Myasthenia Gravis Treatment: Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder characterized by varying degrees of weakness of the voluntary muscles.
The hallmark of MG is muscle weakness that worsens after periods of activity and improves after periods of rest.
Here, we provide a comprehensive overview of the diagnosis and treatment of Myasthenia Gravis.
Understanding Myasthenia Gravis
Myasthenia Gravis (MG) is an intriguing neurological disorder characterized by weakness and rapid fatigue of any of the muscles under voluntary control. It’s associated with a breakdown in the normal communication between nerves and muscles. Understanding MG involves exploring who it affects and how it impacts the body.
Epidemiology: Who is Affected?
- Prevalence and Incidence: Myasthenia Gravis is relatively rare, affecting about 20 out of every 100,000 people in the United States. However, the incidence has been rising, possibly due to increased awareness and improved diagnostic methods.
- Age and Gender: MG can occur at any age, but there are peaks among women in their 20s and 30s and men in their 50s and 60s, suggesting hormonal and immune system influences.
- Global Distribution: While it affects individuals worldwide, there are variations in prevalence among different regions and ethnic groups, influenced by genetic and environmental factors.
Pathophysiology: How Does MG Affect the Body?
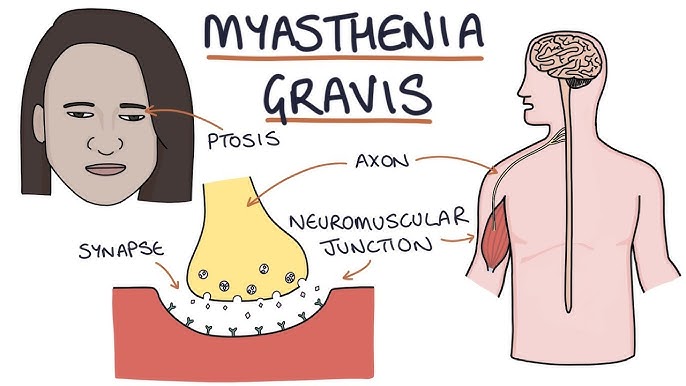
- Autoimmune Reaction: The hallmark of MG is an autoimmune reaction where antibodies mistakenly attack and damage acetylcholine receptors at the neuromuscular junction—the critical point where nerve cells connect with the muscles they control.
- Muscle Fatigue and Weakness: This damage impairs the ability of the receptors to effectively respond to the neurotransmitter acetylcholine, which is essential for muscle contraction. As a result, patients experience muscle weakness and fatigue, especially with sustained activity.
- Impact Across Various Muscles: The severity and specific muscle groups affected can vary widely. Common symptoms include weakness in the eye muscles (resulting in drooping eyelids and double vision), facial expressions, and swallowing. In more severe cases, it can affect limb movements and even respiratory muscles, leading to difficulties in breathing.
However, understanding the epidemiology and pathophysiology of Myasthenia Gravis not only helps in diagnosing and managing this condition but also aids in the research towards more effective treatments and potentially, a cure.
Symptoms of Myasthenia Gravis
Understanding its symptoms can help in early diagnosis and effective management. Below, we explore the common symptoms, their progression over time, and their impact on quality of life.
Common Symptoms Experienced by Patients
- Muscle Weakness: The hallmark symptom of Myasthenia Gravis is muscle weakness that intensifies with activity and eases with rest. This primarily affects voluntary muscles, especially those that control eye movements, facial expressions, chewing, swallowing, and talking.
- Ocular Symptoms: About 85% of patients experience ptosis (drooping of one or both eyelids) and diplopia (double vision), which are often the initial signs of the disorder.
- Facial and Throat Symptoms: Difficulty in swallowing, slurred speech, and changes in facial expressions can occur as the facial muscles weaken.
- Limb Weakness: Weakness in the arms and legs may happen, affecting activities like walking or lifting objects.
- Breathing Difficulty: In severe cases, myasthenia gravis can affect muscles involved in breathing, leading to respiratory failure, which is considered a medical emergency.
How Symptoms Can Progress Over Time
Myasthenia Gravis symptoms can fluctuate and may progressively worsen without treatment. Initially, symptoms such as eye muscle weakness might be mild and not constant; however, they can extend to more severe and broader muscle groups over time. Factors like stress, fatigue, illness, and certain medications can exacerbate symptoms. It’s essential for patients to monitor their condition closely and adjust their treatment plan as needed.
