Coronavirus disease 2019 Symptoms: In the wake of the global health crisis, understanding the nuances of Coronavirus Disease 2019 (COVID-19) has become paramount for individuals and communities worldwide.
This comprehensive guide aims to elucidate the symptoms and causes of COVID-19, offering vital information that can aid in the early detection and prevention of this pervasive illness.
Understanding COVID-19: The Global Impact of the Pandemic
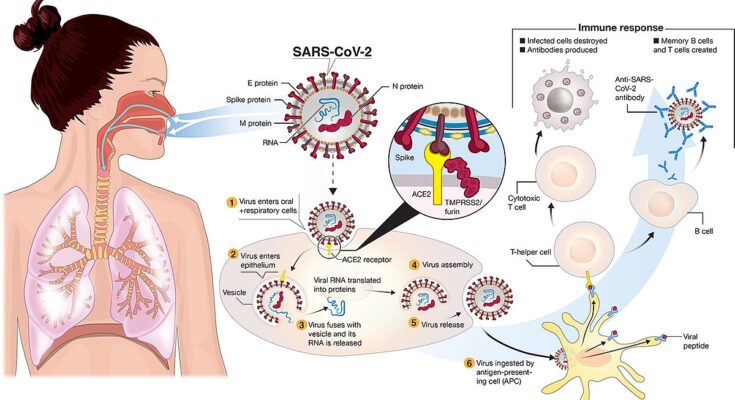
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, emerged as a global health crisis of unprecedented scale, affecting millions worldwide. This section aims to shed light on the nature of COVID-19, its transmission, and the far-reaching consequences it has had on societies across the globe.
What is COVID-19?
COVID-19, or Coronavirus Disease 2019, is an infectious disease that first came to international attention in December 2019 following an outbreak in Wuhan, China. It is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a virus that belongs to the coronavirus family, known for containing strains that can cause respiratory tract infections in humans ranging from the common cold to more severe diseases.
Transmission and Symptoms
The virus primarily spreads between people during close contact, often via small droplets produced by coughing, sneezing, or talking. It can also spread by touching surfaces contaminated with the virus and then touching the face. Symptoms vary widely, from mild or asymptomatic cases to severe illness and death, particularly in older adults and those with underlying health conditions. Common symptoms include fever, cough, and difficulty breathing.
Global Impact
The global impact of the COVID-19 pandemic has been profound, affecting almost every aspect of daily life. Here are some key areas affected:
- Health Systems: Healthcare systems around the world were overwhelmed, with hospitals at capacity and medical supplies in short supply. The pandemic underscored the need for robust healthcare infrastructure and the importance of timely, coordinated responses to public health crises.
- Economy: The economic fallout from the pandemic has been staggering, with businesses closing, unemployment rates soaring, and economies entering recessions. Governments worldwide have implemented unprecedented fiscal measures to mitigate the economic impact, highlighting the interconnectedness of global economies.
- Society and Education: Social distancing measures and lockdowns have transformed how societies function, with impacts on mental health, education, and social cohesion. The move to remote learning exposed inequalities in access to technology and educational resources, affecting students’ learning experiences across the globe.
- Vaccination and Response: The development of COVID-19 vaccines in record time has been a testament to scientific innovation. Vaccination campaigns have varied in effectiveness across countries, influenced by vaccine availability, public trust, and global cooperation.
The pandemic has highlighted the importance of global cooperation, resilient healthcare systems, and the need for equitable access to healthcare resources and vaccines. As the world continues to navigate the pandemic, lessons learned will be invaluable for addressing future global health emergencies.
COVID-19 Symptoms: A Comprehensive Guide
Recognizing the symptoms of COVID-19 is crucial for early detection and prevention of its spread. This comprehensive guide outlines the range of symptoms associated with COVID-19, from the most common to the less frequent, and the severe signs that require immediate medical attention.
Common Symptoms of COVID-19
The most frequently observed symptoms of COVID-19 include:
- Fever: A high body temperature is often one of the first signs of infection.
- Cough: This can be a dry cough that persists over time.
- Fatigue: Many patients report feeling unusually tired or weak.
These symptoms can appear 2-14 days after exposure to the virus, emphasizing the importance of monitoring your health closely if you believe you have been in contact with an infected individual.
Less Common Symptoms
A wider array of symptoms has been reported, albeit less frequently. These include:
- Aches and Pains: Unexplained muscle soreness or joint pain.
- Sore Throat: Many people report a sore or scratchy throat.
- Diarrhea: Some individuals experience gastrointestinal issues.
- Conjunctivitis: Also known as pink eye, characterized by red, irritated eyes.
