Neuroendocrine Tumors Symptoms: Neuroendocrine tumors (NETs) are a complex and diverse group of tumors that arise from neuroendocrine cells, which are specialized cells that produce hormones and release them into the bloodstream in response to neural signals.
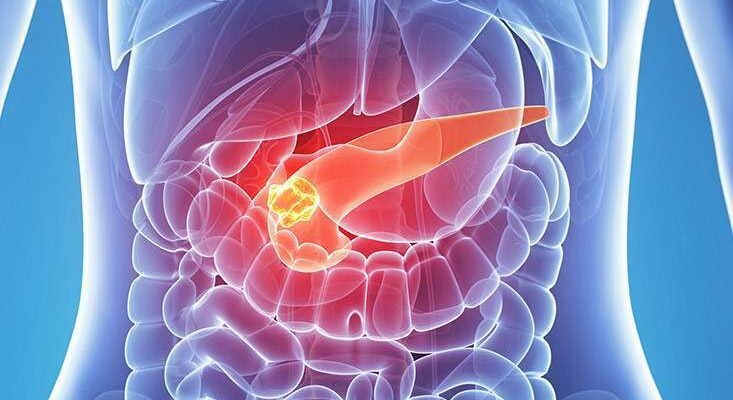
These tumors can occur throughout the body but are most commonly found in the gastrointestinal tract, pancreas, and lungs.
Understanding the symptoms and causes of neuroendocrine tumors is crucial for early diagnosis and effective treatment.
What are Neuroendocrine Tumors?
Neuroendocrine tumors (NETs) are a diverse group of malignancies that originate from neuroendocrine cells. These cells are unique because they possess characteristics of both nerve cells and hormone-producing endocrine cells. NETs can therefore produce hormones, and their behavior ranges from benign to highly malignant. They are relatively rare and can develop in various parts of the body. The symptoms of NETs often vary widely, depending on the location of the tumor and the type of hormones it produces, making them challenging to diagnose early.
Types of Neuroendocrine Tumors
There are several types of neuroendocrine tumors, each classified based on the origin of the cells. Some of the primary types include:
- Carcinoid Tumors: Typically found in the gastrointestinal tract, lungs, or thymus, these tumors are generally slow-growing.
- Pancreatic Neuroendocrine Tumors (PNETs): These arise from the islet cells of the pancreas and can vary widely in their behavior.
- Pheochromocytomas: Originating from the adrenal glands, these tumors primarily affect hormone production that controls blood pressure and heart rate.
- Merkel Cell Carcinoma: A rare and aggressive form of skin cancer that begins in neuroendocrine cells of the skin.
- Medullary Thyroid Carcinoma: This type develops from the C cells in the thyroid, which produce calcitonin, a hormone that regulates calcium levels in the blood.
Common Locations of Neuroendocrine Tumors in the Body
Neuroendocrine tumors can develop in various locations throughout the body, but some sites are more common than others:
- Gastrointestinal Tract: This is the most common site for NETs, particularly the small intestine, rectum, and stomach.
- Pancreas: Pancreatic neuroendocrine tumors are among the most clinically significant, given their potential to affect hormone levels profoundly.
- Lungs: NETs can develop in the lungs, where they are often mistaken for other types of lung cancer.
- Thyroid: Medullary thyroid carcinoma is a specific type of NET that affects the thyroid gland.
- Adrenal Glands: Pheochromocytomas occur in the adrenal glands and significantly impact the body’s stress response mechanisms.
However, understanding the types and locations of neuroendocrine tumors is crucial for early diagnosis and effective treatment, as symptoms can vary and often mimic those of other conditions.
Symptoms of Neuroendocrine Tumors
Understanding the symptoms is crucial for early diagnosis and effective management.
General Symptoms Associated with Neuroendocrine Tumors
NETs often present with nonspecific symptoms that can be easily mistaken for other common conditions, which makes them particularly challenging to diagnose early. General symptoms include:
- Fatigue: A pervasive sense of tiredness that does not improve with rest.