Impact of Symptoms on Quality of Life
The symptoms of Myasthenia Gravis can significantly affect a patient’s quality of life:
- Daily Activities: Routine tasks such as dressing, walking, or eating can become challenging, leading to a dependency on others for basic needs.
- Social Interaction and Emotional Health: Facial muscle weakness can inhibit expressions, affecting social interactions and potentially leading to social withdrawal and depression.
- Employment Challenges: Fluctuating and unpredictable symptoms can make maintaining employment difficult, impacting financial stability and personal fulfillment.
- Overall Health: Complications such as choking, frequent aspiration, and respiratory infections can arise from weakened swallowing and breathing muscles, necessitating vigilant medical care.
However, early diagnosis and tailored treatment are crucial in managing Myasthenia Gravis effectively, helping patients maintain independence and a better quality of life.
Diagnosing Myasthenia Gravis
Diagnosing MG is a critical step in managing its symptoms and improving patient outcomes. Below, we explore the initial steps, diagnostic tests, and the challenges and considerations associated with diagnosing this complex condition.
Initial Steps in Suspecting and Diagnosing Myasthenia Gravis
- Medical History Review: The process begins with a comprehensive review of the patient’s medical history. Clinicians look for signs of muscle weakness that improves with rest and worsens with activity.
- Physical Examination: A thorough physical exam is conducted to assess muscle strength and fatigue. Specific attention is given to the ocular muscles, as drooping eyelids or double vision are often early signs of MG.
- Neurological Examination: This involves a series of tests to evaluate the cranial nerves, muscle strength, reflexes, and coordination. The aim is to identify patterns of weakness typical of MG.
Diagnostic Tests for Myasthenia Gravis
- Acetylcholine Receptor Antibody Test: This blood test detects the presence of antibodies that block, alter, or destroy receptors for acetylcholine at the neuromuscular junction, which are indicative of MG.
- Edrophonium Test: Often referred to as the Tensilon test, this involves the administration of edrophonium chloride to temporarily improve muscle strength in MG patients, suggesting a positive diagnosis.
- Electromyography (EMG): EMG measures the electrical activity of muscle fibers. Repetitive nerve stimulation can reveal a decrease in the muscle’s ability to respond to nerve signals, which is characteristic of MG.
- Imaging Tests: CT scans or MRI may be used to check for thymomas (tumors of the thymus gland), which are associated with MG.
- Ice Pack Test: Particularly useful for diagnosing ocular MG, this test involves placing a cold pack on the eyelid and observing an improvement in ptosis (drooping of the eyelid).
Challenges and Considerations in Diagnosing Myasthenia Gravis
- Variability of Symptoms: MG symptoms can vary widely from patient to patient, which sometimes leads to misdiagnosis. The fluctuating nature of muscle weakness, a hallmark of the disease, complicates diagnosis further.
- Seronegative MG: Approximately 10-20% of MG patients do not have detectable antibodies, making the condition challenging to diagnose through conventional antibody tests.
- Overlap with Other Conditions: MG symptoms can mimic those of other neurological disorders, requiring careful differential diagnosis to rule out conditions like multiple sclerosis or Lambert-Eaton syndrome.
- Age and Gender Factors: MG can affect any age group or gender, but it has peaks among women in their 20s and 30s and men in their 50s and 60s, which can bias the initial clinical approach.
- Response to Treatment: Some patients may respond well to treatments even without a definitive diagnosis, which might delay a formal diagnostic process.
However, diagnosing Myasthenia Gravis requires a meticulous and patient-specific approach, leveraging both clinical expertise and specialized tests to ensure accurate identification and appropriate management of the disease.
Treatment Options for Myasthenia Gravis
There’s no cure for MG, but the symptoms can be managed with various treatments. Here’s an overview of the medications and advanced treatments used to manage this condition.
Medications Used in the Treatment of Myasthenia Gravis
- Cholinesterase Inhibitors: These medications, such as pyridostigmine (Mestinon), work by improving communication between nerves and muscles, thereby increasing muscle strength. They are often the first line of treatment for MG.
- Corticosteroids: Drugs like prednisone can help reduce the immune system’s abnormal response. They are effective in reducing muscle weakness but can have significant side effects, especially with long-term use.
- Immunosuppressants: Medications such as azathioprine, mycophenolate mofetil, and methotrexate decrease the immune response that occurs in MG. These drugs are used for patients who do not respond well to other treatments or when long-term steroid use is contraindicated.
