Myofascial Pain Syndrome Treatment: Myofascial Pain Syndrome (MPS) is a chronic pain disorder that affects the musculoskeletal system, particularly the fascia—the connective tissue that surrounds muscles.
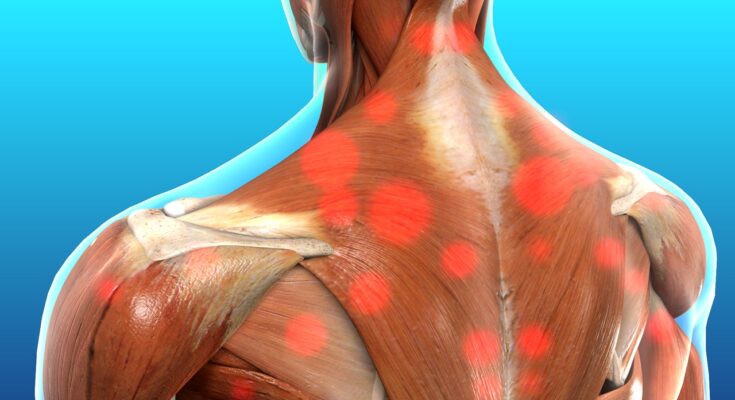
It is characterized by the presence of trigger points or sensitive spots in tight muscle fibers which can cause pain locally and in a referred pattern.
Understanding MPS is crucial for developing effective treatment strategies and improving patient outcomes.
Understanding Myofascial Pain Syndrome
Myofascial Pain Syndrome (MPS) is a chronic condition that affects the musculoskeletal system, characterized by pain that originates from myofascial trigger points in skeletal muscle. Understanding the characteristics and epidemiology of MPS can help in better diagnosis and treatment.
Characteristics of Myofascial Pain Syndrome
- Trigger Points: MPS is primarily associated with discrete, focal, hyper-irritable spots located in a taut band of skeletal muscles. These trigger points can produce local and referred pain when stimulated.
- Referred Pain: One of the hallmark features of MPS is the pain that typically radiates from the trigger point to other areas of the body. This referred pain can complicate diagnosis, as it may not be immediately apparent that the trigger point is the source of pain.
- Muscle Stiffness and Tenderness: Affected muscles may feel tight, and tender spots can develop at the trigger points, making it painful to touch or move the affected areas.
- Autonomic Phenomena: In some cases, stimulation of trigger points can lead to autonomic phenomena such as sweating, tearing of the eyes, or goosebumps.
- Limited Range of Motion: Individuals with MPS may experience a decreased range of motion in the affected muscles due to stiffness and pain.
- Fatigue and Sleep Disturbances: Chronic pain associated with MPS can lead to fatigue and significant disruptions in sleep patterns, further impacting an individual’s quality of life.
Epidemiology: Who is Most Affected?
Myofascial Pain Syndrome can affect individuals of any age, but there are certain populations who are more frequently diagnosed:
- Age Group: It is most commonly seen in individuals between the ages of 30 and 50 years.
- Gender: Women are more likely to develop MPS than men, although the reasons for this gender disparity are not fully understood.
- Occupational Risk: People engaged in jobs that require repetitive motion or sustained muscle use are at a higher risk. This includes occupations like construction workers, musicians, and office workers who use computers extensively.
- Stress and Lifestyle Factors: High levels of stress and poor lifestyle choices, such as lack of exercise or poor posture, can also increase the risk of developing MPS.
- Previous Muscle Injury: Individuals who have had a previous muscle injury are more susceptible to developing MPS as the body attempts to compensate for the injury, potentially leading to stress on other muscles and the development of trigger points.
However, understanding these characteristics and the epidemiology of MPS can aid healthcare professionals in identifying and treating this painful condition more effectively.
Causes and Risk Factors of Myofascial Pain Syndrome
Understanding the primary causes, common risk factors, and the influence of lifestyle and occupational hazards is crucial for both prevention and management of MPS.
Primary Causes of Myofascial Pain Syndrome
- Muscle Overuse or Injury: Repetitive motions or prolonged muscle use often leads to MPS, as the muscles become stressed and strained. This is commonly seen in athletes or individuals with jobs requiring repetitive movements.
- Poor Posture: Chronic poor posture can strain muscles and fascia, particularly in the neck, back, and shoulders, leading to myofascial pain.
- Stress-Related Muscle Tension: Emotional stress can cause individuals to tighten their muscles unconsciously, which can form trigger points and lead to MPS.