- Weight loss: Unintended and unexplained loss of weight.
- Fever: Occasional low-grade fevers that seem to have no apparent cause.
- Skin flushing: Reddening of the face and neck, often accompanied by a warm feeling.
- Sweating: Increased perspiration, especially at night.
- Palpitations: Irregular or fast heartbeats.
Specific Symptoms Based on Tumor Location
The symptoms of NETs can vary significantly depending on the organ affected. Some of the common locations and associated symptoms include:
- Gastrointestinal tract: Abdominal pain, nausea, vomiting, diarrhea, and gastrointestinal bleeding.
- Lungs: Difficulty breathing, wheezing, or a persistent cough that may be mistaken for asthma.
- Pancreas: Symptoms of diabetes such as increased thirst, urination, and unexplained weight loss.
- Liver (from metastasis or primary): Jaundice (yellowing of the skin and eyes), abdominal swelling, and pain.
Symptoms of Metastatic Neuroendocrine Tumors
When NETs metastasize, or spread to other parts of the body, they can present additional symptoms based on the new location of the tumor. Common symptoms of metastatic NETs include:
- Bone pain: If the tumor spreads to the bones, it can cause persistent pain and fragility.
- Neurological symptoms: Metastases to the brain can lead to headaches, visual disturbances, or seizures.
- Hormonal imbalances: Overproduction of hormones can lead to various syndromes, depending on the hormones involved.
- Liver enlargement: Enlarged liver due to metastasis can lead to a feeling of fullness, abdominal pain, and increased abdominal girth.
Recognizing these symptoms and consulting with a healthcare provider can lead to earlier detection and a more effective treatment strategy for neuroendocrine tumors.
Causes and Risk Factors of Neuroendocrine Tumors
Understanding the causes and risk factors of NETs is crucial for early detection and effective management. This section will explore the genetic factors, environmental and lifestyle risk factors, and both rare and common conditions that contribute to the development of neuroendocrine tumors.
Genetic Factors Contributing to NETs
Several genetic mutations and hereditary syndromes significantly increase the risk of developing neuroendocrine tumors:
- Multiple Endocrine Neoplasia Type 1 (MEN1) – This inherited condition typically involves tumors in the parathyroid glands, the pancreas, and the pituitary gland.
- Multiple Endocrine Neoplasia Type 2 (MEN2) – This syndrome is associated with medullary thyroid cancer and can also involve tumors in the adrenal glands (pheochromocytomas).
- Von Hippel-Lindau Syndrome (VHL) – Patients with VHL may develop NETs, particularly pheochromocytomas and neuroendocrine tumors of the pancreas.
- Neurofibromatosis Type 1 (NF1) – Commonly associated with neuroendocrine tumors, including those of the pancreas and adrenal gland.
- Tuberous Sclerosis Complex (TSC) – This condition can lead to the development of NETs in various organs.
Genetic counseling and testing are advised for individuals with a family history of these conditions to assess their risk of neuroendocrine tumors.
Environmental and Lifestyle Risk Factors
Environmental exposures and lifestyle choices can also play a role in the development of neuroendocrine tumors:
- Smoking – Tobacco use has been linked to an increased risk of developing certain types of neuroendocrine tumors, such as those in the lungs.
- Diet and Obesity – High-fat diets and obesity may influence the risk of NETs, particularly those in the gastrointestinal tract.
- Occupational Exposure – Exposure to certain chemicals and toxins, especially in industrial settings, has been associated with a higher risk of developing NETs.
Promoting a healthy lifestyle and minimizing exposure to harmful substances can help reduce the risk of neuroendocrine tumors.
Discussing Rare and Common Conditions Leading to NETs
Neuroendocrine tumors can also arise from both rare and more commonly encountered medical conditions:
- Chronic Gastritis – Ongoing inflammation of the stomach lining, particularly due to Helicobacter pylori infection, can lead to the development of gastric NETs.
