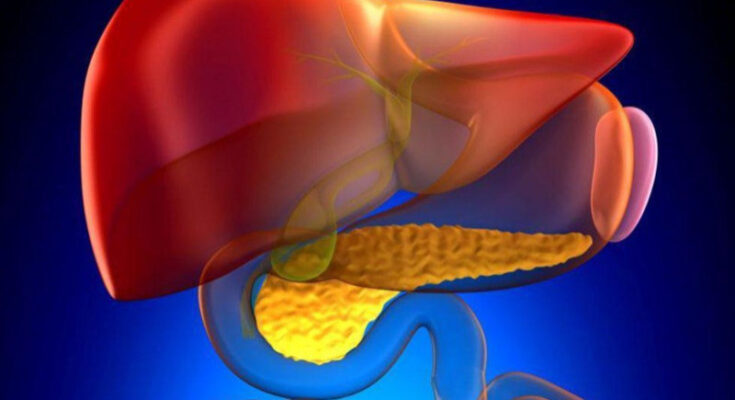
Primary Sclerosing Cholangitis Symptoms: Primary Sclerosing Cholangitis (PSC) is a rare, chronic liver disease that primarily affects the bile ducts both inside and outside the liver.
These ducts become inflamed, leading to scarring and eventual blockage. Over time, this scarring can lead to liver failure.
Understanding the symptoms and causes of PSC is crucial for early diagnosis and management.
Understanding Primary Sclerosing Cholangitis
Primary Sclerosing Cholangitis (PSC) is a chronic liver disease characterized by inflammation and scarring of the bile ducts, which can lead to liver damage and ultimately liver failure. Understanding the demographics and prevalence of this condition is crucial for better awareness and management strategies.
Prevalence of Primary Sclerosing Cholangitis
PSC is considered a rare condition, affecting approximately 6 to 16 individuals per 100,000 in the general population. This disease is more commonly diagnosed in individuals between the ages of 30 and 40, though it can occur at any age.
Demographics Affected by Primary Sclerosing Cholangitis
- Gender Distribution: PSC shows a higher prevalence in males, with about two-thirds of the cases occurring in men compared to one-third in women.
- Geographical Variance: While PSC affects individuals worldwide, there is a higher reported incidence in Western countries, possibly due to better diagnostic facilities and greater awareness of the condition.
- Ethnicity and Genetic Factors: There is a notable variation in the incidence of PSC among different ethnic groups. It is more common in Caucasian populations compared to African or Asian populations. Genetic predispositions, along with environmental factors, are believed to play significant roles in the development of the disease.
However, understanding these statistics and demographics is essential for medical professionals and researchers in tailoring prevention and treatment programs specific to the populations most at risk.
Symptoms of Primary Sclerosing Cholangitis
Understanding the symptoms of PSC is crucial for early detection and management. Below, we explore the early signs, common symptoms, the progression of these symptoms, and provide anecdotal examples for clarity.
Early Signs of Primary Sclerosing Cholangitis
The initial symptoms of PSC might be subtle and easily overlooked. Early signs include:
- Fatigue: A general feeling of tiredness and lack of energy that is not relieved by sleep.
- Itching (Pruritus): Unexplained and persistent itching, typically without a rash.
- Abdominal Discomfort: Mild discomfort or pain in the upper right quadrant of the abdomen.
- Jaundice: Early jaundice is rare but may occur; it manifests as a yellowing of the skin and eyes.
These signs often develop slowly and can be mistaken for symptoms of other less serious conditions.
Common Symptoms Experienced by Patients
As the disease progresses, more evident and severe symptoms begin to appear:
- Cholangitis: Episodes of bacterial cholangitis, which are marked by fever, chills, and upper abdominal pain.
- Liver Enlargement: The liver may become enlarged and palpable.
- Dark Urine: Urine may appear darker than usual, indicating liver dysfunction.
- Pale Stools: Stools may become pale or clay-colored due to lack of bile.
These symptoms reflect more significant bile duct obstruction and liver involvement.
Progression of Symptoms Over Time
Over time, if PSC progresses without intervention, symptoms may worsen, leading to serious liver complications:
- Cirrhosis: Scarring of the liver tissue leading to liver failure.