Common Risk Factors and Triggers
- Age and Activity Level: Middle-aged individuals and those who are less active may be at higher risk due to decreased muscle elasticity and tone.
- Stress and Fatigue: High levels of stress and poor sleep can exacerbate muscle tension and worsen symptoms.
- Medical Conditions: Certain medical conditions such as fibromyalgia or rheumatoid arthritis can predispose individuals to developing MPS due to underlying inflammation and pain mechanisms.
The Role of Lifestyle and Occupational Hazards
- Lifestyle Choices: Sedentary lifestyle, lack of exercise, poor diet, and inadequate sleep can all contribute to the development of MPS.
- Occupational Risks: Jobs that require repetitive motion, heavy lifting, or prolonged sitting in poor ergonomic conditions are significant risk factors. Office workers, assembly line workers, and construction workers are particularly susceptible.
- Mental Health Factors: Psychological stress and poor coping mechanisms can lead to increased body tension and trigger the onset of myofascial pain.
However, regular physical activity, stress management, and proper ergonomic practices at work are essential in managing and preventing MPS.
Symptoms of Myofascial Pain Syndrome
Understanding the symptoms, their role in diagnosis, and how they differ from other similar disorders is essential for effective management and treatment.
Common Symptoms Associated with Myofascial Pain Syndrome
- Localized Muscle Pain: The hallmark of MPS is persistent, deep muscle pain that typically originates from specific areas known as trigger points.
- Trigger Points: These are sensitive spots in the muscles or fascia that, when pressed, cause pain and twitching in the affected muscle as well as referred pain in distant areas.
- Muscle Stiffness and Tenderness: Patients often experience stiffness and tenderness around the affected muscles, which can limit movement and affect posture.
- Fatigue and Sleep Disturbances: The chronic pain associated with MPS can lead to fatigue and significant disruptions in sleep patterns.
- Emotional Effects: Long-term pain can also contribute to psychological effects such as stress and depression, exacerbating the physical symptoms of the syndrome.
How Symptoms Lead to a Diagnosis of Myofascial Pain Syndrome
Diagnosing MPS primarily involves the identification of trigger points and the characteristic pattern of pain referral associated with these points. Health professionals typically perform a physical examination to:
- Locate areas of muscle stiffness and tenderness.
- Identify trigger points that produce localized and/or referred pain upon palpation.
- Evaluate the range of motion affected by muscle pain and stiffness.
Additional diagnostic tools, such as ultrasound or MRI, may be used to rule out other conditions and confirm the presence of muscular abnormalities typical of MPS.
Differences Between Myofascial Pain Syndrome and Other Musculoskeletal Disorders
While MPS shares similarities with other musculoskeletal disorders, key differences aid in its diagnosis:
- Specificity of Pain: Unlike more generalized muscle pain seen in conditions like fibromyalgia, MPS pain is more localized and linked to specific trigger points.
- Pain with Trigger Points: MPS involves distinct trigger points that cause pain directly at the site and referred pain, a feature less commonly observed in other disorders such as muscle strains or arthritis.
- Response to Treatment: MPS often responds well to treatments targeting the trigger points, such as massage therapy, dry needling, or localized injections, which may not be as effective in other musculoskeletal conditions.
However, understanding these symptoms and differences is crucial for the accurate diagnosis and effective management of Myofascial Pain Syndrome, ensuring that patients receive the most appropriate interventions for their specific condition.
Diagnostic Approaches of Myofascial Pain Syndrome
Diagnosing MPS accurately is crucial for effective treatment. Here, we explore the diagnostic processes, tools, and the roles healthcare professionals play in diagnosing this condition.
Diagnostic Process for Myofascial Pain Syndrome
- Patient History: The initial step involves a detailed discussion about the patient’s medical history, symptoms, and any prior injuries or activities that may have contributed to the pain.
- Physical Examination: A thorough physical examination is conducted to identify areas of muscle tenderness, the presence of trigger points, and any associated signs of muscle dysfunction.
- Symptom Assessment: Healthcare providers assess symptoms that typically include persistent pain, aching, and restricted movement. The pattern of pain and its specific locations help in pinpointing potential trigger points.
- Exclusion of Other Conditions: It’s essential to rule out other conditions that may mimic MPS. Conditions such as fibromyalgia, neuropathies, or infections should be considered and excluded.
- Trigger Point Identification: Special attention is given to identifying trigger points that, when pressed, reproduce the pain experienced by the patient. This is a hallmark for diagnosing MPS.
