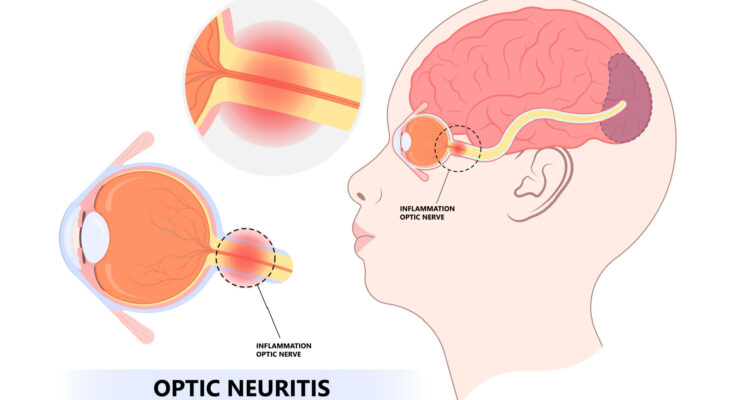
Optic Neuritis Symptoms: Optic neuritis is an inflammatory condition that affects the optic nerve, a crucial component responsible for transmitting visual information from the eyes to the brain.
This condition can lead to a temporary reduction in vision and may serve as an indicator of broader neurological issues, including multiple sclerosis (MS).
Understanding the symptoms and causes of optic neuritis is essential for timely diagnosis and treatment, which can significantly improve patient outcomes.
Understanding Optic Neuritis
Optic neuritis is a condition characterized by the inflammation of the optic nerve, which is crucial for vision. This inflammation can lead to symptoms such as pain on eye movement, blurred vision, and temporary vision loss. Understanding who is most at risk and how it fits into broader neurological conditions is essential for early detection and treatment.
Epidemiology: Who is Most at Risk?
Optic neuritis most commonly affects young adults between the ages of 20 and 40, with a higher prevalence among women. Individuals with specific genetic predispositions are also at a higher risk. Geographic factors play a role too; it is more frequently observed in populations located farther from the equator, suggesting a possible link with lower exposure to sunlight and subsequently lower levels of vitamin D.
Connection to Larger Neurological Conditions
Optic neuritis is often associated with demyelinating diseases such as multiple sclerosis (MS). In fact, it can be an initial sign of MS in many cases. The condition may also occur in isolation or be linked with other autoimmune disorders, highlighting its importance in the landscape of neurological health. This association underscores the need for comprehensive neurological evaluation when optic neuritis is diagnosed.
By recognizing the signs early and understanding the demographics at risk, better preventive strategies and treatments can be developed, improving outcomes for those affected by this challenging condition.
Symptoms of Optic Neuritis
Understanding these symptoms is crucial for early detection and effective management.
Primary Symptoms Linked to Optic Neuritis
The primary symptoms of optic neuritis are directly related to the inflammation of the optic nerve and typically develop rapidly over several hours to a few days. They include:
- Visual Loss: This is often the most noticeable symptom, where the individual experiences a reduction in vision. The severity can range from mild to severe and usually affects one eye.
- Pain: Many individuals report pain that worsens with eye movement. This discomfort is typically described as a dull ache behind the eye.
- Changes in Color Vision: There may be a noticeable reduction in the ability to perceive colors correctly. Colors might appear less vivid, or there might be difficulty distinguishing between shades.
- Visual Field Loss: Some people experience a loss of peripheral vision, which can create difficulties in seeing objects that are not directly in front.
Additional Symptoms and Less Common Presentations
While the primary symptoms cover the most common and significant effects of optic neuritis, there are additional signs that can occur:
- Flashing Lights: Some individuals see flashing or flickering lights, known as phosphenes.
- Visual Distortions: Objects may appear distorted in size, known as metamorphopsia.
- Prolonged Afterimages: After looking at a light source, a person might see an image of it for longer than usual.
How Symptoms May Differ Among Various Populations
The presentation of optic neuritis symptoms can vary widely among different populations:
- Age: Younger adults typically experience more acute symptoms, while older adults might have a more gradual onset.
- Gender: Women are more commonly affected by optic neuritis, potentially experiencing more severe symptoms, especially if linked to autoimmune disorders like multiple sclerosis.