- Zollinger-Ellison Syndrome – This rare condition involves the formation of gastrin-secreting tumors (gastrinomas) in the pancreas and duodenum, increasing the risk of pancreatic NETs.
- Insulinomas and Glucagonomas – These are pancreatic NETs that secrete insulin and glucagon, respectively, and are relatively rare.
By understanding the genetic, environmental, and medical conditions associated with neuroendocrine tumors, individuals can better manage their health risks and seek appropriate medical attention for early diagnosis and treatment.
Diagnosing Neuroendocrine Tumors (NETs)
Early diagnosis is crucial as it significantly impacts the effectiveness of treatment and improves patient outcomes. Here, we explore the common diagnostic tests and procedures, the challenges faced in diagnosing NETs, and the importance of early detection.
Common Diagnostic Tests and Procedures for NETs
1. Blood and Urine Tests: These can detect abnormal levels of hormones and other substances that NETs often produce, such as chromogranin A (CgA) and 5-HIAA (a breakdown product of serotonin).
2. Imaging Tests:
- CT Scan (Computed Tomography): Provides detailed cross-sectional images of the body and can help identify the location and size of neuroendocrine tumors.
- MRI (Magnetic Resonance Imaging): Used for its superior contrast resolution to visualize NETs, especially in the liver and pancreas.
- Octreoscan: A type of scintigraphy that involves injecting a radio-labeled somatostatin analogue, which binds to somatostatin receptors on NET cells, making them visible on a gamma camera.
- PET Scan (Positron Emission Tomography): Often combined with a CT scan (PET/CT), this test can detect the metabolic activity of cells, which is useful for staging and monitoring treatment response.
3. Endoscopic Procedures:
- Bronchoscopy, Gastroscopy, and Colonoscopy: Allow direct visualization and biopsy of tumors within the lungs, stomach, and colon, respectively.
- Endoscopic Ultrasound (EUS): Uses ultrasound along with an endoscope to get detailed images of the digestive tract and surrounding organs, often used to assess the pancreas.
4. Biopsy: The removal of a small amount of tissue for examination under a microscope. This is the definitive method for diagnosing the type and grade of NETs.
Challenges in Diagnosing Neuroendocrine Tumors
- Non-specific Symptoms: Many NETs produce symptoms that are vague and common to other less serious conditions, such as abdominal pain, flushing, and diarrhea, leading to frequent misdiagnosis.
- Variable Tumor Behavior: NETs can be very slow-growing or aggressively malignant, which affects how they manifest in the body and respond to typical diagnostic tests.
- Heterogeneity of Tumors: NETs vary greatly depending on their origin and the type of neuroendocrine cells involved, requiring different diagnostic strategies and expertise.
- Limited Availability of Specialized Tests: Some diagnostic tests, like advanced imaging scans or specific hormonal assays, are not widely available in all healthcare settings.
Importance of Early Diagnosis in Treatment Outcomes
- Better Prognosis: Early-stage neuroendocrine tumors are generally more treatable and have a higher chance of successful management with surgery or targeted therapies.
- Prevention of Metastasis: Detecting and treating NETs before they spread can prevent complications and the need for more extensive treatments.
- Improved Quality of Life: Early diagnosis and treatment can alleviate the symptoms caused by hormone overproduction, significantly improving quality of life.
However, ongoing research and improved diagnostic techniques continue to enhance our ability to identify NETs at an earlier stage.
Treatment Options for Neuroendocrine Tumors
Treatment options are chosen based on the type, location, and stage of the tumor, as well as the patient’s overall health. Here, we explore the established treatment modalities and recent innovations in the treatment of neuroendocrine tumors.
List of Treatment Modalities
- Surgery: Surgery is often the primary treatment for neuroendocrine tumors, especially if the cancer is localized. It involves removing the tumor and possibly some surrounding tissue. In cases where the tumor has spread, surgery may still be performed to remove as much of the tumor mass as possible, a process known as debulking.
- Medication: Medicinal treatments include somatostatin analogs (SSAs) like octreotide or lanreotide, which help control symptoms and may slow tumor growth. Targeted therapies, such as everolimus and sunitinib, specifically attack cancer cells with less damage to normal cells compared to chemotherapy.