Tools and Tests Used in Diagnosing Myofascial Pain Syndrome
- Manual Palpation: The most common method used is manual palpation by a healthcare professional to locate stiff or tender muscle areas.
- Ultrasound Imaging: This tool helps in visualizing muscles, ligaments, and tendons, and can confirm the presence of abnormal muscle contractions.
- Thermography: An imaging technique that detects heat patterns on the skin’s surface, indicating underlying trigger points.
- Electromyography (EMG): Although not routinely used, EMG can help in assessing muscle health and the presence of any neuromuscular abnormalities that contribute to the pain.
The Role of Healthcare Professionals in Diagnosis
- Primary Care Physicians: Often the first contact for patients, they play a pivotal role in the initial assessment and referral to specialists if needed.
- Physical Therapists: Experts in musculoskeletal function, physical therapists specialize in identifying and managing MPS through manual techniques and therapeutic exercises.
- Pain Specialists: These professionals may become involved if the pain is severe, persistent, or complex. They can offer advanced interventions and pain management strategies.
- Rheumatologists: Specialists who deal with musculoskeletal diseases and systemic conditions; they are consulted to exclude other potential causes of muscle pain.
However, healthcare professionals from various disciplines collaborate to ensure accurate diagnosis and optimal management of MPS.
Treatment Options for Myofascial Pain Syndrome
Effective management of MPS involves a combination of pharmacological, non-pharmacological, and recent advanced treatments. Here’s a breakdown of these options:
Pharmacological Treatments
- Anti-inflammatory Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen or naproxen, are commonly used to reduce inflammation and alleviate pain.
- Antidepressants: Tricyclic antidepressants, such as amitriptyline, can be prescribed to help relieve pain and improve sleep.
- Muscle Relaxants: These medications help alleviate muscle tension and reduce symptoms of pain. Common examples include cyclobenzaprine and tizanidine.
- Pain Relievers: For more severe cases, doctors may prescribe stronger painkillers, such as tramadol or low-dose opioids, under strict supervision due to the risk of addiction.
- Anticonvulsants: Drugs originally developed to treat epilepsy may help relieve nerve pain. Gabapentin and pregabalin are frequently used anticonvulsants for MPS.
Non-Pharmacological Treatments
- Physical Therapy: Tailored stretching and strengthening exercises can enhance mobility and reduce the impact of trigger points.
- Trigger Point Injections: Saline, local anesthetics, or corticosteroids are injected into the trigger points to alleviate pain.
- Massage Therapy: Therapeutic massage can help relax tight muscles, improve circulation, and ease pain associated with MPS.
- Heat Therapy: Applying heat can help reduce muscle tension and pain, promoting relaxation and flexibility.
- Acupuncture: This traditional Chinese medicine technique involves inserting fine needles into specific points on the body, which may help relieve muscle pain and stiffness.
- Ultrasound Therapy: The use of sound waves to generate heat in deeper tissues can help relax tight muscles and alleviate pain.
Recent Advances in MPS Treatment
- Botulinum Toxin Injections: Recent studies suggest that botulinum toxin can be effective in relieving pain and improving function in patients with MPS by reducing muscle stiffness.
- Laser Therapy: Low-level laser therapy (LLLT) is gaining attention for its ability to penetrate the skin and soft tissues to promote healing and reduce inflammation and pain.
- Dry Needling: Similar to acupuncture, dry needling involves the insertion of a needle without injectable solutions into the trigger points, which can help break the cycle of pain.
- Biofeedback: This technique uses electronic devices to help patients gain control over involuntary bodily functions, such as muscle tension, to reduce pain.
However, consultation with a healthcare provider is essential to tailor the appropriate treatment plan based on individual needs and health conditions.
Self-Management and Lifestyle Modifications for Myofascial Pain Syndrome
Here are essential tips for managing MPS symptoms at home, the importance of exercise and stretching, and dietary considerations that can impact the condition.
Tips for Managing Myofascial Pain Syndrome at Home
- Regular Stretching: Engage in gentle stretching exercises specifically designed for MPS. Stretching helps relieve muscle tightness and reduce pain.
- Heat Therapy: Applying heat can help relax and loosen muscles. Use a heat pad or a warm towel on affected areas to improve blood flow and ease discomfort.
- Cold Therapy: For inflamed areas, cold packs can reduce swelling and numb deep pain. Alternate between heat and cold therapy for the best results.
- Proper Posture: Maintain a good posture to reduce tension and stress on your muscles. Ergonomic adjustments in your workspace can also prevent the worsening of symptoms.