- Headache: Persistent headaches without a clear cause.
- Loss of Taste or Smell: Many report a sudden inability to taste or smell.
- Skin Rash or Discoloration: Rashes on the skin or a noticeable change in the color of fingers or toes.
Serious Symptoms Warranting Immediate Medical Attention
COVID-19 can also lead to more severe symptoms, particularly in older adults and those with underlying health conditions. These serious symptoms include:
- Difficulty Breathing or Shortness of Breath: This can feel like you can’t get enough air into your lungs.
- Chest Pain or Pressure: A persistent pain or pressure in the chest.
- Loss of Speech or Movement: Sudden inability to speak or move parts of the body.
If you or someone you know experiences these symptoms, seek medical attention immediately.
Asymptomatic Cases: The Silent Spreaders
Significantly, not everyone with COVID-19 shows symptoms. Asymptomatic individuals carry the virus but do not exhibit any of the symptoms listed above. This makes it difficult to identify and contain the spread of the virus, highlighting the importance of wearing masks, practicing social distancing, and following public health guidelines even if you feel healthy.
By recognizing the signs early and taking appropriate actions, we can protect ourselves and others around us. Stay informed, stay safe, and always consult health professionals if you suspect you have been exposed to the virus.
Causes and Transmission of COVID-19
Understanding the causes and transmission mechanisms of COVID-19 is crucial in controlling its spread and protecting communities. COVID-19, caused by the SARS-CoV-2 virus, primarily spreads through person-to-person contact, highlighting the importance of adhering to public health guidelines.
How COVID-19 Spreads
- Person-to-Person Transmission: The most common way the virus spreads is through close contact with someone infected. When an infected person coughs, sneezes, or talks, respiratory droplets containing the virus can reach the mouths or noses of people nearby, potentially entering their lungs.
- Droplets: Large respiratory droplets can land on surfaces or objects. Although not the primary mode of transmission, individuals can get infected by touching these surfaces and then touching their face, particularly the mouth, nose, or eyes.
- Contaminated Surfaces: Surfaces touched by an infected person can harbor the virus for hours to days, depending on the material. Regular cleaning and disinfecting of high-touch surfaces reduce the risk of infection.
Role of Asymptomatic and Pre-Symptomatic Transmission
Asymptomatic (showing no symptoms) and pre-symptomatic (before symptoms appear) transmissions play a significant role in the spread of COVID-19. Individuals without symptoms can unknowingly transmit the virus to others, making it challenging to control the spread. This underscores the importance of wearing masks, social distancing, and practicing good hygiene, even if one feels healthy.
High-Risk Environments and Activities
Certain environments and activities increase the risk of spreading the virus:
- Crowded Places: Enclosed spaces with poor ventilation and crowded settings significantly increase the risk of transmission.
- Close-Contact Settings: Activities that require close physical contact or involve sharing air with many people, such as singing or exercising in gyms, can facilitate the spread.
- High-Touch Environments: Areas where people interact with shared surfaces frequently, like public transportation, shopping centers, and schools, pose a higher risk.
Adhering to guidelines from health authorities, such as wearing masks, maintaining social distance, and getting vaccinated, can significantly reduce the risk of infection and help control the pandemic’s impact on society.
Risk Factors for COVID-19 Severity
Understanding the risk factors associated with severe outcomes from COVID-19 is crucial for everyone, from individuals to healthcare providers. Two primary factors have been identified that significantly influence the severity of COVID-19: age and the presence of pre-existing medical conditions. In this section, we delve into how these factors affect COVID-19 outcomes and why it’s essential to be aware of them.
Age and Its Impact on COVID-19 Severity
Age is a significant determinant of COVID-19 severity. Data and studies from around the globe have consistently shown that older adults are at a higher risk of experiencing severe symptoms, complications, and mortality rates from COVID-19 compared to younger individuals. The immune system’s strength tends to weaken with age, making it harder for the body to fight off infections, including SARS-CoV-2, the virus responsible for COVID-19. Additionally, older adults are more likely to have other health conditions that can exacerbate the effects of COVID-19, further increasing their risk of serious outcomes.
Pre-existing Medical Conditions That Increase COVID-19 Risk
Individuals with certain pre-existing medical conditions are at an elevated risk of severe illness from COVID-19. These conditions can compromise the body’s ability to combat the virus, leading to more significant complications. The main health issues that increase COVID-19 risk include:
- Heart Disease: Patients with heart conditions may experience more severe complications from COVID-19 due to the added strain on the heart.
