Pancreatitis Treatment: Pancreatitis is a complex medical condition where the pancreas becomes inflamed, causing significant pain and dysfunction.
This inflammation can be acute, appearing suddenly and lasting days, or chronic, persisting for years.
Understanding the nuances of diagnosing and treating this condition is crucial for effective management and improving patient outcomes.
Understanding Pancreatitis
Pancreatitis is a medical condition characterized by the inflammation of the pancreas, a vital organ that lies behind the stomach and near the first part of the small intestine. The pancreas plays a crucial role in digestion and hormone production, especially insulin, which regulates blood sugar levels. Understanding the types of pancreatitis and recognizing its prevalence can help in its timely diagnosis and management.
Types of Pancreatitis
Pancreatitis manifests in two main forms:
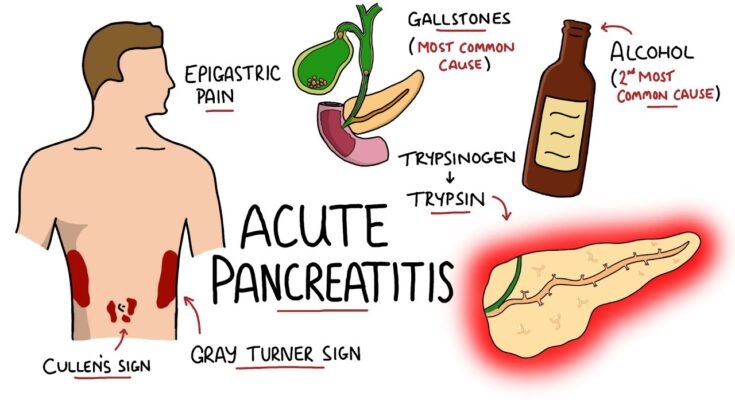
- Acute Pancreatitis: This form occurs suddenly and can last for days. It can range from mild discomfort to severe, life-threatening illness. The most common causes are gallstones and excessive alcohol consumption, but it can also be triggered by certain medications, abdominal trauma, or infections.
- Chronic Pancreatitis: Unlike acute pancreatitis, chronic pancreatitis develops over many years. It is a persistent inflammation that results in permanent damage and scarring of the pancreas, leading to decreased function and problems with digestion and blood sugar regulation. Chronic pancreatitis is often caused by prolonged alcohol abuse, genetic disorders, or as a complication of acute pancreatitis.
Statistics and Prevalence
Pancreatitis is a relatively common condition affecting a wide range of individuals:
- Acute Pancreatitis: It is one of the most frequent gastrointestinal causes for hospital admission in the United States. Each year, acute pancreatitis affects about 40 to 50 per 100,000 adults.
- Chronic Pancreatitis: This condition is less common than its acute counterpart, with an estimated prevalence of about 50 cases per 100,000 individuals annually. However, the prevalence can vary significantly depending on geographic and demographic factors.
- Demographic Variability: The incidence of pancreatitis is higher in men than in women, particularly in the context of alcohol-related pancreatitis. Moreover, certain genetic predispositions can influence the likelihood of developing this condition, particularly in chronic cases.
However, understanding the types and prevalence of pancreatitis is crucial for awareness and early intervention, which can significantly impact the prognosis and quality of life for those affected by the disease.
Causes and Risk Factors of Pancreatitis
Understanding the common causes and risk factors associated with each type is crucial for prevention and management. Additionally, lifestyle factors such as alcohol consumption, smoking, and dietary habits significantly impact the development and progression of this condition.
Common Causes of Acute Pancreatitis
Acute pancreatitis often occurs suddenly and can range from mild discomfort to a severe, life-threatening illness. Some of the most common causes include:
- Gallstones: These are the leading cause of acute pancreatitis. They can block the bile duct, which shares an opening with the pancreatic duct, disrupting pancreatic function.
- Alcohol Consumption: Heavy alcohol use can trigger acute pancreatitis and is a major cause in many cases.
