Myofascial Pain Syndrome Symptoms: Myofascial Pain Syndrome (MPS) is a chronic pain disorder marked by sensitivity in the myofascial tissues.
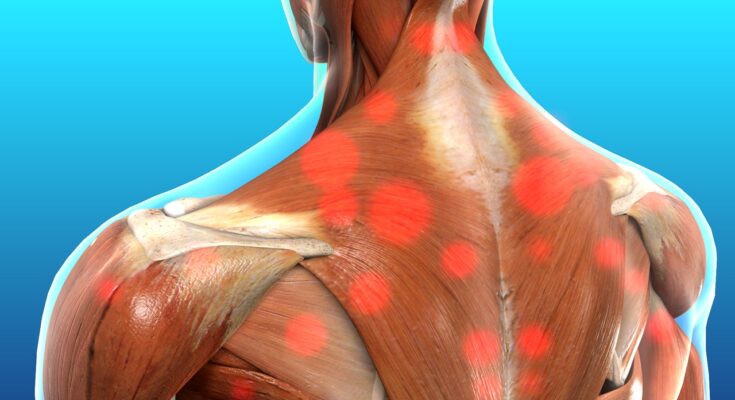
These tissues surround and support the muscles throughout your body. The pain usually originates from specific points within your myofascial tissues called “trigger points.”
What is Myofascial Pain Syndrome?
Myofascial Pain Syndrome (MPS) is a chronic pain disorder marked by sensitivity in the myofascial tissues—these are the tough membranes that wrap, connect, and support your muscles. The primary indicator of MPS is the presence of localized trigger points, small, tight knots that form in muscles and cause intense pain, often referred to as referred pain because it can spread to seemingly unrelated parts of the body.
How Myofascial Pain Syndrome Differs from Other Types of Pain
- Localized versus Widespread Pain: Unlike fibromyalgia, which causes widespread body pain, MPS pain is localized to specific areas linked to the knotted trigger points within the muscles.
- Trigger Points: MPS is characterized by palpable trigger points that elicit pain upon compression, which are not typically seen in other pain syndromes like nerve pain disorders or joint pain from arthritis.
- Pain Nature: The pain associated with MPS is described as a deep, aching pain within the muscle, along with sensations such as stiffness and tenderness, differentiating it from the sharp or burning pain sensations often experienced with neuropathic pain conditions.
- Pain Patterns: MPS pain can be associated with specific activities or mechanical stress, whereas other chronic pain conditions such as neuropathic pain may be constant and less related to movement.
- Treatment Approaches: Treatment for MPS often involves physical therapy, massage, and trigger point injections, which are specifically targeted at relaxing the trigger points. This is distinct from other pain management strategies that might focus more on medication, surgery, or electrical stimulation therapies.
However, understanding the distinct features of Myofascial Pain Syndrome helps in accurately diagnosing and effectively treating it, distinguishing it from other types of chronic pain disorders.
Symptoms of Myofascial Pain Syndrome
Understanding these symptoms is crucial for diagnosis and management. Here’s a detailed list of the common symptoms associated with MPS:
1. Localized Muscle Pain
MPS typically causes deep, aching muscle pain that persists or worsens over time. This pain is localized to specific areas known as trigger points.
2. Trigger Points
Trigger points are sensitive spots in the muscle or fascial tissue. When pressed, these points can produce pain and twitching in the muscle.
3. Referred Pain
This condition is known for causing referred pain, which means pain is felt in areas of the body other than where the trigger point is located. For instance, a trigger point in the back might cause pain in the shoulder.
4. Limited Range of Motion
The stiffness in the muscles associated with MPS can lead to a decreased range of motion. This might make it difficult to perform everyday tasks that involve moving the affected muscle group.
5. Muscle Fatigue
Individuals with MPS may experience a notable increase in muscle fatigue. Even minimal physical activity can lead to feelings of exhaustion in the muscle.
6. Muscle Tension
MPS can cause muscles to tense up, which can be felt as hard knots within the muscle. These are often palpable on physical examination.
7. Sleep Disturbances
The discomfort and pain caused by MPS can interfere with sleep, leading to a cycle of pain and fatigue that can exacerbate other symptoms.
Case Studies Illustrating Symptoms of MPS
Case Study 1: Office Worker with Shoulder Pain
A 45-year-old office worker complained of persistent shoulder pain, initially attributed to poor ergonomic setup at her workstation. Despite adjustments, her pain persisted. On examination, a physician identified multiple trigger points in her upper back and shoulders. Treatment focused on these points relieved her symptoms, confirming the diagnosis of MPS.