- Diabetes: Both type 1 and type 2 diabetes can impair the immune system’s effectiveness, making it harder for the body to fight off the virus. Poorly controlled blood sugar levels may also exacerbate the severity of COVID-19.
- Chronic Respiratory Disease: Individuals with pre-existing respiratory conditions, such as chronic obstructive pulmonary disease (COPD), asthma, or pulmonary fibrosis, are at a higher risk of severe respiratory complications from COVID-19.
It’s essential for individuals with these conditions, and those caring for them, to be particularly vigilant in taking precautions against COVID-19. Preventative measures such as vaccination, wearing masks in crowded or indoor settings, and practicing good hygiene can significantly reduce the risk of severe illness.
Age and pre-existing medical conditions are critical risk factors for COVID-19 severity. Understanding these risks can help individuals and healthcare providers take appropriate precautions to protect those most vulnerable to severe outcomes from the virus. By staying informed and adhering to recommended health guidelines, we can collectively work towards minimizing the impact of COVID-19 on our communities.
Complications and Long-term Effects of COVID-19
The journey through COVID-19 doesn’t end with recovery for everyone. For some, the aftermath of the infection brings about a series of complications and long-term effects that can impact health and quality of life. This section delves into the potential complications such as pneumonia and organ failure, and discusses the phenomenon known as Long COVID or post-COVID conditions, shedding light on their implications and the need for ongoing research and support.
Pneumonia and Organ Failure
COVID-19 primarily attacks the respiratory system, but its effects can extend beyond the lungs, leading to severe and sometimes life-threatening complications. Pneumonia, a significant lung infection that fills the lungs with fluid, is a common complication in moderate to severe cases of COVID-19. This condition can severely impair the ability to breathe and, in dire cases, necessitate medical interventions such as oxygen therapy or mechanical ventilation.
Moreover, COVID-19 can precipitate acute organ failure, including the kidneys, heart, and liver. The virus can induce an overwhelming inflammatory response in the body, known as a cytokine storm, which can damage organ tissue and lead to multi-organ failure. This complication is particularly concerning as it significantly increases the mortality risk and requires intensive care to manage.
Long COVID or Post-COVID Conditions
Long COVID, also known as post-COVID-19 syndrome or post-acute sequelae of SARS-CoV-2 infection (PASC), refers to a range of symptoms that continue for weeks or months after the acute phase of the infection has resolved. This condition can affect anyone who has had COVID-19, regardless of the severity of their initial infection.
Symptoms of Long COVID are diverse and can include fatigue, shortness of breath, cognitive impairments (often referred to as “brain fog”), joint pain, chest pain, and more. These symptoms can fluctuate or relapse over time, leading to significant challenges in daily life and, for some, prolonged disability.
The exact cause of Long COVID is still under investigation, but it is believed to result from the immune system’s response to the virus, direct damage caused by the virus, and the psychological impact of infection. Ongoing research aims to understand the mechanisms behind Long COVID, identify risk factors, and develop effective treatments.
The potential complications and long-term effects of COVID-19 underscore the importance of prevention measures, timely treatment for those infected, and support for those experiencing lingering symptoms. As we continue to navigate the pandemic, acknowledging and addressing these challenges is crucial for the health and well-being of individuals and communities worldwide.
Understanding the broad spectrum of COVID-19’s impact is essential for healthcare providers, researchers, and policymakers as they work to mitigate the effects of the pandemic and support those affected by its long-term consequences.
Prevention Strategies for COVID-19
By understanding and implementing a range of protective measures, individuals can significantly reduce their risk of infection. This article outlines the most effective prevention strategies, including hygiene measures, social distancing, and vaccination, to guide you in safeguarding yourself and your community.
Hygiene Measures
Good hygiene practices are the cornerstone of preventing the spread of COVID-19. These include:
- Handwashing: Regularly washing your hands with soap and water for at least 20 seconds is crucial. This simple yet effective practice helps to kill viruses that may be on your hands.
- Sanitizing: In situations where soap and water are not readily available, use an alcohol-based hand sanitizer. Sanitizers with at least 60% alcohol content are recommended to effectively kill viruses.
- Mask-Wearing: Wearing masks in public places, especially where social distancing is difficult, helps reduce the spread of the virus. Masks act as a barrier to prevent virus-laden droplets from infecting others or landing on surfaces.
Social Distancing and Avoiding Crowded Places
Maintaining a safe distance from others is essential to prevent the spread of COVID-19. Social distancing measures include:
- Keeping Distance: Stay at least 6 feet (about 2 arm’s length) away from other people who are not from your household, in both indoor and outdoor spaces.