- Ethnicity and Genetic Background: People of different ethnic backgrounds may experience variations in symptoms and prognosis. For instance, individuals of African descent might have a more severe course of optic neuritis compared to those of European descent.
- Underlying Health Conditions: Those with specific autoimmune conditions such as multiple sclerosis or neuromyelitis optica might experience recurrent episodes of optic neuritis with varying symptoms.
By being aware of the various symptoms and how they might differ among different groups, patients and healthcare providers can better recognize the early signs of optic neuritis, leading to timely and appropriate interventions.
Causes and Risk Factors of Optic Neuritis
Understanding the causes and risk factors of optic neuritis can help in early detection and management of this condition.
Causes of Optic Neuritis
Optic neuritis can occur due to a variety of underlying causes:
- Autoimmune Disorders: The most common cause of optic neuritis is an autoimmune response where the body’s immune system mistakenly attacks the optic nerve. This is often associated with multiple sclerosis (MS), where the immune system damages the protective sheath (myelin) surrounding nerve fibers.
- Infections: Certain viral and bacterial infections can lead to optic neuritis. Viruses such as measles, mumps, and herpes can trigger inflammation of the optic nerve. Bacterial infections, including syphilis and Lyme disease, might also be responsible.
- Other Diseases: Conditions like neuromyelitis optica (NMO) and sarcoidosis can also cause optic neuritis. NMO affects the eyes and the spinal cord, while sarcoidosis causes inflammation in various organs, including the eyes.
- Medications: Some drugs, particularly those that affect the immune system like interferon alpha and certain antibiotics, have been linked to the development of optic neuritis.
Risk Factors of Optic Neuritis
While anyone can develop optic neuritis, certain factors increase the risk:
- Age and Gender: Optic neuritis most frequently affects young adults aged 20 to 40 years, and it is more common in women than in men.
- Ethnicity: Studies have shown that individuals of Caucasian descent are at a higher risk of developing optic neuritis compared to other ethnic groups.
- Genetic Factors: A family history of autoimmune diseases can increase the risk of developing conditions like optic neuritis.
- Environmental Factors: Exposure to certain viral infections and possibly smoking might contribute to the increased risk of optic neuritis.
- Existing Autoimmune Conditions: People with autoimmune disorders such as multiple sclerosis or lupus are at a heightened risk of optic neuritis as part of their systemic immune-mediated attacks.
However, early intervention can significantly improve the management of optic neuritis and help prevent potential vision loss.
Diagnosis of Optic Neuritis
Timely and accurate diagnosis is crucial for effective treatment and management. Below, we explore the key diagnostic tests and procedures, the role of MRI in confirming the diagnosis, and the importance of differential diagnosis.
Key Diagnostic Tests and Procedures
- Visual Acuity Test: This basic test measures the clarity and sharpness of vision. It helps determine the extent of vision loss, which is common in optic neuritis.
- Pupillary Light Reflex Test: Evaluating the response of the pupil to light can indicate anomalies in the optic nerve, as a delayed or absent reflex may suggest optic neuritis.
- Color Vision Testing: Optic neuritis often impairs color vision, especially the perception of red hues. Testing this can provide additional clues to the diagnosis.
- Visual Field Test: This test assesses peripheral vision. Optic neuritis can cause specific patterns of visual field loss, aiding in its identification.
- Optical Coherence Tomography (OCT): This non-invasive imaging test captures detailed images of the retina, allowing doctors to observe its thickness and structure, which are often affected in optic neuritis.
- Visual Evoked Potential (VEP) Test: By measuring the electrical activity in the vision center of the brain following visual stimuli, VEP can indicate if there is a slowed response time due to optic nerve damage.
The Role of MRI in Confirming Diagnosis
Magnetic Resonance Imaging (MRI) plays a pivotal role in confirming the diagnosis of optic neuritis and ruling out other conditions that may mimic its symptoms, such as tumors or multiple sclerosis. An MRI can provide detailed images of the brain and optic nerve, revealing inflammation, demyelination (loss of the protective sheath around nerves), or other abnormalities. High-resolution scans can specifically detect changes in the optic nerve’s integrity and are useful in planning subsequent treatment strategies.
Importance of Differential Diagnosis
Differential diagnosis is vital for ensuring the appropriate management of optic neuritis. This process helps distinguish optic neuritis from other similar conditions such as:
- Ischemic Optic Neuropathy: Caused by reduced blood flow to the optic nerve.