- Portal Hypertension: Increased blood pressure in the portal veins.
- Varices: Swollen blood vessels, particularly in the esophagus or stomach, which can bleed.
- Ascites: Accumulation of fluid in the abdomen.
- Hepatic Encephalopathy: Impaired brain function due to liver’s inability to remove toxins from the blood.
Each of these conditions is serious and requires medical attention.
Case Studies and Anecdotal Examples
Consider the case of John, a 43-year-old male, who initially experienced mild itching and fatigue that he attributed to his demanding job. Over several months, John’s symptoms expanded to include upper abdominal pain and jaundice. After a blood test showed abnormal liver enzyme levels, further evaluation led to a PSC diagnosis. John’s case illustrates how gradual and deceptive the onset of PSC can be.
In another anecdote, Sarah, a 35-year-old female, noted an abrupt onset of dark urine and persistent itching. Unlike John, Sarah sought immediate medical help, leading to an early diagnosis and management plan for PSC, highlighting the importance of attention to subtle body changes.
Causes and Risk Factors of Primary Sclerosing Cholangitis
Primary Sclerosing Cholangitis (PSC) is a progressive liver disease characterized by inflammation and scarring of the bile ducts. The exact causes of PSC remain unknown, but several factors may increase the risk of developing this condition.
Causes of Primary Sclerosing Cholangitis
Although the precise cause of PSC is not fully understood, it is often considered an autoimmune condition. This means the body’s immune system mistakenly attacks its own bile duct cells, leading to inflammation and fibrosis. Here are some possible triggers:
- Genetic predisposition: Some individuals may have genetic markers that increase their susceptibility to PSC.
- Autoimmune response: PSC may be related to an abnormal immune reaction against the bile duct cells, although the specific antigens or triggers are not yet identified.
- Gut microbiome: Recent studies suggest a potential link between the composition of the gut microbiota and the development of PSC, although this area is still under investigation.
Risk Factors of Primary Sclerosing Cholangitis
Certain risk factors are associated with a higher likelihood of developing PSC:
- Age and gender: PSC is more commonly diagnosed in men than in women and typically affects individuals between the ages of 30 and 60.
- Existing health conditions: Having inflammatory bowel disease, particularly ulcerative colitis, is strongly associated with PSC. Around 75% of PSC patients also suffer from ulcerative colitis.
- Geographic and ethnic factors: The prevalence of PSC varies geographically and is more common in Northern European populations.
Lifestyle or Other Risk Factors
While lifestyle factors are not directly linked to the onset of PSC, certain behaviors may impact the overall health of individuals with the condition or the progression of liver diseases in general:
- Smoking: Tobacco use can exacerbate liver damage and is discouraged in patients with any liver condition.
- Alcohol consumption: Although alcohol is not a direct cause of PSC, avoiding alcohol can help manage liver health and prevent further complications.
- Diet: No specific diet causes or prevents PSC, but a balanced diet supports liver health and overall well-being.
If you or someone you know is at risk or showing symptoms of PSC, consulting with a healthcare professional for early diagnosis and management is crucial.
Diagnosing Primary Sclerosing Cholangitis
Accurate diagnosis is crucial but can be complex due to the disease’s subtle early symptoms. Here, we explore the common diagnostic tests and procedures, how symptoms contribute to diagnosis, and the challenges faced in diagnosing PSC early.
Common Diagnostic Tests and Procedures
- Blood Tests: Initial screening often begins with blood tests that check liver function. Elevated liver enzymes might suggest bile duct obstruction and damage.
- Magnetic Resonance Imaging (MRI): An MRI can produce detailed images of the bile ducts and liver, helping to identify blockages or abnormalities without invasive surgery.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This procedure involves inserting a tube through the mouth, down to the bile ducts, where dye is injected before taking X-rays. ERCP can help visualize blockages and take tissue samples.
- Liver Biopsy: A biopsy involves taking a small sample of liver tissue to examine under a microscope, helping to confirm the diagnosis and assess the extent of liver damage.