- Avoiding Crowded Places: Limit your exposure by avoiding places where maintaining a safe distance from others is difficult. This includes crowded public places, large gatherings, and any event that draws a crowd.
Vaccination: Current Status and Effectiveness
Vaccination against COVID-19 has proven to be a game-changer in the fight against the pandemic. Here’s what you need to know:
- Current Status: As of the latest updates, several COVID-19 vaccines have received authorization from health authorities worldwide. These vaccines have undergone rigorous testing to ensure their safety and effectiveness.
- Effectiveness: Vaccines work by training the immune system to recognize and fight the virus. They significantly reduce the risk of developing severe illness, hospitalization, and death due to the virus. It’s important to stay informed about the latest vaccine recommendations, including booster shots, to maintain high levels of immunity.
Implementing these prevention strategies can greatly reduce your risk of contracting and spreading COVID-19. By practicing good hygiene, maintaining social distance, avoiding crowded places, and getting vaccinated, you play a crucial role in the global effort to control the pandemic. Stay informed, stay safe, and together, we can overcome COVID-19.
Diagnosis and Testing for COVID-19
Diagnosing and testing for COVID-19 are crucial steps in managing and controlling the spread of the virus. Understanding the methods of diagnosis and the types of tests available is essential for individuals suspecting an infection and for healthcare providers. This guide outlines the various diagnostic methods for COVID-19, the types of tests available, and advice on when and how to get tested.
Methods of Diagnosis for COVID-19
The diagnosis of COVID-19 primarily involves identifying the presence of the SARS-CoV-2 virus, which causes the disease. Healthcare professionals use a combination of medical history, symptom assessment, and laboratory tests to diagnose COVID-19. The diagnostic process may include:
- Clinical Evaluation: Assessment of symptoms such as fever, cough, shortness of breath, and recent exposure to COVID-19.
- Epidemiological Information: Considering factors like recent travel history to affected areas or contact with confirmed COVID-19 cases.
- Laboratory Testing: The most definitive method for diagnosing COVID-19, involving various types of tests to detect the virus.
Types of Tests for COVID-19
Several types of tests are available for COVID-19, each serving different purposes:
- PCR Tests: Polymerase Chain Reaction (PCR) tests are considered the gold standard for detecting the presence of the virus’s genetic material in a sample. They are highly accurate and are used for confirming active infections.
- Antigen Tests: These tests detect specific proteins from the virus. Antigen tests are faster and less expensive than PCR tests but may not be as accurate. They are useful for rapid screening in high-volume settings.
- Antibody Tests: Also known as serology tests, antibody tests identify antibodies produced by the immune system in response to COVID-19. These tests help determine if an individual had a past infection but are not effective for diagnosing active infections.
When and How to Get Tested
- When to Get Tested: Testing is recommended if you have symptoms of COVID-19, have been in close contact with a confirmed case, or have been advised by a healthcare professional. In areas with high transmission rates, regular testing might be recommended for people with frequent public exposure.
- How to Get Tested: If you need a COVID-19 test, contact your healthcare provider or local health department to find out where and how to get tested. Testing protocols may vary by location, but generally, you will need to provide a sample through a nasal or throat swab for PCR and antigen tests, or a blood sample for antibody tests.
- Follow-Up After Testing: Follow the advice of healthcare professionals regarding isolation and treatment while waiting for test results. If you test positive for COVID-19, follow public health guidelines for isolation and notify close contacts about their potential exposure.
Always consult healthcare professionals for guidance on testing and follow public health recommendations to protect yourself and others.
Treatment and Management of COVID-19
As the world continues to navigate the challenges posed by COVID-19, understanding the most effective ways to treat and manage the virus is crucial. Whether you’re dealing with mild symptoms at home or facing more severe cases that require medical intervention, there are strategies and treatments available to support recovery and manage symptoms.
Home Care for Mild Symptoms
For many individuals, COVID-19 presents with mild symptoms that can be effectively managed at home. The key is to focus on relief from symptoms while your body fights off the virus. Here’s how you can take care of yourself or a loved one:
- Stay Hydrated: Drink plenty of fluids like water, herbal teas, or broth to stay hydrated. Avoid caffeine and alcohol as they can lead to dehydration.
- Rest: Ensure you get plenty of sleep and rest to help your body’s immune system fight off the virus.
- Isolate: To prevent the spread of the virus to family members or housemates, isolate yourself in a separate room and use a separate bathroom if possible.
- Monitor Symptoms: Keep a close eye on your symptoms. If they worsen or if you experience difficulty breathing, persistent pain or pressure in your chest, new confusion, inability to wake or stay awake, or bluish lips or face, seek medical attention immediately.