- Chemotherapy: This treatment uses drugs to kill cancer cells and is typically used for fast-growing neuroendocrine tumors. Chemotherapy might be combined with other treatment options to improve outcomes.
- Radiation Therapy: Radiation therapy uses high-energy rays to target and kill cancer cells. For neuroendocrine tumors, peptide receptor radionuclide therapy (PRRT) is a specific type of radiation therapy that delivers radioactive material directly to the tumor cells via a peptide.
- Interventional Radiology: Techniques such as radiofrequency ablation (RFA) and transarterial chemoembolization (TACE) are used to directly target tumors, often when surgery is not an option.
- Hormonal Therapy: This involves using hormones to slow the growth of certain types of neuroendocrine tumors. Hormonal therapy can be effective in managing symptoms and controlling tumor progression.
Innovations in Treatment Approaches
- Immunotherapy: Emerging as a promising approach, immunotherapy enhances the body’s immune system to fight cancer. Trials are currently underway to evaluate the effectiveness of immunotherapy in treating neuroendocrine tumors.
- Molecular Targeted Therapies: New drugs that target specific molecular pathways involved in tumor growth are being developed. These include inhibitors of angiogenesis, growth factor receptors, and the mTOR pathway, offering a more personalized treatment approach.
- Genomic Profiling: Advances in genomic profiling are allowing for more personalized treatment plans. By understanding the specific genetic alterations in a tumor, treatments can be tailored to target those changes specifically.
- Nanoparticle Therapy: Research is ongoing into the use of nanoparticles to deliver chemotherapy directly to cancer cells, potentially reducing side effects and improving treatment efficacy.
- Radioembolization: This is a newer form of treatment that combines radiation therapy with embolization. It involves injecting tiny radioactive beads into the arteries that feed the tumor, blocking the blood supply and delivering radiation directly to the cancer cells.
However, these treatment options and innovations represent the forefront of a rapidly evolving field. As research continues, these approaches are refined to improve outcomes and quality of life for patients with neuroendocrine tumors.
Living with Neuroendocrine Tumors
Living with neuroendocrine tumors can present unique challenges, impacting a patient’s quality of life in various ways. However, effective management strategies and robust support systems can help mitigate these challenges, allowing individuals to lead fulfilling lives.
Impact on Quality of Life
Neuroendocrine tumors can significantly affect a patient’s quality of life, manifesting through both physical and emotional symptoms. Common impacts include:
- Fatigue and Weakness: Many patients experience chronic fatigue, which can hinder daily activities and reduce overall energy levels.
- Pain and Discomfort: Depending on the tumor’s location, pain can be a persistent issue, affecting mobility and comfort.
- Hormonal Imbalances: Since NETs can produce hormones, they often cause hormonal imbalances that lead to symptoms like flushing, diarrhea, and heart palpitations.
- Emotional and Psychological Distress: The stress of living with a chronic illness can lead to depression, anxiety, and feelings of isolation.
Management Strategies for Symptoms
Managing the symptoms of neuroendocrine tumors involves a combination of medical treatment and lifestyle adjustments. Key strategies include:
- Medication: Pharmaceutical treatments, such as somatostatin analogs, can help control hormone-related symptoms and tumor growth.
- Surgery and Procedures: When feasible, surgical removal of the tumor or localized treatments like radiofrequency ablation can alleviate symptoms and improve prognosis.
- Diet and Nutrition: Tailoring diet to manage gastrointestinal symptoms and nutritional deficiencies can play a crucial role in overall well-being.
- Physical Activity: Regular, moderate exercise can combat fatigue, bolster mental health, and enhance physical functioning.
Support Systems and Resources for Patients
A strong support network is crucial for managing life with neuroendocrine tumors. Useful resources include:
- Support Groups: Connecting with others facing similar challenges can provide emotional support, practical tips, and a sense of community.