- Neuromyelitis Optica: A distinct condition that also affects the spinal cord and optic nerve but requires different treatment.
- Infectious Optic Neuropathy: Resulting from infections like syphilis or Lyme disease.
A thorough differential diagnosis not only aids in confirming optic neuritis but also in identifying any underlying systemic diseases that could be contributing to the optic nerve inflammation.
Treatment Options for Optic Neuritis
Managing this condition effectively requires a comprehensive treatment approach tailored to alleviate symptoms and prevent further damage to the optic nerve. Below, we explore the standard treatments, common medications, and emerging therapies in the management of optic neuritis.
Standard Treatments and Their Objectives
The primary goals of treating optic neuritis include reducing inflammation, alleviating symptoms, and promoting recovery of vision. The standard treatment options are:
- Corticosteroids: These are the mainstay of treatment for acute optic neuritis to reduce inflammation and accelerate vision recovery. High-dose intravenous methylprednisolone is commonly administered, followed by a tapering course of oral steroids.
- Observation: In cases where symptoms are mild, doctors may recommend a watchful waiting approach. This involves closely monitoring the patient’s condition without immediate medical intervention, as some cases of optic neuritis may improve on their own.
- Plasma Exchange (Plasmapheresis): For severe cases of optic neuritis or cases not responding to steroid treatment, plasma exchange may be used. This procedure involves removing and treating the blood plasma, which can help reduce the immune system’s attack on the optic nerve.
Medications Commonly Used
The following medications are typically used in the treatment of optic neuritis:
- Intravenous Methylprednisolone: Used for severe cases to quickly reduce inflammation.
- Oral Prednisone: May be used after an initial course of intravenous steroids to taper the treatment.
- Pain Relievers: Over-the-counter pain relievers like ibuprofen or acetaminophen can be used to manage pain associated with optic neuritis.
Emerging Therapies and Research Directions
Research into optic neuritis is ongoing, with several promising therapies and research directions emerging:
- Immunomodulatory Treatments: These involve medications that modify the immune system’s response, potentially offering a more targeted approach to preventing optic nerve damage.
- Neuroprotective Agents: Researchers are exploring treatments that could protect nerve cells from damage during episodes of inflammation, potentially improving long-term outcomes.
- Biologics: These are advanced drugs derived from living organisms that target specific parts of the immune system. They are being investigated for their potential to treat autoimmune conditions, including those affecting the optic nerve.
- Stem Cell Therapy: This innovative approach involves using stem cells to regenerate or repair damaged tissues and nerves. Although still in the experimental stages, stem cell therapy holds promise for restoring vision lost due to optic neuritis.
- Clinical Trials: Patients with optic neuritis might also consider participating in clinical trials, which can provide access to cutting-edge treatments not yet widely available.
By staying informed about these developments, patients and healthcare providers can better navigate the complexities of treating optic neuritis, aiming for the best possible outcomes in vision recovery and quality of life.
Managing Life with Optic Neuritis
Optic neuritis, an inflammation of the optic nerve that can cause a sudden decrease in vision and color blindness, often requires not only medical treatment but also significant lifestyle adjustments and coping strategies. Here’s how individuals can manage life with optic neuritis effectively.
Lifestyle Adjustments and Home Remedies
- Prioritize Eye Rest: Reduce activities that strain the eyes, such as long periods of screen time. Use text-to-speech software when necessary to lessen the visual load.
- Optimize Lighting: Ensure that your reading and work environments are well-lit to help reduce eye strain. Adjustable desk lamps can provide targeted lighting without overwhelming the eyes.
- Diet and Supplements: Incorporate foods rich in antioxidants, such as leafy greens and berries, which may help support nerve health. Omega-3 fatty acids, found in fish like salmon, are also beneficial for overall eye health.
- Temperature Control: Avoid exposure to extreme temperatures, as heat can exacerbate symptoms. Use cool compresses to soothe the eyes when feeling discomfort.
- Vision Aids: Use aids like magnifiers or high-contrast settings on digital devices to help with vision impairment.
Coping Strategies and Support Systems
- Educate Yourself and Others: Understanding your condition can alleviate anxiety and help you communicate your needs better. Educate those around you to foster a supportive environment.