- Stress Management: Since stress can exacerbate MPS, techniques such as meditation, deep-breathing exercises, and yoga can be beneficial in managing stress levels.
Importance of Exercise and Stretching
Exercise is not just about maintaining fitness—it’s crucial for managing MPS. Here’s why it’s beneficial:
- Enhances Muscle Function: Regular physical activity helps keep muscles flexible and strong, which can prevent the formation of new trigger points.
- Improves Circulation: Exercise increases blood flow, which helps to nourish muscles and tissues, accelerating the healing process.
- Reduces Stiffness: Consistent movement prevents muscle stiffness, a common symptom of MPS, and can improve overall mobility.
Incorporating a mix of aerobic activities, strength training, and flexibility exercises into your routine can greatly aid in managing MPS symptoms.
Dietary Considerations and Their Impact on Myofascial Pain Syndrome
What you eat can influence MPS, both positively and negatively. Here are some dietary tips to consider:
- Anti-inflammatory Foods: Incorporate foods rich in omega-3 fatty acids like salmon, flaxseeds, and walnuts, which are known for their anti-inflammatory properties.
- Stay Hydrated: Adequate hydration is crucial as it helps to keep the muscles hydrated and flushes toxins out of the body, potentially reducing muscle pain.
- Limit Sugar and Processed Foods: These can increase inflammation in the body and may exacerbate pain symptoms. Aim for a natural, whole-food-based diet as much as possible.
- Magnesium-Rich Foods: Including foods high in magnesium, such as spinach, chard, and pumpkin seeds, can help in muscle relaxation and pain relief.
By understanding the importance of exercise, stretching, and proper diet, individuals with MPS can lead a more comfortable and active life.
Long-Term Management of Myofascial Pain Syndrome
Below are strategies and insights into maintaining control over MPS and enhancing the quality of life for those affected.
Strategies for Long-Term Care of MPS
- Consistent Physical Therapy: Engaging regularly in physical therapy sessions helps maintain muscle flexibility and strength, which are crucial for managing pain and preventing stiffness.
- Medication Management: Under the guidance of healthcare providers, using medications such as muscle relaxants, anti-inflammatories, or pain relievers can help manage pain levels effectively.
- Trigger Point Injections: For persistent pain, trigger point injections can be a valuable part of a long-term management strategy, providing relief from the discomfort associated with MPS.
- Regular Exercise: Incorporating a routine exercise program tailored to individual needs can improve overall muscle condition and reduce the recurrence of pain.
- Stress Management Techniques: Techniques such as meditation, yoga, and deep breathing exercises can help manage the stress that often exacerbates muscle tension and pain.
Importance of Regular Follow-Up and Reassessment
- Monitoring Progress: Regular check-ups with healthcare providers allow for the monitoring of the condition’s progress and the effectiveness of the treatment plan.
- Adjusting Treatments: Follow-up visits are critical as they help in adjusting treatment strategies based on the patient’s current health status and pain levels.
- Early Detection of Flare-Ups: Consistent reassessments can help in detecting any flare-ups or complications early, allowing for timely interventions.
Coping Strategies and Quality of Life Improvements
- Education About MPS: Understanding the nature of MPS and the factors that exacerbate pain can empower patients to make informed decisions about their lifestyle and treatment options.
- Community Support: Joining support groups where experiences and tips are shared can provide emotional relief and practical advice for coping with MPS.
- Ergonomic Adjustments: Making changes at home and work, such as using ergonomic furniture and tools, can help reduce strain on affected muscles and prevent pain.
- Regular Sleep Patterns: Establishing a regular, restful sleep schedule is vital, as poor sleep can worsen the symptoms of MPS.
- Dietary Changes: Incorporating anti-inflammatory foods into the diet can support muscle health and reduce inflammation.
By implementing these strategies, individuals with Myofascial Pain Syndrome can manage their symptoms more effectively, improving their overall quality of life.
The Future of Myofascial Pain Syndrome Treatment
Emerging Research and Potential New Treatments
The landscape of treatment for Myofascial Pain Syndrome (MPS) is rapidly evolving, driven by groundbreaking research and innovative therapies. Researchers are continually uncovering new aspects of MPS pathology, which in turn fuels the development of advanced treatments. One promising area is the use of biologics, which target specific mechanisms within the body’s response to pain and inflammation. Additionally, advancements in pharmacogenomics hold the potential to tailor medication regimens to individuals based on their genetic makeup, enhancing both efficacy and safety.
