Peyronie Disease Symptoms: Peyronie’s disease is a medical condition characterized by the development of fibrous scar tissue inside the penis, which can lead to a variety of symptoms including significant bending, pain, and erectile dysfunction.
This condition can impact a man’s ability to engage in sexual activity and may also cause psychological distress.
Understanding the symptoms and causes of Peyronie’s disease is crucial for timely diagnosis and management.
Understanding Peyronie’s Disease
Peyronie’s disease is a medical condition characterized by the development of fibrous scar tissue inside the penis, leading to curved, painful erections. This curvature can make sexual intercourse difficult or even impossible in severe cases. Understanding the prevalence and demographics affected by Peyronie’s disease is crucial for recognizing its impact on men’s health globally.
Prevalence of Peyronie’s Disease
Peyronie’s disease affects a significant number of men, though exact figures vary due to underreporting and variations in study methodologies. Research suggests that Peyronie’s disease may affect between 3% to 9% of men. However, some studies indicate the prevalence might be as high as 13% when including milder or undiagnosed cases. The incidence of Peyronie’s disease appears to increase with age, particularly in men over 40 years old, though it can occur in younger men as well.
Demographics Affected
Peyronie’s disease primarily affects middle-aged and older men, but it is not exclusive to these age groups. It is rare in young men but can still occur. The condition is most commonly diagnosed in men between the ages of 40 and 70. Certain risk factors are associated with a higher likelihood of developing Peyronie’s disease, including:
- Genetic predisposition: There is evidence suggesting that Peyronie’s disease may run in families, indicating a genetic component to the risk.
- Medical conditions: Men with certain health issues, such as diabetes, Dupuytren’s contracture, and certain connective tissue disorders, are at increased risk.
- Lifestyle factors: Behaviors that cause repeated injury to the penis, such as intense physical activity or certain sexual practices, can increase the risk of developing scar tissue.
However, understanding these demographics helps in identifying and managing Peyronie’s disease effectively, emphasizing the importance of awareness and appropriate medical consultation for those experiencing symptoms.
Symptoms of Peyronie’s Disease
Understanding the symptoms of Peyronie’s disease can help individuals recognize the condition early and seek appropriate treatment. Below, we explore the early signs, the progression of symptoms, and how these symptoms can affect sexual function and emotional well-being.
Early Signs and Symptoms
The onset of Peyronie’s disease may initially be subtle and gradually become more noticeable. Early signs include:
- Small, localized swelling: The first indication might be a small, localized area of swelling or a noticeable lump on the penis, which is the developing scar tissue.
- Pain: In its early stages, Peyronie’s disease can cause pain during erections or even when the penis is flaccid.
- Curvature begins: As the scar tissue forms, it may start to cause a noticeable bend or curvature in the penis, which is often more apparent during an erection.
These initial symptoms might not seem severe but can progress, significantly impacting an individual’s quality of life.
Progression of Symptoms
As Peyronie’s disease advances, the symptoms may become more pronounced and disruptive:
- Increased curvature: The curvature of the penis may increase, becoming more pronounced and possibly leading to a deformed appearance.
- Shortening of the penis: Some men may notice a shortening of their penis, which is due to the pulling effect of the internal scar tissue.
- Erectile dysfunction: The physical changes can interfere with sexual function, making it difficult to maintain an erection.
- Pain intensifies: While the pain may decrease over time for some, others may experience persistent or worsening pain.
This progression can vary significantly from person to person, with some experiencing mild symptoms and others facing more severe and obstructive changes.
Impact on Sexual Function and Emotional Well-Being
The symptoms of Peyronie’s disease can have profound effects on both sexual function and emotional health:
- Sexual challenges: The curvature and pain associated with Peyronie’s can make sexual intercourse painful or even impossible, leading to difficulties in maintaining intimate relationships.
- Emotional distress: The physical limitations imposed by the disease often lead to significant emotional distress. Men may experience feelings of embarrassment, anxiety, or depression due to the changes in their sexual abilities and physical appearance.
- Relationship stress: The strain on sexual relationships can extend into broader emotional and psychological challenges, impacting overall life satisfaction and partner relationships.
If you or someone you know is experiencing these symptoms, consulting a healthcare professional for a proper diagnosis and personalized treatment plan is essential.
Causes and Risk Factors of Peyronie’s Disease
Understanding the causes and risk factors associated with this condition can help in managing and potentially mitigating its impact.
Causes of Peyronie’s Disease
The exact causes of Peyronie’s disease are not fully understood, but it is generally believed to stem from repeated injury to the penis. Such injuries may not always be significant or remembered, and they can include:
- Physical trauma – Accidents, sports injuries, or vigorous sexual activity can damage the penile tissue, leading to scar formation as it heals.