- Medications: Certain medications, including some diuretics, antibiotics, and chemotherapy agents, can induce pancreatitis.
- High Triglyceride Levels: Extremely high levels of triglycerides in the blood can lead to acute pancreatitis.
- Abdominal Surgery or Trauma: Physical injury to the abdomen or recent surgical procedures can precipitate an episode of acute pancreatitis.
Common Causes of Chronic Pancreatitis
Chronic pancreatitis, on the other hand, is a long-lasting condition that particularly affects individuals who have had multiple episodes of acute pancreatitis. Its causes include:
- Repeated Alcohol Consumption: Prolonged alcohol abuse is the most common cause of chronic pancreatitis in adults.
- Genetic Disorders: Certain genetic mutations can predispose individuals to develop chronic pancreatitis.
- Cystic Fibrosis: This genetic disorder can affect the pancreas, among other organs.
- Autoimmune Issues: In some cases, the body’s immune system attacks the pancreas, leading to chronic inflammation.
Risk Factors of Pancreatitis
Risk factors that increase the likelihood of developing either acute or chronic pancreatitis include:
- Alcoholism: Regular, excessive alcohol consumption is a significant risk factor.
- Smoking: Tobacco use is strongly linked to the development of chronic pancreatitis and can exacerbate the severity of the condition.
- Obesity: Excessive body weight increases the risk of gallstones, which can lead to acute pancreatitis.
- Family History: A family history of pancreatitis increases the risk, suggesting a genetic predisposition to the disease.
Impact of Alcohol, Smoking, and Dietary Habits
- Alcohol: Alcohol can cause direct pancreatic toxicity and induces acute pancreatitis after periods of heavy drinking and is the most common cause of chronic pancreatitis.
- Smoking: Smoking not only increases the risk of developing pancreatitis but also accelerates the progression to chronic pancreatitis. It is also associated with a higher risk of pancreatic cancer.
- Dietary Habits: High-fat diets and diets rich in processed foods can increase triglyceride levels, thus raising the risk of acute pancreatitis. Conversely, a balanced diet rich in fruits, vegetables, and whole grains can help manage and prevent flare-ups.
However, understanding and mitigating these risk factors through lifestyle changes can significantly reduce the likelihood of developing pancreatitis and help manage the symptoms in those already affected.
Symptoms of Pancreatitis
Recognizing the early signs and knowing when to seek medical help can be crucial for effective treatment and management. Below, we explore the early symptoms of pancreatitis and provide guidance on when it is essential to consult a healthcare professional.
Early Signs and Symptoms of Pancreatitis
The onset of pancreatitis symptoms can be sudden or gradual, depending on the type and severity of the condition. Here are the early signs to watch for:
- Upper Abdominal Pain: Often described as a severe, dull ache radiating to the back, this pain may increase after eating, especially foods high in fat.
- Abdominal Tenderness: The abdomen might feel tender to the touch and swollen.
- Nausea and Vomiting: These are common symptoms that accompany abdominal pain and discomfort.
- Fever: A mild fever can often accompany other symptoms of pancreatitis.
- Increased Heart Rate: Some individuals might experience a rapid pulse, especially if the inflammation is causing internal stress.
- Jaundice: In some cases, the skin and the whites of the eyes may turn yellowish, indicating that the pancreas is not functioning properly.
These symptoms can often be mistaken for less serious conditions, so it’s important to be aware of the intensity and duration of these signs.
When to Seek Medical Help
Immediate medical attention is required if you or someone you know experiences the following symptoms related to pancreatitis:
- Severe Abdominal Pain: If the abdominal pain is intense and does not go away, it’s critical to seek medical help promptly.
- Persistent Vomiting: Continuous vomiting that prevents keeping liquids down is a serious sign that needs immediate medical evaluation.
- Signs of Jaundice: Yellowing of the skin or eyes, especially if accompanied by other symptoms, requires urgent medical attention.