- Ultrasound: This non-invasive test uses sound waves to create images of the liver and bile ducts, often used as a preliminary assessment tool.
How Symptoms Contribute to Diagnosis
Symptoms of PSC often include jaundice (yellowing of the skin and eyes), itching, fatigue, and abdominal pain. These symptoms prompt further investigation through the diagnostic tests listed above. However, in early stages, symptoms can be minimal or absent, which makes timely diagnosis challenging. The presence of inflammatory bowel disease, which is commonly associated with PSC, can also guide the diagnostic process.
Challenges in Diagnosing PSC Early
Diagnosing PSC early poses several challenges:
- Non-specific Symptoms: Early symptoms are often vague and can be mistaken for other less severe conditions, delaying specific testing.
- Silent Progression: PSC can progress significantly without any symptoms, often leading to a delay in seeking medical advice until the disease is quite advanced.
- Lack of Specific Biomarkers: There is currently no single test that can definitively diagnose PSC, requiring a combination of imaging and histological data to confirm the disease.
- Overlap with Other Liver Diseases: Symptoms and test results can overlap with other liver and bile duct diseases, complicating the diagnosis.
However, early recognition and monitoring of symptoms, combined with the appropriate use of diagnostic tests, are key to managing this complex condition.
Impact of Primary Sclerosing Cholangitis on Patients
Primary Sclerosing Cholangitis (PSC) is a chronic liver disease that significantly impacts patients’ lives both physically and psychologically. Understanding these effects is crucial for patients, caregivers, and healthcare providers to manage the condition effectively and improve quality of life.
Physical Impacts and Complications
PSC primarily affects the bile ducts, leading to a range of physical complications:
- Cholestasis: This is one of the earliest symptoms of PSC, where bile flow from the liver is progressively impaired, causing jaundice, itching, and fatigue.
- Liver Cirrhosis: Over time, PSC can lead to cirrhosis, where normal liver tissue is replaced by scar tissue. This severe condition results in decreased liver function and can lead to liver failure.
- Increased Risk of Liver Cancer: Patients with PSC have a heightened risk of developing cholangiocarcinoma, a type of cancer that affects the bile ducts.
- Infections: The damage to bile ducts can make patients more susceptible to infections, particularly bacterial cholangitis, which can cause fever, pain, and jaundice.
- Digestive Problems: As bile flow decreases, digestion of fats becomes more difficult, leading to issues such as diarrhea, vitamin deficiencies, and weight loss.
- Portal Hypertension: Advanced PSC can cause increased blood pressure in the portal vein system, leading to complications like varices (enlarged veins) which can bleed severely.
Psychological and Social Effects of Living with PSC
Living with PSC also has profound psychological and social effects:
- Anxiety and Depression: The uncertainty and chronic nature of PSC can lead to significant mental health challenges, including anxiety and depression.
- Social Isolation: Symptoms like fatigue and itching can reduce patients’ ability to participate in social activities, leading to feelings of isolation.
- Impact on Employment: Fluctuating symptoms can affect a patient’s ability to maintain regular employment, which may lead to financial stress and affect their professional identity and self-esteem.
- Emotional Strain: Constant health concerns and frequent medical appointments can cause considerable emotional distress and strain on personal relationships.
- Coping with Uncertainty: The variable progression of PSC means that patients must cope with a lot of uncertainty regarding their health and future.
However, understanding these impacts can aid in more compassionate care and tailored treatment strategies to help mitigate the burdens of PSC.
Management and Treatment Options for Primary Sclerosing Cholangitis
Managing PSC effectively requires a comprehensive approach tailored to individual patient needs. Here, we explore current treatment options, emerging therapies, and the importance of personalized treatment plans.
Current Treatment Approaches for Managing Symptoms
- Medication to Manage Cholestasis: Medications such as ursodeoxycholic acid (UDCA) are often prescribed to help improve bile flow, which can potentially slow the disease’s progression and alleviate symptoms like itching.
- Endoscopic Procedures: Regular endoscopic retrograde cholangiopancreatography (ERCP) procedures are used to dilate strictures in the bile ducts, helping to relieve blockages and reduce symptoms such as jaundice.