- Genetic factors – There is some evidence suggesting that Peyronie’s disease might have a genetic component, as it sometimes occurs in men with a family history of the condition.
Risk Factors of Peyronie’s Disease
Several risk factors can increase the likelihood of developing Peyronie’s disease:
- Age – Peyronie’s disease is more common in men over the age of 40, likely due to decreased tissue elasticity and other age-related changes.
- Connective tissue disorders – Men with certain genetic disorders affecting connective tissue, such as Dupuytren’s contracture, are at higher risk.
- Previous penile injury – A history of penile trauma, even if it didn’t initially result in Peyronie’s disease, can predispose an individual to develop the condition later on.
- Certain health conditions – Diseases like diabetes and heart disease, which affect blood flow and tissue integrity, can also increase risk.
Lifestyle Habits That Might Influence Risk
Lifestyle choices can influence the risk of developing Peyronie’s disease or affect its severity:
- Smoking – Smoking can impair blood flow and tissue health, potentially exacerbating the condition.
- Alcohol consumption – Excessive alcohol intake can lead to various health issues that may indirectly influence the risk of developing Peyronie’s disease.
- Exercise – Regular physical activity might help improve blood flow and overall health, potentially reducing the risk of tissue damage.
However, adopting healthier lifestyle choices, being aware of the risks associated with certain activities, and seeking medical advice when necessary can all help manage or prevent the condition.
Complications Associated with Peyronie’s Disease
Understanding these complications is crucial for managing the condition effectively and seeking appropriate treatment. Here, we explore the major complications associated with Peyronie’s disease.
Erectile Dysfunction
One of the most common complications of Peyronie’s disease is erectile dysfunction (ED). The scar tissue can cause deformities in the penis, such as curvature or indentations, which may hinder the ability to achieve or maintain an erection sufficient for intercourse. This physical barrier to sexual function can be distressing and may require medical intervention to manage effectively.
Challenges in Sexual Relationships
Peyronie’s disease can severely impact sexual relationships. The physical changes in the penis might make sexual intercourse painful or difficult, which can lead to decreased sexual activity. Partners may also feel distressed about the change in their sexual dynamics, which can strain the relationship further. Open communication and counseling might be necessary to navigate these challenges effectively.
Emotional and Psychological Impact
The emotional and psychological effects of Peyronie’s disease are significant and often overlooked. Men may experience feelings of embarrassment, anxiety, or depression due to the physical symptoms and the changes in their sexual performance and relationships. The stigma surrounding sexual health issues can further exacerbate these feelings, making it important for affected individuals to seek support from mental health professionals, support groups, or therapy.
However, while Peyronie’s disease primarily affects the physical aspect of the penis, its complications can ripple through a man’s sexual function, relationships, and emotional wellbeing. Recognizing and addressing these issues early with the help of healthcare providers can improve outcomes and quality of life.
Diagnosing Peyronie’s Disease
Diagnosing this condition accurately is crucial for effective management and treatment. Here’s how medical professionals typically diagnose Peyronie’s Disease, focusing on medical history, physical examinations, and the use of imaging and other diagnostic tools.
Medical History and Physical Examinations
- Medical History: The first step in diagnosing Peyronie’s Disease involves a detailed medical history. Doctors will ask about the onset of symptoms, the presence of pain, the degree of curvature, and any difficulties with sexual intercourse. Understanding the patient’s health history, including any previous injuries to the genital area or surgeries, is also crucial. This helps in assessing whether the symptoms are due to Peyronie’s Disease or other conditions like erectile dysfunction or congenital curvature.
- Physical Examination: A physical examination is essential to confirm the diagnosis of Peyronie’s Disease. During the exam, the doctor will look for palpable scar tissue, or plaques, on the penis. The examination is usually performed when the penis is flaccid and may include manipulating the penis to better understand the location and extent of the curvature.
Imaging and Other Diagnostic Tools
- Ultrasound: This is the most common imaging test used to diagnose Peyronie’s Disease. Penile ultrasound provides images of the penis in both its flaccid and erect states (often induced by an injection). It helps in identifying the presence and severity of plaques, penile curvature, and other abnormalities like erectile dysfunction. Ultrasound can also measure blood flow to the penis, which is useful for planning treatment.
- X-ray: Although less common, an X-ray of the penis can help visualize the extent of calcification in the plaques, if any. This method is usually employed in advanced cases where the calcified plaques are suspected.
- MRI: Magnetic Resonance Imaging (MRI) of the penis is another tool that might be used, although it’s less common than ultrasound. MRI can provide detailed images of both the soft tissues and the blood vessels in the penis, offering valuable information about the plaque’s characteristics and exact location.
By combining information from a patient’s medical history, physical exam findings, and diagnostic imaging, healthcare providers can accurately diagnose Peyronie’s Disease and tailor a treatment approach that best suits the individual’s condition.