- Changes in Heart Rate: A significantly rapid or irregular heartbeat combined with other symptoms is a reason for immediate care.
- Sudden and Severe Symptoms: If the symptoms of pancreatitis appear suddenly and are severe, it’s essential to go to the emergency room or call emergency services.
However, pancreatitis is a condition that can escalate quickly and may lead to serious complications if not treated promptly. Early detection and timely medical intervention can significantly improve the outcomes.
Diagnosis of Pancreatitis
Diagnosing pancreatitis effectively is crucial as it enables timely and appropriate treatment, potentially preventing complications. Here’s a structured guide to understanding how pancreatitis is diagnosed, from the initial assessment to the use of advanced diagnostic techniques.
Initial Assessment and Medical History Evaluation
The diagnosis of pancreatitis begins with a comprehensive initial assessment and a detailed evaluation of the patient’s medical history. Here are the steps typically involved:
- Symptom Review: Healthcare providers start by identifying key symptoms of pancreatitis, such as severe abdominal pain, nausea, vomiting, fever, and rapid pulse.
- Medical History: Doctors assess risk factors and past medical history that could contribute to pancreatitis, including alcohol consumption, gallstones, recent medical procedures, and family history of pancreatic diseases.
- Physical Examination: A thorough physical exam is conducted to check for abdominal tenderness or swelling, which are common in patients with pancreatitis.
Key Diagnostic Tests and Imaging Techniques
Several diagnostic tests and imaging techniques are essential for confirming the presence of pancreatitis and assessing its severity:
- Blood Tests: These are crucial for measuring levels of amylase and lipase, enzymes that are typically elevated in patients with pancreatitis.
- Abdominal Ultrasound: This non-invasive test is used to identify gallstones and other abnormalities that might cause pancreatitis.
- Computed Tomography (CT) Scan: A CT scan provides detailed images of the pancreas, helping to assess the extent of inflammation and detect complications.
- Magnetic Resonance Imaging (MRI): MRI is used for obtaining detailed images of the bile ducts, pancreas, and surrounding structures.
The Role of Endoscopic Procedures in Diagnosis
Endoscopic procedures play a significant role in the diagnosis of pancreatitis, particularly when biliary causes are suspected:
- Endoscopic Ultrasound (EUS): This procedure involves the use of a small ultrasound device on the tip of an endoscope, which is inserted through the mouth and into the stomach to obtain close-up images of the pancreas and bile ducts.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP is both a diagnostic and therapeutic procedure. It involves the insertion of an endoscope through the mouth to the small intestine, where dye is injected into the pancreatic and bile ducts. X-rays are then taken to look for blockages or abnormalities.
However, by combining these diagnostic approaches, healthcare professionals can accurately diagnose pancreatitis, assess its severity, and plan effective treatment strategies.
Treatment Options for Pancreatitis
Pancreatitis, the inflammation of the pancreas, requires prompt medical attention to manage symptoms and prevent complications. Here, we explore various treatment options tailored to the severity and type of pancreatitis—acute or chronic.
Immediate Treatments to Manage Symptoms
Initial treatment for pancreatitis often involves hospitalization to stabilize the patient’s condition. The primary goals are to relieve pain and manage fluid loss. Patients are generally advised to refrain from eating and drinking for a few days to allow the pancreas to recover. Intravenous (IV) fluids are administered to prevent dehydration, and medications may be given for pain relief.
Detailed Discussion on Pancreatitis Treatment Approaches
Medications:
- Pain Relievers: Over-the-counter pain medications like acetaminophen or ibuprofen are commonly used. In more severe cases, stronger pain medications may be prescribed by a healthcare provider.
- Enzyme Supplements: To aid digestion and reduce the workload on the pancreas, enzyme supplements such as pancrelipase may be recommended.
- Antibiotics: If an infection is suspected or confirmed, antibiotics are essential to treat the infection and prevent further complications.