- Over-the-counter Medications: Use over-the-counter medications to help relieve fever, headaches, and body aches. Follow the instructions on the label and consult your healthcare provider for advice tailored to your specific health condition.
Medical Treatments for Severe Cases
Severe cases of COVID-19 often require medical intervention and hospitalization. These cases may present with severe respiratory symptoms, high fever, significant fatigue, and other complications that necessitate more advanced care. Here are the primary treatments currently being used for severe COVID-19 cases:
- Antiviral Medications: These are prescription drugs that fight against the coronavirus in your body. They are typically administered in a hospital setting.
- Steroids: To reduce inflammation in the lungs caused by the virus, doctors may prescribe steroids.
- Oxygen Therapy: Patients experiencing difficulty breathing may require supplemental oxygen or mechanical ventilation in more severe cases.
- Antibody Treatments: For certain high-risk patients, monoclonal antibodies that target the coronavirus can be used early in the infection to help reduce the severity of the disease.
- Supportive Care: This includes treatments to support vital organ functions, such as mechanical ventilation for critically ill patients, as well as fluids and medication to support blood pressure.
It’s important to note that treatment strategies for COVID-19 continue to evolve as more research is conducted and new therapies are developed. Always consult healthcare professionals for the most current advice and personalized treatment options.
By understanding the appropriate steps to take for both mild and severe cases of COVID-19, individuals can better prepare to manage the virus’s impact. Remember, prevention through vaccination, wearing masks, and practicing social distancing remains key in controlling the spread of COVID-19.
FAQs: Understanding COVID-19 Symptoms and Causes
What are the common symptoms of COVID-19?
COVID-19 symptoms can range from mild to severe and may appear 2-14 days after exposure to the virus. The most common symptoms include fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea. It’s important to note that this list does not include all possible symptoms, and individuals may experience symptoms differently.
How does COVID-19 spread?
COVID-19 is primarily spread from person to person, mainly through respiratory droplets produced when an infected person coughs, sneezes, talks, or breathes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. Spread is more likely when people are in close contact with one another (within about 6 feet). COVID-19 may also spread by touching surfaces or objects that have the virus on them and then touching one’s mouth, nose, or possibly eyes, although this is not thought to be the main way the virus spreads.
Can asymptomatic individuals transmit COVID-19?
Yes, individuals infected with COVID-19 can transmit the virus to others even if they do not show symptoms (asymptomatic) or before they start showing symptoms (pre-symptomatic). This is why wearing masks, practicing social distancing, and frequent handwashing are recommended as preventive measures.
What causes COVID-19?
COVID-19 is caused by the coronavirus known as SARS-CoV-2. Coronaviruses are a large family of viruses that are common in people and many different species of animals. SARS-CoV-2 is a novel coronavirus that was first identified in an outbreak in Wuhan, China, in December 2019. It is related to other coronaviruses like MERS-CoV and SARS-CoV, but it is a distinct virus with its own characteristics.
Is there a cure for COVID-19?
As of my last update, there is no specific cure for COVID-19. Treatment focuses on relieving symptoms and may include rest, fluid intake, and pain relievers. For severe cases, hospitalization may be required, and treatment might involve respiratory support such as mechanical ventilation. Vaccines are available and are the most effective way to prevent the disease and reduce the severity of symptoms if infected.
How can I protect myself from COVID-19?
The best way to prevent illness is to avoid being exposed to the virus. Measures to protect yourself and others include getting vaccinated, wearing masks in public settings, practicing social distancing, washing your hands frequently with soap and water for at least 20 seconds, avoiding touching your face, covering coughs and sneezes, cleaning and disinfecting frequently touched surfaces daily, and staying home if you are sick.
Conclusion
Vaccination emerges as a beacon of hope in curbing the pandemic. Getting vaccinated is a critical step toward achieving herd immunity, significantly reducing the virus’s spread, and paving the way for a return to normalcy. Vaccines have undergone rigorous testing and have proven to be safe and effective in preventing COVID-19, including its severe forms and complications. By choosing to get vaccinated, you contribute to a global effort to end the pandemic, demonstrating solidarity and concern for your community’s well-being.
In conclusion, the fight against COVID-19 is far from over, but with the right knowledge and actions, we can make a difference. Recognizing symptoms, understanding the virus’s causes, following public health guidelines, and getting vaccinated are key strategies in this ongoing battle. Let’s continue to support each other, stay informed, and take proactive steps to protect our health and the health of those around us. Together, we can overcome this challenge and emerge stronger on the other side.