Choroid Plexus Carcinoma Symptoms: Choroid Plexus Carcinoma (CPC) represents a rare, aggressive type of brain cancer that originates in the choroid plexus, the area of the brain responsible for producing cerebrospinal fluid (CSF).
This fluid is crucial for protecting and nourishing the brain and spinal cord. Although CPC is most commonly diagnosed in young children, it can affect individuals at any age, presenting a unique set of challenges for diagnosis and treatment.
What is Choroid Plexus Carcinoma?
Choroid Plexus Carcinoma (CPC) is a rare, aggressive type of cancer that arises in the choroid plexus of the brain. The choroid plexus is a vital tissue within the brain’s ventricular system responsible for producing cerebrospinal fluid (CSF), which cushions the brain and spinal cord, provides nutrients, and removes waste. CPC is characterized by the rapid growth of malignant cells in the choroid plexus, leading to an overproduction of CSF and potential blockage of fluid pathways, resulting in increased intracranial pressure and associated symptoms.
The Role of the Choroid Plexus in the Brain
The choroid plexus plays a crucial role in maintaining the brain’s environment. It produces the cerebrospinal fluid that bathes the brain and spinal cord, offering protection, nutrient delivery, and waste removal. The CSF also maintains intracranial pressure, providing a cushioning effect that protects the brain against injury. Additionally, the choroid plexus acts as a selective barrier, regulating the exchange of substances between the blood and the CSF, thus playing a significant role in the brain’s immune defense.
Statistics on Prevalence and Demographics Affected
Choroid Plexus Carcinoma is an exceedingly rare condition, accounting for less than 1% of all brain tumors. It predominantly affects children under the age of 5, with a higher incidence in infants and toddlers. Although it can occur in adults, such cases are extremely rare. The incidence rate does not show a significant preference for any gender or race, indicating that CPC can affect individuals across various demographics. Due to its rarity, comprehensive statistics on prevalence are limited; however, the available data underscores the importance of awareness and research to improve diagnosis, treatment, and outcomes for those affected by this aggressive cancer.
Symptoms of Choroid Plexus Carcinoma
Understanding these symptoms is vital for early diagnosis and effective treatment. Below, we delve into the common symptoms associated with CPC, explore the reasons behind these symptoms, and highlight how they can differ between children and adults.
Common Symptoms of Choroid Plexus Carcinoma
Patients with CPC may experience a variety of symptoms, which often relate to increased intracranial pressure caused by the tumor. These symptoms include:
- Headaches: Often severe and more intense in the morning.
- Nausea and Vomiting: Especially prominent in the morning or worsening with movement.
- Problems with Balance and Coordination: Difficulty walking or performing tasks that require fine motor skills.
- Vision Problems: Blurred vision, double vision, or loss of peripheral vision.
- Seizures: Can vary in severity and frequency.
- Changes in Personality or Behavior: Especially noted in adults, these can include irritability, confusion, or lethargy.
- Cognitive Decline: Difficulty with memory, concentration, or executive functions.
Why These Symptoms Occur
The symptoms of CPC primarily arise due to the tumor’s location and its impact on the normal flow and absorption of CSF, leading to increased pressure within the skull. This pressure can directly affect brain function, leading to the symptoms described above. Tumors can also invade surrounding brain tissues, further exacerbating symptoms through direct damage or disruption of normal brain activities.
Differences Between Children and Adults
The manifestation of CPC symptoms can vary significantly between children and adults, primarily due to the differences in brain development and the capacity of the skull:
- Children: In infants and young children, the most noticeable symptoms may include an unusually rapid increase in head size (due to the flexibility of the skull sutures), bulging at the soft spots (fontanelles), and irritability. Given their limited ability to communicate, symptoms in children may be more difficult to initially recognize.
- Adults: Adults are more likely to present with more defined neurological symptoms such as cognitive changes, headaches, and vision problems. Since an adult’s skull is fully fused, any increase in intracranial pressure is less likely to affect head size but more likely to result in pronounced neurological and cognitive symptoms.
Recognizing the symptoms of Choroid Plexus Carcinoma is crucial for timely diagnosis and treatment. While there is an overlap in the symptoms experienced by children and adults, the presentation can vary significantly due to physiological differences. If you or someone you know is exhibiting symptoms consistent with CPC, seeking medical attention is imperative for a thorough evaluation and appropriate management. Early intervention can significantly improve outcomes, highlighting the importance of awareness and prompt action.
Causes and Risk Factors of Choroid Plexus Carcinoma
Understanding the causes and risk factors of CPC is crucial for early diagnosis and effective treatment. This article provides an overview of current knowledge regarding the causes of CPC, the role of genetic mutations, potential environmental risk factors, and insights from recent research and studies.
Genetic Mutations and Their Role
Genetic mutations play a significant role in the development of CPC. Studies have identified several genetic alterations associated with CPC, including mutations in the TP53 gene, which is known to be a crucial tumor suppressor gene in many types of cancer. Additionally, alterations in the genes responsible for cell growth and division may lead to the uncontrolled proliferation of cells, resulting in cancer. In some cases, CPC has been linked to genetic syndromes, such as Li-Fraumeni syndrome, suggesting a hereditary component to the risk of developing this cancer.