Nutritional Management and Dietary Changes:
Diet plays a crucial role in managing and recovering from pancreatitis. Initially, patients may need to avoid solid food to reduce pancreatic stimulation. Once inflammation subsides, a low-fat, high-nutrition diet is typically recommended. Dietitians may advise:
- Small, frequent meals to ensure nutritional needs are met without overworking the pancreas.
- Avoiding alcohol and smoking, as both can exacerbate the condition.
- Incorporating healthy fats like avocados and olive oil, while steering clear of fried and processed foods.
Surgical Interventions for Severe Cases:
In cases where complications like cysts or necrosis occur, surgical intervention may be necessary. Procedures may include:
- Cholecystectomy: Removal of the gallbladder if gallstones are causing pancreatitis.
- Pancreatic Necrosectomy: Removal of dead or infected pancreatic tissue.
- Endoscopic procedures: These minimally invasive procedures can drain cysts or blockages in the bile ducts.
Importance of Treating Underlying Conditions
Effectively managing underlying conditions such as gallstones, high triglyceride levels, or alcohol dependency is crucial for the treatment and prevention of pancreatitis. Addressing these issues can reduce the risk of recurrence and help maintain pancreatic health.
By adopting a comprehensive treatment strategy that includes immediate symptom management, medication, dietary adjustments, and possibly surgery, individuals with pancreatitis can manage their symptoms and work towards recovery. Collaboration with gastroenterologists, dietitians, and other specialists is essential to tailor treatment plans to individual needs and improve outcomes.
Managing Chronic Pancreatitis
Effective management of chronic pancreatitis involves a combination of treatment strategies, lifestyle modifications, and supportive therapies. Below, we detail the best approaches to handle this condition, aiming to improve quality of life and reduce symptoms.
Long-term Treatment Strategies
- Pain Management: Since chronic pancreatitis often causes severe pain, pain management is crucial. This may include prescribed medications such as pancreatic enzymes to reduce the strain on the pancreas, and non-steroidal anti-inflammatory drugs (NSAIDs) or opioids in more severe cases.
- Dietary Adjustments: Implementing a low-fat, high-protein, and low-carbohydrate diet can help manage symptoms and improve nutrient absorption.
- Pancreatic Enzyme Replacement Therapy (PERT): To aid digestion and improve nutrient absorption, patients are often prescribed pancreatic enzymes. This helps to decrease malnutrition and weight loss associated with chronic pancreatitis.
- Insulin Therapy: For those who develop diabetes as a complication of chronic pancreatitis, insulin therapy may be necessary to control blood glucose levels.
- Regular Monitoring: Regular visits with healthcare providers for monitoring the progression of the disease, managing complications, and adjusting treatments as needed are vital.
Lifestyle Modifications and Their Benefits
- Alcohol and Smoking Cessation: Avoiding alcohol and quitting smoking are paramount, as both can exacerbate the inflammation of the pancreas.
- Dietary Changes: Eating smaller, more frequent meals can help reduce the workload on the pancreas. It’s also beneficial to limit caffeinated beverages and spicy foods to prevent aggravating symptoms.
- Hydration: Staying hydrated is essential, as dehydration can worsen the condition. Drinking plenty of fluids throughout the day is recommended.
- Exercise: Regular, gentle exercise can improve overall health and help maintain a healthy weight, reducing the stress on the pancreas.
Supportive Therapies and Patient Education
- Mental Health Support: Chronic illnesses can take a toll on mental health. Support groups, counseling, and therapy can be beneficial.
- Nutritional Counseling: A dietitian can provide guidance tailored to the specific needs of those with chronic pancreatitis, helping to manage diet-related symptoms and improve quality of life.
- Patient Education: Educating patients about their condition, including how to manage flare-ups and prevent complications, is crucial. Knowledge empowers patients to take an active role in their treatment plan.