- Connect with Support Groups: Joining support groups, either online or in person, can connect you with others facing similar challenges. Sharing experiences and tips can be incredibly comforting and helpful.
- Professional Counseling: Consider therapy or counseling to manage the emotional and psychological impacts of living with a chronic condition. Professionals can provide coping mechanisms that ease the mental burden.
- Routine Medical Check-ups: Regular appointments with your healthcare provider are crucial. They can monitor your condition, adjust treatments, and provide guidance on managing symptoms.
Long-term Management and Prognosis
- Regular Monitoring: Long-term management of optic neuritis often involves ongoing monitoring of vision and general neurological health to catch any changes promptly.
- Adaptive Techniques: As symptoms evolve, learning new skills to adapt to changes in vision can help maintain independence and quality of life. Occupational therapy may be beneficial.
- Medication Management: For some individuals, long-term use of medication may be necessary to control inflammation or manage associated conditions like multiple sclerosis.
- Stay Informed: Advances in medical research may lead to new treatments or changes in management strategies. Staying informed about the latest research can empower you to make informed decisions about your health care.
By adopting these lifestyle adjustments, utilizing support systems, and focusing on long-term management, individuals with optic neuritis can lead fulfilling lives despite the challenges posed by their condition.
FAQs about Optic Neuritis Symptoms
What is optic neuritis?
Optic neuritis is an inflammation of the optic nerve, which transmits visual information from the eye to the brain. This condition can cause a range of visual disturbances.
What are the common symptoms of optic neuritis?
The most common symptom of optic neuritis is sudden vision loss, which is often partial but can be complete. Other symptoms include pain during eye movement, blurred vision, and seeing flashing lights. Colors might also appear faded or washed out.
How quickly do symptoms of optic neuritis develop?
Symptoms of optic neuritis typically develop rapidly over a few hours or days. Most patients experience a peak in symptoms within one week from onset.
Can symptoms of optic neuritis improve on their own?
Yes, the symptoms of optic neuritis often improve without treatment within a few weeks. However, some people might experience lingering effects like reduced color vision or contrast sensitivity.
When should someone seek medical attention for optic neuritis symptoms?
Immediate medical attention should be sought if you experience sudden changes in vision, especially if accompanied by pain when moving the eyes. Early diagnosis and treatment are crucial for managing the condition and preventing potential complications.
Are there any long-term effects of optic neuritis?
While many recover completely, some individuals may have residual visual deficits. The long-term effects can vary, including persistent problems with color vision, contrast sensitivity, or sharpness of vision.
Can optic neuritis be a sign of another condition?
Yes, optic neuritis can be associated with multiple sclerosis (MS) and other autoimmune disorders. It may be an initial sign of these conditions in some patients.
Conclusion
In summary, optic neuritis presents with symptoms such as blurred vision, pain with eye movement, and sometimes, a loss of color vision. These symptoms are typically triggered by underlying causes, including autoimmune disorders like multiple sclerosis, infections, and other inflammatory conditions. Understanding these symptoms and their potential triggers is crucial.
The importance of early diagnosis and comprehensive treatment for optic neuritis cannot be overstated. Early medical intervention can significantly improve the prognosis and manage the underlying causes effectively. Treatment often involves corticosteroids to reduce inflammation and, when appropriate, addressing specific underlying conditions.
If you experience any symptoms of optic neuritis, it is imperative to seek professional medical advice promptly. Consulting an eye specialist or neurologist can lead to early diagnosis and appropriate management, enhancing recovery prospects and overall health. Remember, timely action can make a significant difference in the outcome of optic neuritis treatment.
References
For further reading and to validate the information on optic neuritis symptoms, consider exploring these reputable sources:
- Mayo Clinic – Provides a detailed overview of symptoms, causes, and treatment options for optic neuritis. Access the full article here.
- National Multiple Sclerosis Society – Offers comprehensive resources on optic neuritis as it relates to multiple sclerosis, including symptom management and long-term care. Read more here.
- Healthline – Features an article that breaks down optic neuritis symptoms, diagnostic methods, and treatment strategies, written by medical professionals. Visit the page here.
- American Academy of Ophthalmology – Contains peer-reviewed medical articles on optic neuritis, its implications, and advanced treatment techniques. Explore the subject here.
These sources provide credible and in-depth information that can help deepen your understanding of optic neuritis and its implications on health.