recognizing the signs of epilepsy—such as seizures, temporary confusion, a staring spell, or involuntary movements—can lead to timely and effective management of the disorder. Additionally, understanding the potential causes, which range from genetic influence to traumatic brain injuries or infectious diseases, empowers individuals to seek the most appropriate care.
We cannot overemphasize the importance of consulting with healthcare professionals if you or someone you know is experiencing symptoms of epilepsy. While the information provided here serves as a foundational overview, each individual’s condition is unique. Professional medical advice is crucial for accurate diagnosis, personalized treatment plans, and managing epilepsy effectively.
In navigating the complexities of epilepsy, remember that you are not alone. With the support of medical professionals and a thorough understanding of the condition, managing epilepsy becomes a more attainable goal. Seek out professional guidance, stay informed, and take proactive steps towards health and well-being.
References
For those interested in delving deeper into the subject of epilepsy symptoms, a wealth of information can be found through reputable sources. Below, we provide carefully selected references to ensure you have access to reliable and comprehensive insights:
- Centers for Disease Control and Prevention (CDC): The CDC’s epilepsy section provides scientifically backed information on the symptoms, causes, and management of epilepsy. A great resource for those seeking knowledge supported by public health research. Explore more at CDC – Epilepsy.
- World Health Organization (WHO): The WHO offers global insights into epilepsy, emphasizing its impact on different populations and strategies for treatment and care worldwide. Their content is invaluable for understanding epilepsy within a global context. Further information can be found at World Health Organization – Epilepsy.
- Mayo Clinic: Renowned for its patient care and research, the Mayo Clinic provides an exhaustive look at epilepsy symptoms, causes, diagnosis, and treatments. Their articles are written by medical professionals and are a trustworthy source for medical advice. Learn more at Mayo Clinic – Epilepsy.
- National Institute of Neurological Disorders and Stroke (NINDS): NINDS offers detailed, research-based information on neurological disorders, including epilepsy. Their resources are geared towards both patients and healthcare professionals, providing a deep dive into the science of epilepsy. Visit NINDS – Epilepsy Information Page for more details.
These resources are instrumental in broadening your understanding of epilepsy symptoms and related information. Whether you’re a patient, caregiver, or simply looking to inform yourself, these links offer a pathway to reputable and authoritative content.