Environmental Risk Factors
While much of the focus has been on genetic factors, researchers are also investigating potential environmental risk factors that could contribute to CPC. However, to date, no specific environmental factors have been conclusively linked to the development of CPC. This area of research remains speculative, and more studies are needed to understand any potential environmental influences.
Research and Studies on Causes
Research into the causes of CPC is ongoing, with scientists conducting genetic studies and exploring potential environmental influences. Advances in genomic sequencing technology have allowed researchers to identify specific genetic mutations associated with CPC, providing insights into the molecular mechanisms that drive the development of this cancer. Clinical studies focusing on patients with CPC and related conditions are crucial for uncovering new information about risk factors and causes.
However, while the exact causes of CPC are not fully understood, current evidence points to a combination of genetic mutations and possibly environmental factors. Ongoing research and technological advances in genomics are expected to shed further light on the causes of CPC, potentially leading to better prevention strategies and treatment options. Understanding the risk factors and causes of CPC is essential for early diagnosis, effective treatment, and improving patient outcomes.
Diagnosing Choroid Plexus Carcinoma
Diagnosing Choroid Plexus Carcinoma (CPC) is a critical step in managing and treating this rare type of brain tumor. Early detection and accurate diagnosis are essential for determining the most effective treatment plan. This guide provides an overview of the diagnostic process for CPC, including the types of medical tests and imaging techniques commonly used and the importance of early detection.
The Process of Diagnosing CPC
The journey to diagnosing Choroid Plexus Carcinoma typically begins with a careful assessment of symptoms and a thorough medical history review. Since CPC symptoms can vary and often mimic other conditions, healthcare providers employ a range of diagnostic tests to confirm the presence of a tumor and to determine its type.
Types of Medical Tests and Imaging Used
- Magnetic Resonance Imaging (MRI): MRI scans are pivotal in diagnosing CPC because they can produce detailed images of the brain, highlighting the presence of tumors. MRI helps in determining the size, location, and potential spread of the tumor within the brain or spinal cord.
- Computed Tomography (CT) Scan: Though MRI is preferred, CT scans can also be used, especially if MRI is not available. CT scans can provide valuable information about the tumor’s shape, size, and effect on surrounding structures.
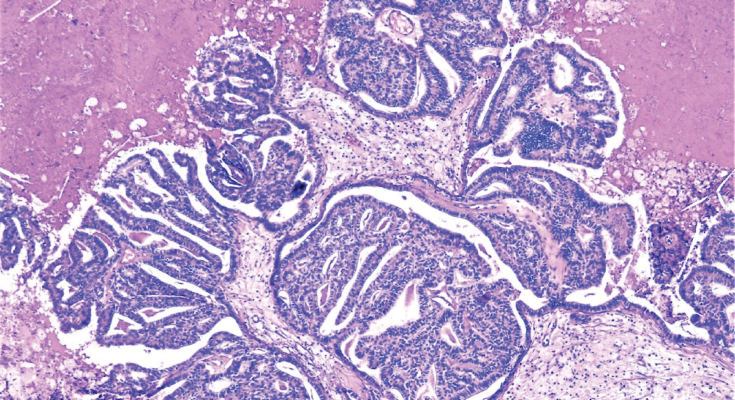
- Biopsy: A biopsy is a definitive test for diagnosing CPC. This procedure involves removing a small tissue sample from the tumor for microscopic examination. A biopsy can confirm whether the tumor is benign (choroid plexus papilloma) or malignant (choroid plexus carcinoma) and helps in planning the treatment.
Importance of Early Detection
Early detection of CPC is crucial. It can significantly influence the treatment outcome and improve the prognosis. When detected early, treatment options like surgery, radiation therapy, and chemotherapy can be more effective, potentially leading to a better quality of life and longer survival rates. Early diagnosis also allows for timely intervention before the tumor can grow larger or spread, reducing the risk of complications and improving the chances of successful treatment.
However, diagnosing Choroid Plexus Carcinoma involves a comprehensive evaluation using advanced imaging techniques and biopsy procedures. Understanding the importance of early detection and the role of various diagnostic tools can empower patients and caregivers to seek prompt medical attention, leading to timely and effective treatment. If you or someone you know is experiencing symptoms suggestive of a brain tumor, consult a healthcare professional immediately for an accurate diagnosis and appropriate treatment plan.
Treatment Options for Choroid Plexus Carcinoma
Understanding the nuances of each treatment method, alongside the latest advances in medical science, is crucial for optimizing patient outcomes. This guide delves into the conventional treatment options for CPC, highlights recent advancements, and underscores the significance of personalized treatment plans.
Conventional Treatment Methods
Surgery is often the first line of defense against CPC. The primary goal is to remove as much of the tumor as possible without compromising vital brain functions. Complete resection can significantly improve prognosis, but the tumor’s location and the potential for neurological damage make this challenging.
Chemotherapy plays a pivotal role, especially when surgical resection is incomplete or infeasible. Chemotherapy can reduce tumor size, manage symptoms, and, in some cases, serve as a neoadjuvant (pre-surgery) treatment to shrink the tumor, making surgical removal easier and safer.