- Antibiotics for Infections: Due to the risk of bile duct infections, antibiotics are frequently used as a preventive measure or to treat ongoing infections.
- Vitamin Supplementation: Patients with PSC often suffer from vitamin deficiencies due to poor absorption. Supplements for vitamins A, D, E, and K are usually recommended to maintain adequate nutrient levels.
- Liver Transplant: For advanced PSC, a liver transplant may be considered. This is generally reserved for cases where other treatments have failed, and significant liver damage has occurred.
Research on New Treatments and Therapies
Emerging research into PSC treatments is focused on both improving existing therapies and discovering new treatment avenues:
- Immunosuppressive Therapies: Clinical trials are exploring the effectiveness of immunosuppressive drugs in reducing inflammation and delaying disease progression.
- Fibrosis Inhibitors: New drugs aimed at preventing or reducing fibrosis (scarring of the liver) are under investigation. These could potentially halt the progression of PSC or even reverse some of its effects.
- Genetic and Molecular Therapies: Researchers are examining the genetic and molecular bases of PSC to develop targeted therapies that could prevent or treat the disease at its root.
- Microbiome Treatments: The role of gut bacteria in PSC is a growing area of interest, with studies looking into how modifying the gut microbiota might influence the course of the disease.
Importance of Personalized Treatment Plans
Personalized treatment plans are vital in managing PSC effectively due to the disease’s variable progression and the differences in symptoms among patients:
- Individual Symptom Management: Because symptoms and disease progression can vary widely, treatments need to be tailored to each patient’s specific needs and symptoms.
- Regular Monitoring and Adjustment: Frequent monitoring through blood tests, imaging, and possibly liver biopsies is crucial. These allow for timely adjustments in treatment strategies based on disease progression and response to therapy.
- Multidisciplinary Approach: Effective management of PSC often requires a team of specialists, including hepatologists, gastroenterologists, radiologists, and transplant surgeons, to address the comprehensive needs of the patient.
- Patient Education and Support: Educating patients about their condition and treatment options is essential for effective disease management. Support groups and counseling can also play a significant role in helping patients cope with the psychological aspects of chronic illness.
However, managing Primary Sclerosing Cholangitis involves a combination of current treatments, ongoing research into new therapies, and a personalized approach to care.
Prevention and Monitoring of Primary Sclerosing Cholangitis
While there is currently no definitive way to prevent PSC, adopting a proactive approach to monitor and manage the condition can help manage symptoms and slow its progression. Below, we explore practical tips for monitoring and managing symptoms, outline preventative measures, and highlight the importance of regular medical checkups and patient education.
Tips for Monitoring and Managing Symptoms
- Regular Liver Function Tests: Routine blood tests can help monitor liver function and detect early signs of worsening conditions.
- Symptom Diary: Keeping a diary of symptoms can help you and your healthcare provider identify triggers and monitor changes over time.
- Nutritional Support: Consulting with a dietitian to ensure a balanced diet that supports liver health and overall well-being.
- Avoid Alcohol and Toxins: Alcohol can exacerbate liver disease. Avoiding it, along with other liver toxins like certain medications and environmental toxins, is crucial.
- Exercise Regularly: Moderate exercise can help maintain liver health and manage symptoms like fatigue.
Preventative Measures
Although PSC cannot be prevented due to its unknown exact causes, certain actions may help reduce the risk of complications:
- Vaccinations: Stay up to date with vaccinations, especially for Hepatitis A and B, which can prevent infections that may further damage the liver.
- Regular Screening for Complications: Regular screenings for cholangiocarcinoma, a type of cancer associated with PSC, and other complications can help catch issues early when they are more treatable.
- Manage Associated Conditions: Many people with PSC also have inflammatory bowel disease (IBD). Managing IBD effectively can potentially slow the progression of PSC.
Importance of Regular Medical Check-ups and Patient Education
- Early Detection and Treatment: Regular check-ups allow for the early detection and management of PSC and its complications. This proactive approach can significantly affect the quality of life and prognosis.
- Patient Education: Understanding PSC, its potential complications, and treatment options empowers patients to take an active role in their healthcare. Education on the disease process and potential warning signs of complications is vital.