Case Study 2: Retired Athlete with Leg Pain
A retired athlete, aged 60, experienced ongoing leg pain which was sharp at times and dull at others. He reported that the pain worsened with physical activity and during cold weather. A detailed examination revealed several trigger points in his thighs and lower back. Targeted therapy on these trigger points significantly alleviated his pain, supporting the diagnosis of MPS.
By recognizing these symptoms and understanding how they manifest in everyday scenarios, patients and healthcare providers can better manage Myofascial Pain Syndrome, leading to improved outcomes and quality of life.
Potential Causes of Myofascial Pain Syndrome
Understanding the potential causes of MPS can help in managing symptoms and improving overall well-being. Below are the key factors that contribute to the development of this condition:
Factors Contributing to the Development of MPS
- Muscle Overuse or Injury: Repeated muscle use or sustained muscle activity can lead to MPS. This is often seen in individuals who engage in repetitive work-related activities, sports, or exercise routines that strain certain muscle groups.
- Stress and Emotional Factors: Emotional stress is a significant contributor to MPS as it can lead to increased muscle tension and trigger point formation. Stress-related muscle tension often affects the neck, shoulders, and back, leading to pain and discomfort.
- Poor Posture: Maintaining a poor posture for extended periods, such as slouching while sitting or standing improperly, can strain muscles and connective tissues, contributing to the development of trigger points and MPS.
- Lack of Exercise: Inactivity can weaken muscles and reduce flexibility, making them more susceptible to injuries and the development of myofascial pain. Regular physical activity is crucial in maintaining muscle health and preventing MPS.
- Sleep Disturbances: Inadequate or poor-quality sleep can exacerbate muscle tension and pain. Consistently good sleep helps in muscle recovery and pain management.
- Nutritional Deficiencies: Certain nutritional deficiencies, like vitamin D or magnesium, can affect muscle function and health, potentially leading to or worsening MPS.
Additional Contributing Factors
- Medical Conditions: Some medical conditions, such as fibromyalgia or arthritis, can predispose individuals to MPS due to chronic inflammation and pain.
- Age and Gender: As people age, muscle elasticity and tone tend to decrease, which can increase the risk of developing MPS. Additionally, MPS appears to be more prevalent in women, though the reasons for this are still under investigation.
By addressing issues like muscle overuse, stress management, and maintaining a healthy lifestyle, individuals can significantly reduce their risk of developing myofascial pain syndrome.
Diagnosing Myofascial Pain Syndrome
Accurately diagnosing MPS is crucial for effective treatment. Below, we explore the primary diagnostic methods used by healthcare professionals and highlight the importance of distinguishing MPS from other conditions.
Diagnostic Methods for Myofascial Pain Syndrome
- Medical History and Physical Examination: The first step in diagnosing MPS involves a detailed review of the patient’s medical history and a physical exam. Healthcare providers look for specific symptoms like chronic muscle pain, tenderness in certain areas, and the presence of trigger points.
- Manual Palpation: This technique is used to identify areas of muscle stiffness and trigger points. During palpation, the healthcare provider applies gentle pressure to the muscles to assess pain responses and feel for tense muscle fibers or knots.
- Imaging Tests: While imaging tests like MRI or ultrasound are not typically used to diagnose MPS alone, they can help rule out other conditions that may mimic its symptoms, such as fibromyalgia or neurological disorders.
- Trigger Point Injections: Sometimes, a diagnostic anesthetic injection into a trigger point can help confirm MPS. If the injection relieves pain, it supports the diagnosis of MPS.
- Rule-Out Tests: These tests are essential to eliminate the possibility of other diseases. Blood tests, X-rays, and additional scans might be conducted to rule out rheumatologic diseases, infections, or other muscular disorders.
Importance of Accurate Diagnosis
Distinguishing MPS from other conditions is critical for several reasons:
- Targeted Treatment: Accurate diagnosis ensures that patients receive the most appropriate and effective treatments. MPS, for example, may be treated with physical therapy, medications, and trigger point injections, which might not be suitable for other conditions.
- Prevention of Mismanagement: Without a proper diagnosis, patients might undergo unnecessary procedures or therapies that can lead to increased discomfort or complications.
- Understanding and Managing Symptoms: Knowing that the pain is due to MPS helps patients and healthcare providers better understand the pain triggers and manage them effectively.
- Avoiding Chronic Conditions: Early and accurate diagnosis can prevent the condition from worsening or becoming chronic, leading to prolonged discomfort and disability.
However, diagnosing Myofascial Pain Syndrome requires a comprehensive approach that includes a thorough medical examination and specific diagnostic tests.