Treatment Options for Peyronie’s Disease
Treatment options for Peyronie’s Disease vary from non-surgical approaches to surgical interventions, depending on the severity of the symptoms and the stage of the disease. Here’s a comprehensive guide to the available treatments.
Non-Surgical Treatments
Non-surgical treatments are typically considered for men who experience less severe curvature or pain, and whose condition is in the early stages or has not progressed significantly. These options include:
- Medications: Oral medications like pentoxifylline or potassium para-aminobenzoate can help manage symptoms or slow the progression of the disease in some men. Topical treatments with verapamil gel may also be prescribed to reduce pain and curvature.
- Injections: Collagenase Clostridium histolyticum (brand name Xiaflex) is an FDA-approved injectable treatment for Peyronie’s Disease. It works by breaking down the buildup of collagen that causes penile curvature. Other injectable options include interferon alpha-2b and verapamil, which are believed to reduce fibrosis and improve elasticity.
- Shockwave Therapy: This method uses sound waves to potentially break apart the scar tissue in the penis, reducing pain and improving function. While promising, more research is needed to fully understand its effectiveness.
- Penile Traction Therapy: Devices that stretch the penis can be used to reduce curvature and lengthen the penis. Consistent use of these devices has shown to be beneficial in some cases, especially when used in conjunction with other treatments.
- Vacuum Devices: These devices can help in reducing curvature and maintaining erectile function by drawing blood into the penis and encouraging straightening over time.
Surgical Options
Surgery may be considered when Peyronie’s Disease has caused severe curvature or pain that significantly interferes with sexual function or quality of life, and when symptoms have not improved with non-surgical treatments. Surgical options include:
- Nesbit Procedure: This involves the removal or alteration of tissue from the side of the penis opposite the plaque, which helps to straighten the penis. It’s effective but can lead to a shortening of the penis.
- Plaque Excision and Grafting: In this procedure, surgeons remove the scar tissue and replace it with a graft. This option is suitable for men with more complex or severe curvatures and aims to maintain penile length.
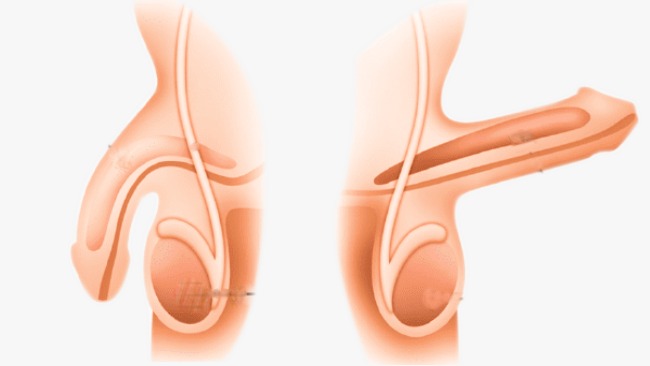
- Penile Implant: For men with Peyronie’s Disease who also suffer from erectile dysfunction, a penile prosthesis may be an option. This procedure involves the placement of a device that can help achieve and maintain an erection and can also help straighten the penis.
- Plication: This simpler surgical technique involves suturing the longer side of the penis to match the shortened, scarred side, effectively reducing the curvature. This method is less invasive but may also result in a slight shortening of the penis.
However, choosing the right treatment for Peyronie’s Disease depends on a variety of factors, including the severity of the symptoms, the stage of the disease, and the patient’s overall health and preferences.
Managing Life with Peyronie’s Disease
Living with Peyronie’s Disease can be challenging, but understanding how to manage symptoms effectively and finding the right support can make a significant difference. Here are practical strategies for dealing with this condition.
Lifestyle Adjustments for Managing Symptoms
- Physical Activities: Engaging in gentle, non-strenuous physical activities can help maintain overall health without exacerbating symptoms. Consult with a healthcare professional to identify safe exercises.
- Dietary Considerations: Focus on a balanced diet rich in anti-inflammatory foods such as fruits, vegetables, nuts, and fish. These can help manage pain and swelling associated with Peyronie’s Disease.
- Avoidance of Certain Activities: Some activities, including specific sexual positions or exercises, might aggravate the condition. It’s crucial to understand and avoid these triggers.
- Use of Medical Devices: In some cases, doctors might recommend using devices like penile traction devices to help reduce curvature and maintain penile length.
- Stress Management: Chronic stress can worsen symptoms, so incorporating stress-reduction techniques such as mindfulness, yoga, or meditation can be beneficial.
Support Systems and Counseling
- Professional Counseling: Talking to a mental health professional can help individuals cope with the emotional and psychological impacts of Peyronie’s Disease.