- Professional Counseling: Mental health professionals can help patients cope with the emotional and psychological impacts of their diagnosis.
- Educational Resources: Organizations such as the Neuroendocrine Tumor Research Foundation provide information and updates on treatment options, research developments, and patient education.
- Specialist Care: Engaging with healthcare providers who specialize in neuroendocrine tumors ensures that patients receive informed, tailored medical advice and care.
However, living with neuroendocrine tumors is undoubtedly challenging, but with the right strategies and support, patients can manage their symptoms and maintain a good quality of life.
FAQs about Neuroendocrine Tumor Symptoms
What are the common symptoms of neuroendocrine tumors?
Neuroendocrine tumors (NETs) often manifest subtly and can vary greatly depending on the tumor’s location in the body. Common symptoms include persistent pain in a specific area, noticeable changes in bowel or urinary habits, unexplained weight loss, fatigue, and skin flushing. These symptoms typically arise from the excess hormones that NETs produce.
Can neuroendocrine tumors cause symptoms that mimic other conditions?
Yes, symptoms of neuroendocrine tumors can closely resemble those of other more common conditions. For instance, symptoms like stomach ulcers, asthma, or diabetes can overlap with those of NETs due to hormonal imbalances caused by the tumors. This similarity can often lead to misdiagnosis or delays in the correct diagnosis.
Are there any early warning signs of neuroendocrine tumors?
Early warning signs of neuroendocrine tumors can be non-specific and vary widely, which makes them easy to overlook. Subtle signs might include intermittent flushing of the skin, diarrhea, or heart palpitations, especially if these symptoms seem disproportionate to any clear cause or are persistent.
How do symptoms vary with different types of neuroendocrine tumors?
The symptoms of neuroendocrine tumors depend significantly on the tumor’s location. For example, insulinomas in the pancreas can lead to low blood sugar symptoms, whereas carcinoid tumors often result in flushing and diarrhea. Understanding the specific type and location of the tumor is crucial for identifying the related symptoms.
When should someone consult a doctor about neuroendocrine tumor symptoms?
It is advisable to consult a healthcare provider if you experience any unusual or persistent symptoms, especially if they do not respond to standard treatments or are accompanied by significant changes in health like unexpected weight loss or a drastic change in bowel habits. Early consultation and screening can lead to timely diagnosis and better management of the condition.
Conclusion
In summary, neuroendocrine tumors (NETs) present with a diverse range of symptoms that can often be elusive and mimic those of more common diseases, such as abdominal pain, weight changes, and hormonal fluctuations.
The causes of NETs are generally not well-understood, but genetic factors and family history can play a significant role in some individuals. Early recognition and diagnosis are crucial for effective management and treatment. If you notice any persistent, unusual symptoms, it is essential to consult with healthcare providers.
They can offer appropriate diagnostic evaluations and treatment options tailored to individual needs. Prioritizing your health by seeking professional advice is key in managing any potential risks associated with neuroendocrine tumors.
References
For further reading and to validate the information provided on neuroendocrine tumor symptoms, consider exploring the following reputable sources. These resources offer comprehensive insights and are recognized for their accuracy in medical reporting.
- National Cancer Institute: The NCI provides detailed information on the types, symptoms, and treatments of neuroendocrine tumors. Access their resource page here.
- Mayo Clinic: A leading healthcare organization, Mayo Clinic offers an extensive overview of neuroendocrine tumors, including symptoms, causes, and diagnostic procedures. Visit their detailed guide here.
- The New England Journal of Medicine: For peer-reviewed articles and latest research findings on neuroendocrine tumors, check out NEJM’s collection here.
- American Cancer Society: This resource provides comprehensive information on the diagnosis, treatment, and management of neuroendocrine tumors. Read more at American Cancer Society’s website.
- PubMed Central: For research articles and studies on neuroendocrine tumors, PubMed Central is an invaluable resource. You can explore their library of free articles here.
By consulting these sources, you can deepen your understanding of neuroendocrine tumors and stay updated with the latest research in the field.