Impact of Myofascial Pain Syndrome on Daily Life
Below, we explore the various ways in which MPS can impact daily routines and hear from individuals who live with the condition, sharing their personal experiences.
How MPS Affects Everyday Activities
- Chronic Pain and Stiffness: Individuals with MPS experience persistent pain and muscle stiffness, which can hinder basic daily activities such as walking, bending, and lifting objects. This constant discomfort can severely limit one’s mobility and independence.
- Fatigue: The chronic pain associated with MPS often leads to significant fatigue. This exhaustion can impair a person’s ability to stay active and participate fully in work or social activities, contributing to a reduced engagement in life’s pleasures.
- Sleep Disturbances: MPS is known to disrupt sleep due to pain and discomfort, leading to difficulties in falling asleep or staying asleep. Poor sleep quality can exacerbate daytime fatigue, affecting cognitive functions like memory and concentration.
- Mood Changes: Living with chronic pain can also lead to emotional and psychological effects, including anxiety, depression, and irritability. These mood changes can strain personal relationships and decrease overall life satisfaction.
- Reduced Work Capacity: Many individuals with MPS find it challenging to maintain regular employment due to their symptoms. The inability to perform physically demanding tasks or even sit for extended periods can lead to reduced earning capacity and financial strain.
Personal Stories from Those Living with MPS
- John’s Story: “Every morning, I wake up feeling like I haven’t slept at all. The pain and stiffness in my back make it hard to get out of bed, much less think about going to work or playing with my kids. It feels like I’m always planning my life around my pain.”
- Maria’s Experience: “Living with MPS has been a constant battle with pain. It affects not just my physical health but my mental well-being too. There are days when the pain is manageable, but on bad days, it feels like a dark cloud is hanging over everything I do.”
- Quote from Emily: “The hardest part of living with MPS is the unpredictability. Some days I feel okay, and other days it’s unbearable. It’s frustrating not knowing how I’ll feel when I wake up each morning.”
However, these stories and experiences highlight the profound impact MPS can have on daily life, from managing chronic pain and emotional struggles to navigating the complexities of personal and professional life.
Management and Treatment Options for Myofascial Pain Syndrome
Managing and treating this condition effectively requires a comprehensive approach that incorporates various strategies. Here, we explore the current treatment options for MPS, including physical therapy, medications, and alternative treatments.
Current Treatment Strategies for Myofascial Pain Syndrome
Physical Therapy and Massage: Physical therapy is one of the cornerstone treatments for MPS. It involves various techniques, such as stretching exercises and postural training, which help alleviate muscle tightness and pain. Massage therapy, particularly trigger point massage, is also highly effective. It focuses on specific areas of muscle tightness, helping to release tension and reduce pain.
Medications and Pain Relief Techniques: Pain management in MPS often includes the use of medications. Over-the-counter pain relievers like ibuprofen and acetaminophen are commonly prescribed to reduce inflammation and pain. In more severe cases, doctors may prescribe muscle relaxants or even low-dose antidepressants, which have been found to be effective in managing chronic pain. Local anesthetic injections directly into the trigger points are another option for immediate pain relief.
Alternative Treatments and Lifestyle Changes: In addition to conventional treatments, many patients find relief through alternative methods. Acupuncture and dry needling can help by targeting trigger points to relieve muscle pain and stiffness. Lifestyle changes, such as improving sleep patterns and diet, incorporating regular physical activity, and learning stress management techniques, also play a crucial role in managing MPS symptoms.
However, consulting with healthcare providers who specialize in pain management and physical therapy will help tailor a treatment plan that best fits the needs of each patient.
Prevention Tips for Myofascial Pain Syndrome (MPS)
Preventing the onset of Myofascial Pain Syndrome (MPS) involves adopting healthy lifestyle practices that focus on maintaining good muscle health and reducing the risk of muscle strain or injury. Here are practical tips and the significance of incorporating ergonomic practices and regular physical activity into your daily routine to help prevent MPS.
Practical Advice on Preventing the Onset of MPS Symptoms
- Maintain Good Posture: Keeping your body properly aligned can prevent unnecessary strain on your muscles and fascia. Make a conscious effort to sit, stand, and move with proper posture.
- Regular Stretching and Flexibility Exercises: Incorporate stretching into your daily routine. Focus on stretches that enhance flexibility and improve range of motion, which can help reduce the tension in your muscles.
- Strengthening Exercises: Build muscle strength, particularly in areas prone to MPS, such as the neck, shoulders, and back. Strong muscles are less susceptible to injury and strain.