- Building a Healthcare Team: Establishing a relationship with a healthcare team that specializes in liver diseases can provide specialized care tailored to the needs of PSC patients.
Regular dialogue with healthcare providers, staying informed about the latest research, and a supportive care network are essential components of effective disease management.
FAQs about Primary Sclerosing Cholangitis Symptoms
What is primary sclerosing cholangitis (PSC)?
Primary sclerosing cholangitis (PSC) is a chronic liver disease where inflammation and scarring affect the bile ducts, leading to bile buildup and liver damage. It is often linked with inflammatory bowel diseases like ulcerative colitis.
What are the early symptoms of PSC?
Early symptoms of PSC may be mild or absent. Some individuals might experience fatigue, itching, or discomfort in the upper right part of the abdomen. Due to its subtle onset, PSC can go unnoticed in the initial stages.
Does PSC cause jaundice?
Yes, as PSC progresses, it can obstruct bile flow, leading to jaundice. This is characterized by yellowing of the skin and eyes, dark urine, and pale stool. Jaundice indicates significant liver dysfunction and requires medical attention.
Are there any specific symptoms that differentiate PSC from other liver diseases?
PSC is particularly associated with recurrent episodes of cholangitis, an infection of the bile ducts, which is less common in other liver diseases. Symptoms of cholangitis include fever, chills, and upper abdominal pain.
Can PSC symptoms fluctuate over time?
Yes, the symptoms of PSC can fluctuate. Some patients experience periods of relative wellbeing interspersed with bouts of worsening symptoms, especially during episodes of cholangitis.
How is PSC diagnosed through its symptoms?
Symptoms alone are not sufficient for diagnosing PSC. Diagnosis typically involves blood tests, imaging studies like MRCP (Magnetic Resonance Cholangiopancreatography) or ERCP (Endoscopic Retrograde Cholangiopancreatography), and sometimes a liver biopsy. These tests help visualize the bile ducts and assess liver health.
When should someone seek medical advice for PSC symptoms?
Seek medical advice if you experience symptoms like severe itching, jaundice, significant fatigue, or abdominal pain. Early consultation can lead to timely diagnosis and management of PSC and its complications.
Conclusion
Understanding the symptoms and recognizing the causes of Primary Sclerosing Cholangitis (PSC) is crucial for early diagnosis and effective management of this chronic liver disease. Symptoms such as jaundice, itching, and fatigue should not be overlooked, as they are key indicators of potential liver dysfunction. Given the complexity of PSC and its possible progression to more severe liver conditions, it is vital to stay informed about its manifestations.
If you or someone you know is experiencing symptoms related to PSC, prompt consultation with healthcare providers is essential. Healthcare professionals can offer comprehensive evaluations and tailor treatment plans that address both the symptoms and the progression of the disease. Remember, early intervention can significantly improve the quality of life for those affected by Primary Sclerosing Cholangitis.
References
For those seeking further information on primary sclerosing cholangitis (PSC) symptoms, the following references provide reputable sources and additional insights. These links offer detailed explanations and validate the information discussed, enhancing understanding of this complex liver condition.
- Mayo Clinic – Primary Sclerosing Cholangitis Overview: This comprehensive guide from the Mayo Clinic offers an in-depth look at PSC, covering symptoms, causes, and treatment options. Read more about PSC on Mayo Clinic.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Liver Diseases: NIDDK provides a detailed section on liver diseases, including primary sclerosing cholangitis. Their resources are scientifically accurate and helpful for understanding the medical perspective on PSC. Explore NIDDK resources on liver diseases.
- American Liver Foundation – Primary Sclerosing Cholangitis: The American Liver Foundation offers resources tailored to patients and caregivers, focusing on symptom management and daily living with PSC. Visit the American Liver Foundation.
- PubMed Central: For those interested in research and academic studies, PubMed Central provides access to numerous scientific papers on PSC. This is a valuable resource for detailed studies and latest findings. Search for PSC studies on PubMed Central.
These resources are chosen for their reliability and authority in the field of hepatology and are intended to provide readers with a solid foundation for understanding primary sclerosing cholangitis symptoms.