Radiation Therapy is considered for older children and adults, particularly in cases where the tumor is inoperable or only partially resected. Radiation can target tumor cells while sparing surrounding healthy tissue, though its use in very young children is limited due to the risk of long-term cognitive and developmental side effects.
Advances in Treatment Options
The medical community’s understanding of CPC has grown, leading to significant advancements in treatment. Innovations such as targeted therapy and immunotherapy have opened new avenues for managing CPC. Targeted therapies aim to attack specific genetic mutations within the tumor, minimizing damage to healthy cells, while immunotherapy helps the body’s immune system recognize and destroy cancer cells. These advances not only promise improved survival rates but also aim to reduce the long-term side effects associated with traditional treatments.
Another exciting development is the use of precision medicine, which involves tailoring treatment plans based on the genetic makeup of the patient’s tumor. This approach has the potential to increase treatment efficacy and minimize adverse effects by focusing on the individual characteristics of the tumor.
The Importance of Personalized Treatment Plans
Given the complexity of CPC and the variability in how it affects individuals, personalized treatment plans are paramount. A multidisciplinary team of specialists, including neurosurgeons, oncologists, radiologists, and pediatricians, should collaborate to tailor treatment strategies that meet the specific needs of each patient. Factors such as the tumor’s size, location, genetic mutations, and the patient’s overall health and age play a critical role in shaping these plans.
Personalized treatment plans not only aim to improve survival rates but also focus on the quality of life, seeking to minimize the cognitive and physical side effects that can result from treatment. Regular follow-ups and adjustments to the treatment plan are essential to manage the disease effectively and address any complications that may arise.
Living with Choroid Plexus Carcinoma
Managing symptoms, coping with treatment side effects, and maintaining quality of life require a comprehensive approach. Here, we delve into strategies to manage the physical and emotional impact of CPC, and the support systems available to assist patients and their loved ones through this journey.
Managing Symptoms and Side Effects of Treatment
CPC and its treatments can lead to a range of symptoms and side effects, varying from mild to severe. Common symptoms include headaches, nausea, and changes in mood or behavior, stemming from the tumor’s pressure on the brain. Treatments like surgery, chemotherapy, and radiation, while pivotal in managing the disease, can also contribute to side effects such as fatigue, cognitive changes, and emotional distress.
Strategies for Symptom Management:
- Medication: Regular consultations with your healthcare team can help adjust medications to manage pain, nausea, and other symptoms effectively.
- Rehabilitation Therapies: Physical, occupational, and speech therapy can assist in regaining lost functions and improving quality of life.
- Lifestyle Adjustments: Simple changes, such as maintaining a healthy diet, engaging in gentle exercise, and ensuring adequate rest, can significantly impact symptom management.
Support for Patients and Families
The diagnosis of CPC can be overwhelming for both patients and their families. Emotional support and practical assistance are critical components of the care plan.
Counseling: Individual or family counseling with a psychologist or psychiatrist can help address the emotional and psychological challenges of living with CPC. It provides a safe space to express feelings, cope with anxiety and depression, and strengthen coping mechanisms.
Support Groups: Connecting with others who are facing similar challenges can provide comfort and practical advice. Support groups, whether in-person or online, offer a platform to share experiences, tips, and encouragement.
Quality of Life Considerations
Maintaining or enhancing quality of life is a central goal in the care of patients with CPC. This involves addressing physical symptoms, emotional well-being, social interactions, and spiritual concerns.
Holistic Care Approaches: Integrative therapies such as meditation, acupuncture, and yoga can complement traditional treatments by reducing stress and improving mental health.
Social and Recreational Activities: Encouraging participation in enjoyable activities can help patients maintain a sense of normalcy and fulfillment.
Advanced Care Planning: Discussing preferences for future care and decision-making can reduce uncertainties and ensure that patient values guide health care decisions.
Living with Choroid Plexus Carcinoma is a challenging journey that requires a multifaceted care approach. Managing symptoms and side effects, accessing emotional support, and focusing on quality of life are essential steps in navigating this path. With the right support and resources, patients and their families can find strength and resilience amidst the challenges, leading to a life filled with hope and dignity.
Conclusion
To those who are navigating through the challenges posed by CPC, know that you are not alone. Seeking medical advice from healthcare professionals who specialize in neuro-oncology can provide you with the tailored care and support you need. Additionally, connecting with support groups and networks can offer comfort and guidance through shared experiences and resources.
As we conclude, let’s also underscore the critical need for further research and heightened awareness about Choroid Plexus Carcinoma. Advances in medical research are essential in developing more effective treatments and understanding the underlying causes of CPC. Raising awareness can lead to increased funding for research and support for affected individuals and their families.
Therefore, we call on researchers, healthcare professionals, patients, and the broader community to join forces in the fight against Choroid Plexus Carcinoma. By contributing to research efforts, sharing information, and supporting those impacted, we can make strides in improving outcomes and ultimately finding a cure. Let’s work together to shine a light on CPC and make a difference in the lives of those touched by this condition.