- Support Groups: Joining a support group, whether online or in person, allows individuals to connect with others facing similar challenges. These groups provide a platform for sharing experiences and coping strategies.
- Partner Support: Open communication with one’s partner is essential for managing the relationship dynamics affected by Peyronie’s Disease. Couples counseling might also be beneficial.
- Educational Resources: Utilizing resources provided by health organizations can help patients and their families understand the disease better and keep informed about new treatments or management strategies.
Future Outlook and Ongoing Research
- Advancements in Treatment: Ongoing research is continually improving the treatment options available for Peyronie’s Disease. These include new medications, therapies, and surgical techniques aimed at reducing symptoms and improving quality of life.
- Genetic Research: Scientists are exploring the genetic factors that may contribute to the development of Peyronie’s Disease, which could lead to targeted therapies in the future.
- Long-term Studies: Longitudinal studies are helping to better understand the progression of Peyronie’s Disease and its long-term impact on patients’ lives, potentially guiding future therapeutic approaches.
- Patient Education: As research progresses, educational programs are updated to provide patients and healthcare providers with the latest information and management techniques.
By embracing lifestyle adjustments, leveraging support systems, and staying informed about ongoing research, individuals living with Peyronie’s Disease can lead fulfilling lives despite the challenges posed by the condition.
FAQs about Peyronie’s Disease Symptoms
What are the primary symptoms of Peyronie’s Disease?
The primary symptom of Peyronie’s Disease is the development of fibrous scar tissue inside the penis, which can lead to curved, painful erections. Other symptoms may include changes in the shape of the penis, such as narrowing or shortening, and erectile dysfunction.
How soon do symptoms of Peyronie’s Disease appear?
Symptoms of Peyronie’s Disease can appear suddenly or develop gradually over time. The curvature of the penis is often most noticeable during an erection and can progress or stabilize over time.
Does Peyronie’s Disease always cause pain?
Not always. While many men experience pain, especially during the initial stages of the disease, the pain tends to decrease over time. Some men may not experience pain at all, but still notice penile curvature and other deformities.
Can Peyronie’s Disease affect sexual function?
Yes, Peyronie’s Disease can significantly affect sexual function. The curvature and discomfort can make sexual intercourse difficult or painful, which can lead to erectile dysfunction and decreased sexual satisfaction.
Are there any visible signs of Peyronie’s Disease when the penis is not erect?
Yes, in some cases, there can be visible abnormalities even when the penis is not erect. These may include indentations, a narrow band around the shaft, or a lumpy appearance from the scar tissue.
Is the curvature from Peyronie’s Disease permanent?
The curvature caused by Peyronie’s Disease can be permanent if not treated. In some cases, the curvature may improve or worsen over time. Treatment options are available that can help reduce the curvature and alleviate symptoms.
Should I see a doctor if I suspect Peyronie’s Disease?
Yes, if you notice any abnormalities in the shape of your penis or experience pain during erections, it’s important to consult a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve outcomes.
Conclusion
Understanding the early symptoms of Peyronie’s Disease is crucial for timely and effective management of the condition. Recognizing signs such as pain during erections, noticeable curvature of the penis, or the formation of hard lumps can be pivotal in seeking early intervention.
It’s important to address these symptoms promptly by consulting healthcare professionals who specialize in men’s health. Early diagnosis and treatment not only improve the likelihood of successful outcomes but also help in preventing the progression of the disease.
If you or someone you know is experiencing any symptoms suggestive of Peyronie’s Disease, do not hesitate to seek expert medical advice. Taking action early can make a significant difference in health outcomes and quality of life.
References
For those seeking more detailed information on Peyronie’s disease and to validate the symptoms discussed, the following reputable sources are recommended. These resources provide in-depth knowledge and are recognized for their authority in the medical field.
- Mayo Clinic: Offers a comprehensive overview of Peyronie’s disease, including symptoms, causes, and treatment options. Read more about Peyronie’s Disease on Mayo Clinic.
- Cleveland Clinic: Provides detailed articles on the diagnosis and management of Peyronie’s disease. Explore Peyronie’s Disease resources at Cleveland Clinic.
- WebMD: Features articles that cover a wide range of topics related to Peyronie’s disease, including symptom recognition and treatment advice. Visit WebMD for more information on Peyronie’s Disease.
- National Institutes of Health (NIH): Offers research papers and articles that delve into the clinical aspects of Peyronie’s disease. Access NIH resources on Peyronie’s Disease.
- PubMed: A valuable resource for accessing scientific studies and research reviews on Peyronie’s disease. Search for Peyronie’s Disease studies on PubMed.
These sources are excellent starting points for those interested in gaining a deeper understanding of Peyronie’s disease and its symptoms. They provide reliable and current information that is crucial for patients and healthcare providers alike.