- Use Correct Techniques: Whether exercising or engaging in daily activities, using the correct techniques can prevent muscle overuse and repetitive strain injuries, common triggers for MPS.
- Manage Stress: High stress levels can contribute to muscle tension. Techniques such as yoga, meditation, and deep-breathing exercises can help manage stress and reduce muscle tightness.
- Adequate Hydration: Staying hydrated helps maintain the health of the fascia and muscles. Ensure you drink plenty of water throughout the day.
- Proper Nutrition: A balanced diet rich in anti-inflammatory foods can support muscle and fascia health. Include foods high in magnesium and potassium to help muscle function.
Importance of Ergonomic Practices and Regular Physical Activity
- Ergonomic Practices: Implementing ergonomic solutions in your workspace can significantly reduce the risk of developing MPS. Use chairs, desks, and computer setups that support a natural posture. If your job involves repetitive motions, make sure to take frequent breaks and use tools that minimize strain.
- Regular Physical Activity: Engaging in regular physical activity is crucial for maintaining muscle health and flexibility. Activities like walking, swimming, or cycling promote good circulation, which is essential for muscle and fascial health. Regular exercise also helps in maintaining a healthy weight, which reduces the burden on your musculoskeletal system.
Awareness of your body’s posture, movement patterns, and the environment in which you work and live will play a crucial role in preventing MPS symptoms. By focusing on good ergonomics and regular physical activity, you can maintain muscle health and improve your overall well-being.
FAQs about Myofascial Pain Syndrome Symptoms
1. What are the primary symptoms of Myofascial Pain Syndrome?
Myofascial Pain Syndrome (MPS) primarily manifests as persistent, deep muscle pain. Key symptoms include localized muscle tenderness, knots in the muscles known as trigger points, and pain that persists or worsens. These trigger points may also cause referred pain, meaning pain in areas of the body that are not the direct site of the trigger point.
2. How does referred pain from MPS present itself?
Referred pain from MPS can be misleading as it may occur in areas distant from the actual trigger points. For example, a trigger point in the back might cause pain in the shoulder. This pain is typically steady, aching, and can vary in intensity based on activity or stress.
3. Are there any visible signs of Myofascial Pain Syndrome?
Visible signs of MPS are not common, but you might notice muscle knots or taut bands of muscle fibers. These can be felt under the skin as small lumps or bumps. Occasionally, the affected muscle might appear swollen or taut due to prolonged tension.
4. Does Myofascial Pain Syndrome cause fatigue?
Yes, individuals with MPS often experience fatigue, especially if pain disrupts their sleep. The chronic nature of the pain can also lead to increased emotional and physical stress, contributing further to feelings of tiredness and exhaustion.
5. Can MPS symptoms be intermittent, or are they always constant?
MPS symptoms can vary; they may be constant or intermittent. Factors like physical activity, stress, poor posture, or lack of movement can influence the intensity and presence of symptoms. Managing these factors can help reduce symptom episodes.
Conclusion
In summary, Myofascial Pain Syndrome (MPS) manifests through symptoms like deep, aching muscle pains, persistent knots, and sensitive trigger points that can cause referred pain. These symptoms not only disrupt daily activities but can also significantly reduce the quality of life. If you’re experiencing any of these discomforts, it’s essential not to ignore them.
We highly encourage anyone who suspects they might be dealing with MPS to seek professional medical advice. A healthcare provider can offer a proper diagnosis and tailor a treatment plan that addresses the specific needs of your condition. Remember, early intervention is key to managing symptoms effectively and preventing further complications. Don’t hesitate to consult a professional and take a step towards better health and well-being.
References
For those interested in deepening their understanding of Myofascial Pain Syndrome (MPS) and its symptoms, the following reputable sources offer detailed insights and validation of the information discussed:
American Academy of Family Physicians: Provides comprehensive articles on the diagnosis and management of MPS. Visit AAFP for more details
Mayo Clinic: Offers an extensive overview of symptoms, causes, and treatment options for Myofascial Pain Syndrome. Explore MPS information at Mayo Clinic
National Institutes of Health (NIH): Features research publications and clinical trials related to MPS, highlighting the latest advancements in treatment. Read more at NIH
PubMed Central: An invaluable resource for accessing scientific studies and review articles on MPS.
Access studies on PubMed Central
WebMD: Provides a user-friendly guide on the symptoms and management of Myofascial Pain Syndrome.
Learn about MPS on WebMD
These sources are esteemed for their reliability and depth of information. They serve as excellent starting points for both general readers and healthcare professionals seeking to verify details and expand their knowledge on Myofascial Pain Syndrome.