- Alternative Therapies: Some patients find relief in alternative therapies like acupuncture or yoga, which can help manage pain and stress associated with the disease.
However, continuous engagement with healthcare providers and adherence to prescribed treatments remain key components of effective management.
Complications of Pancreatitis
Pancreatitis, an inflammation of the pancreas, can lead to various complications that range from mild to life-threatening. It’s crucial for individuals diagnosed with this condition to understand the potential risks and how to mitigate them effectively.
Potential Complications and Their Impact
- Pseudocysts: Accumulations of fluid and debris in cyst-like pockets in the pancreas. These can cause persistent abdominal pain and may become infected.
- Infection: The pancreas can become infected, which might require surgical intervention or drainage to remove the infected tissue.
- Necrotizing Pancreatitis: Some of the pancreatic tissue dies due to inflammation. This serious complication can lead to systemic infection (sepsis) and multiple organ failure.
- Breathing Difficulties: Pancreatitis can affect lung function, leading to oxygen levels that are dangerously low, which may require supplemental oxygen or even mechanical ventilation in severe cases.
- Diabetes: Since the pancreas produces insulin, damage from pancreatitis can lead to diabetes, a serious condition that affects your body’s ability to manage blood sugar levels.
- Kidney Failure: In severe cases, pancreatitis can impair kidney function, potentially leading to temporary or permanent kidney failure.
- Pancreatic Cancer: Chronic pancreatitis is a risk factor for pancreatic cancer, a typically aggressive form of cancer.
Preventive Measures and Monitoring
Preventing complications from pancreatitis involves both lifestyle modifications and medical interventions. Here are essential strategies:
- Avoid Alcohol: Alcohol consumption is a significant risk factor for pancreatitis. Abstaining from alcohol can reduce the risk of recurrent episodes.
- Dietary Changes: Adopting a low-fat diet helps reduce the workload on the pancreas. Small, frequent meals can also be beneficial.
- Stop Smoking: Smoking is a risk factor for pancreatitis and its complications. Quitting smoking can significantly reduce these risks.
- Regular Monitoring: Frequent medical check-ups to monitor the function of the pancreas and detect any changes early are crucial.
- Medications: Utilizing medications to manage pain and treat underlying conditions like high triglycerides can help prevent flare-ups of pancreatitis.
- Hydration: Adequate hydration is vital, especially during episodes of pancreatitis, to help ensure proper bodily functions and reduce the risk of kidney problems.
- Education and Support: Understanding the condition and having access to support groups or counseling can help manage the stress and mental health aspects related to chronic illnesses.
By recognizing the potential complications and adhering to preventive measures, individuals with pancreatitis can manage their condition more effectively and reduce the risk of severe outcomes.
Advances in Pancreatitis Treatment
Pancreatitis, an inflammation of the pancreas, has seen promising advancements in both its understanding and treatment options. This progress is crucial as it affects numerous patients globally, presenting in acute or chronic forms. Below, we discuss the latest research and emerging therapies, along with innovations in surgical techniques and drug therapies.
Latest Research and Emerging Therapies
Recent research in pancreatitis treatment has focused on identifying novel therapeutic targets and developing more effective management strategies. One significant area of study is the role of gut microbiota in modulating the disease’s progression. Researchers are exploring how altering gut bacteria can influence inflammation and potentially decrease pancreatitis severity.
Another emerging therapy is the use of antioxidants and anti-inflammatory compounds. Studies have shown that certain antioxidants can help reduce oxidative stress and inflammation in the pancreas. Additionally, new biologic drugs that target specific inflammatory pathways are in the trial phase, offering hope for more targeted and effective treatments.
Innovations in Surgical Techniques and Drug Therapies
Surgical techniques for treating pancreatitis have also evolved. Minimally invasive procedures, such as endoscopic ultrasound-guided drainage, have become more common. These methods offer fewer complications and shorter recovery times compared to traditional surgery. Innovations such as robotic surgery provide greater precision and flexibility during operations, potentially improving outcomes for patients with complex pancreatic issues.