Another exciting development is the exploration of neuromodulation techniques. These methods, including transcutaneous electrical nerve stimulation (TENS) and spinal cord stimulation, offer non-pharmacological options for pain management, reducing the reliance on traditional painkillers and minimizing the risk of side effects.
The Role of Technology in Managing MPS
Technology plays a pivotal role in modernizing the management of Myofascial Pain Syndrome. Wearable devices and mobile apps are becoming increasingly prevalent, offering patients real-time monitoring of their symptoms and progress. These tools not only enhance patient engagement and compliance but also provide practitioners with detailed data to better inform treatment decisions.
Telehealth has also become a vital component of MPS management, particularly in the wake of the global pandemic. It allows for consistent patient-provider interactions without the need for physical travel, ensuring that patients receive timely care while minimizing exposure risks. Furthermore, virtual reality (VR) is emerging as a tool for pain distraction techniques, providing immersive environments that help patients manage pain through cognitive diversion.
As research continues and technology advances, the future of Myofascial Pain Syndrome treatment looks promising, with more personalized, effective, and accessible options on the horizon. This ongoing evolution is expected to significantly improve quality of life for those affected by MPS.
FAQs about Myofascial Pain Syndrome Treatment
What is Myofascial Pain Syndrome (MPS)?
Myofascial Pain Syndrome is a chronic condition affecting the fascia (connective tissue) surrounding the muscles. It often involves the development of trigger points, which are tight, painful spots within the muscle fibers.
How is Myofascial Pain Syndrome treated?
Treatment options for MPS include physical therapy, medication, trigger point injections, and lifestyle changes such as exercise and stress management. Each treatment plan is tailored to the individual’s symptoms and overall health.
Can exercise help in managing MPS?
Yes, exercise is a critical component of managing MPS. Activities like stretching, yoga, and strength training can help relieve pain by improving flexibility and reducing muscle tension.
Are there any home remedies for MPS?
Home remedies that may alleviate MPS symptoms include applying heat or cold packs, practicing relaxation techniques, and maintaining proper posture. However, it’s important to consult with a healthcare provider before starting any home treatment.
When should I see a doctor for Myofascial Pain Syndrome?
You should consult a healthcare professional if you experience persistent muscle pain that doesn’t improve with rest and over-the-counter pain relievers, or if the pain disrupts your daily activities.
Is Myofascial Pain Syndrome curable?
While there is no cure for MPS, many patients can manage their symptoms effectively with the right treatment and lifestyle adjustments, leading to a better quality of life.
Conclusion
In conclusion, recognizing the significance of accurate diagnosis is crucial for managing Myofascial Pain Syndrome effectively. This condition, characterized by persistent muscle pain, can significantly impact daily activities and overall quality of life. An accurate diagnosis is the first step toward a tailored treatment plan that can alleviate pain and restore functionality.
We encourage patients experiencing symptoms of Myofascial Pain Syndrome to seek professional medical advice. Adhering to a prescribed treatment regimen, whether it involves physical therapy, medication, or trigger point injections, is essential. Persistence in treatment can lead to substantial improvements in symptoms and an enhanced quality of life.
Remember, the journey to recovery begins with the right diagnosis and continues with committed treatment. Don’t hesitate to consult healthcare providers and explore various treatment options to find what works best for you. Your health and well-being are worth it!
References
For those seeking additional information or verification of the data presented on treatments for Myofascial Pain Syndrome, the following reputable sources are recommended. These references have been carefully selected to provide a deeper understanding and further insight into effective treatment strategies and current research trends:
- National Institute of Health (NIH) – Explore a wide range of peer-reviewed articles and studies detailing the latest advancements in the treatment of Myofascial Pain Syndrome. Visit NIH
- Mayo Clinic – Offers comprehensive details on symptoms, diagnosis, and a variety of treatment options for Myofascial Pain Syndrome, supported by expert medical knowledge. Visit Mayo Clinic
- PubMed Central – Access an extensive database of scientific papers on Myofascial Pain Syndrome, providing in-depth research and clinical findings. Visit PubMed
- WebMD – Find easy-to-understand information on the causes, symptoms, and treatments of Myofascial Pain Syndrome, suitable for non-professionals seeking clear and accurate health information. Visit WebMD
- The American Academy of Pain Medicine – Provides resources on the latest treatment modalities and research in pain management, including detailed sections on Myofascial Pain Syndrome. Visit AAPM
These resources are valuable for both healthcare professionals and patients looking to expand their knowledge on Myofascial Pain Syndrome and explore evidence-based treatment options.