- Monoclonal Antibodies: Newer therapies like eculizumab (Soliris) and rituximab (Rituxan) target specific components of the immune system. They can be very effective, especially for patients with refractory MG.
Advanced Treatments for Myasthenia Gravis
- Plasmapheresis (Plasma Exchange): This procedure removes antibodies from the blood that are involved in the immune response against the neuromuscular junction. It can provide rapid short-term relief of MG symptoms, particularly in crisis situations.
- Intravenous Immunoglobulin (IVIG): IVIG provides the body with normal antibodies, which can alter the immune system’s activity and reduce the abnormal immune response in MG. This treatment is generally used for managing exacerbations or as a bridge to other long-term therapies.
- Thymectomy: This is a surgical procedure to remove the thymus gland, which is believed to play a role in autoimmune reactions in MG. A thymectomy can reduce symptoms in some patients and might be recommended even if a tumor isn’t present in the thymus.
- Biologic Therapies: Treatments like rituximab and eculizumab, which specifically target components of the immune system, represent a newer frontier in MG management. These treatments are often considered when other therapies have failed.
However, understanding these treatment options can empower patients and caregivers to make informed decisions about managing Myasthenia Gravis. With appropriate treatment, many individuals with MG can lead active and fulfilling lives.
Lifestyle and Management Tips for Myasthenia Gravis
With the right adjustments and management strategies, individuals living with MG can lead fulfilling lives. Here are essential tips on lifestyle modifications, the importance of regular monitoring, and the available support systems.
Adjustments and Lifestyle Changes to Manage Symptoms
- Energy Conservation: Plan your day to include regular rest periods to avoid overexertion. Break tasks into smaller, manageable steps and prioritize activities when your energy levels are highest, typically after a good rest.
- Diet and Swallowing: Adopt a diet that is easy to chew and swallow. Soft foods and small, frequent meals can help prevent fatigue associated with eating. Consult with a dietitian to ensure your nutritional needs are met despite dietary adjustments.
- Exercise: Engage in mild, low-impact exercises like walking, swimming, or yoga. Physical activity can help improve overall strength and endurance. Work with a physical therapist to tailor a routine that suits your energy levels and capabilities.
- Avoiding Triggers: Be aware of factors that exacerbate symptoms, such as stress, heat, and certain medications. Educate yourself about potential triggers and discuss them with your healthcare provider.
- Home and Workplace Modifications: Implement practical changes in your living and work environments to reduce strain. Use assistive devices like shower chairs, handrails, and ergonomic furniture to help maintain independence and safety.
Importance of Regular Follow-Up and Monitoring
Regular visits to a healthcare provider are crucial for anyone diagnosed with Myasthenia Gravis. These appointments allow for:
- Medication Adjustments: Monitoring effectiveness and side effects of current medications, and making necessary adjustments.
- Symptom Tracking: Assessing any new symptoms or changes in existing symptoms to tailor treatments effectively.
- General Health Maintenance: Addressing other health issues that might affect MG or be affected by its treatment.
Staying proactive with regular check-ups can significantly influence the quality of life and the management of MG symptoms.
Support Systems and Resources for Patients
Living with Myasthenia Gravis can be challenging, but numerous resources and support systems can help:
- Patient Support Groups: Connecting with others facing similar challenges can provide emotional support, practical tips, and companionship. Look for local or online MG communities.
- Educational Resources: Utilize resources from organizations such as the Myasthenia Gravis Foundation of America (MGFA) which offers educational materials, updates on research, and guidance on living with MG.
- Professional Counseling: Mental health professionals can help manage the emotional and psychological challenges of living with a chronic illness like MG.
- Family and Friends: Educate your close circle about your condition. Support from family and friends can be invaluable in managing daily challenges.
Implementing these management tips and utilizing available resources can help mitigate the effects of Myasthenia Gravis, allowing individuals to lead more active and controlled lives.
Emerging Research and Future Directions of Myasthenia Gravis
Myasthenia Gravis (MG) is a chronic autoimmune disorder characterized by weakness and rapid fatigue of voluntary muscles. The scientific community has made substantial advancements in understanding and treating this condition. Here, we explore the most recent developments, ongoing clinical trials, and the promising future of personalized medicine in managing MG.
Recent Advancements in the Treatment of Myasthenia Gravis
Several recent advancements have significantly impacted the treatment landscape of Myasthenia Gravis. These include:
- New Monoclonal Antibodies: Efgartigimod, a neonatal Fc receptor blocker that reduces pathogenic IgG antibodies, has shown promising results and was approved by the FDA in recent years.