On the pharmacological front, there are several innovative drug therapies under development. These include new enzyme replacement therapies and pain management drugs specifically designed to address the unique needs of pancreatitis patients. The development of these drugs focuses on efficacy, reducing side effects, and improving the quality of life for those affected by the disease.
However, the advances in both research and clinical practices related to pancreatitis are rapidly evolving. These developments not only promise better management of the disease but also a greater understanding of its mechanisms, paving the way for more effective treatments in the future.
FAQs about Pancreatitis Treatment
What is the most common treatment for pancreatitis?
The most common treatments for pancreatitis focus on alleviating symptoms and preventing complications. These typically include fasting to rest the pancreas, IV fluids to prevent dehydration, and medications to manage pain. In more severe cases, surgery might be necessary to remove blockages or damaged tissue.
Can pancreatitis be treated at home?
Mild cases of acute pancreatitis can often be managed at home with guidance from healthcare professionals, which usually involves dietary modifications, hydration, and over-the-counter pain relief. However, it’s crucial to consult with a doctor before starting home treatment, as pancreatitis can sometimes worsen unexpectedly.
What dietary changes are recommended for someone with pancreatitis?
Diet plays a pivotal role in managing and recovering from pancreatitis. Patients are generally advised to eat a low-fat, high-nutrient diet. Small, frequent meals that are easy to digest can also help. Avoiding alcohol and smoking is strongly recommended, as these can exacerbate the condition.
How long does it take to recover from pancreatitis?
Recovery time varies depending on the severity of the pancreatitis. Acute pancreatitis may resolve in a week with proper treatment, while chronic pancreatitis may require ongoing management. It’s important to follow a healthcare provider’s instructions closely to manage symptoms effectively.
Are there any new treatments for pancreatitis on the horizon?
Research into pancreatitis treatment is ongoing. Recent advances include new drug therapies aimed at better managing pain and inflammation, as well as innovative surgical techniques to address the underlying causes of the condition. Always discuss the possibility of participating in clinical trials or new treatments with your healthcare provider.
Conclusion
Understanding and addressing pancreatitis with prompt and effective treatment is crucial for managing the condition’s severity and preventing further complications. This disease, characterized by the inflammation of the pancreas, can lead to significant health issues if not treated properly. It is essential for patients to recognize the importance of adhering to the medical advice provided by healthcare professionals.
We strongly encourage individuals diagnosed with pancreatitis to maintain regular check-ups and follow their treatment plans diligently. Regular monitoring and adherence to prescribed treatments enhance the effectiveness of the interventions and support better health outcomes. Remember, managing your condition proactively is the key to leading a healthier life.
References
For further reading and to validate the information provided on the treatment of pancreatitis, we recommend consulting the following reputable sources. These references offer detailed insights and the latest research findings to enhance your understanding of pancreatitis treatments:
- American Gastroenterological Association – This site provides comprehensive guidelines and the latest research on the treatment of pancreatitis. Read more about pancreatitis treatment guidelines here.
- Mayo Clinic – Known for its patient-friendly approach, Mayo Clinic offers an extensive overview of pancreatitis, including symptoms, causes, treatments, and managing lifestyle changes. Explore their pancreatitis section.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – NIDDK provides detailed information on the causes, treatment options, and preventive measures for pancreatitis. Learn more from their pancreatitis resources.
- Pancreas Foundation – Offers resources for patients and healthcare professionals about the latest treatment options and ongoing research in pancreatitis. Visit the Pancreas Foundation.
- PubMed Central – A free full-text archive of biomedical and life sciences journal literature. It is a valuable resource for finding scientific studies and reviews related to pancreatitis treatment. Search for pancreatitis studies on PubMed Central.
These resources are excellent starting points for anyone seeking in-depth information on the management and treatment of pancreatitis.