- Improved Thymectomy Techniques: Minimally invasive surgical approaches for thymus gland removal have improved outcomes and recovery times.
- Advances in Immunotherapy: Rituximab, though not new, has gained traction for its off-label use in treating MG, offering another option for patients who do not respond to traditional therapies.
Ongoing Clinical Trials and Emerging Therapies
The landscape of clinical trials for Myasthenia Gravis is robust, with several innovative therapies being tested:
- Firdapse (Amifampridine): Ongoing trials are investigating its effectiveness in a broader range of MG symptoms.
- B-cell Maturation Antigen (BCMA) Targeted Therapy: This novel approach is being explored to reduce specific antibody-producing cells in MG patients.
- Gene Therapy and Cellular Therapies: Early-stage trials are looking into correcting the underlying immune dysfunction in MG.
The Future of Personalized Medicine in Managing Myasthenia Gravis
Personalized medicine is poised to transform the management of Myasthenia Gravis by tailoring treatments to individual genetic profiles, lifestyle, and disease patterns:
- Genetic Profiling: Identifying genetic factors that contribute to MG can lead to more targeted and effective treatments.
- Biomarker Development: Developing biomarkers to predict treatment responses will enhance treatment efficacy and minimize side effects.
- Integration of Digital Health Tools: Wearable technology and mobile apps designed to monitor symptoms and treatment responses can significantly improve patient outcomes and quality of life.
However, these exciting developments not only promise better management of Myasthenia Gravis but also a more hopeful future for those affected by this challenging condition.
FAQs about Myasthenia Gravis Treatment
What is the first line of treatment for Myasthenia Gravis?
The initial treatment typically involves medications such as anticholinesterase agents which improve neuromuscular transmission and increase muscle strength. For some patients, corticosteroids or immunosuppressants may also be prescribed to reduce the immune system’s abnormal response.
Are there surgical options for Myasthenia Gravis?
Yes, thymectomy, the surgical removal of the thymus gland, is a common procedure for Myasthenia Gravis. This surgery is often recommended if a thymoma is present and can help reduce symptoms in some patients, even those without a thymoma.
Can Myasthenia Gravis be treated without surgery?
Absolutely. Many patients manage their condition with medications and lifestyle adjustments without needing surgery. Treatments may include medications like anticholinesterase inhibitors, corticosteroids, and other immunosuppressants.
What lifestyle changes can help manage Myasthenia Gravis symptoms?
Patients are often advised to avoid fatigue and to pace their activities. Eating smaller, more frequent meals can help if chewing or swallowing is difficult. Adjusting living spaces to be more accessible can also significantly help in managing daily activities.
Is Myasthenia Gravis curable?
Currently, there is no cure for Myasthenia Gravis, but treatment can effectively manage symptoms and improve quality of life. Most individuals with proper treatment can lead active lives, although monitoring and adjustments in treatment plans are often necessary.
Conclusion
In this discussion, we have explored the critical aspects of Myasthenia Gravis, focusing on the latest treatment options and strategies for managing this complex condition. For patients and healthcare providers alike, staying abreast of these advancements is paramount.
We encourage both groups to continually seek out new information and participate in ongoing education to ensure that those affected by Myasthenia Gravis receive the most effective and innovative care possible.
Together, by keeping informed and proactive, we can significantly improve outcomes and quality of life for those battling this disease.
References
For further reading and to validate the information provided on Myasthenia Gravis treatment, the following sources are highly recommended. These references are reputable and provide comprehensive insights into various aspects of managing and treating Myasthenia Gravis:
- National Institute of Neurological Disorders and Stroke (NINDS) – Provides detailed information on symptoms, diagnosis, and the latest treatment options for Myasthenia Gravis. Read more about Myasthenia Gravis on NINDS.
- Myasthenia Gravis Foundation of America (MGFA) – Offers resources for patients, including treatment guidelines, support groups, and research updates. Visit MGFA’s official website.
- Mayo Clinic – Features an extensive section on Myasthenia Gravis, covering everything from lifestyle recommendations to treatment advancements. Explore Mayo Clinic’s Myasthenia Gravis resources.
- PubMed Central – An invaluable resource for accessing scientific studies and clinical trial results on Myasthenia Gravis treatments. Search for Myasthenia Gravis studies on PubMed.
These sources are trustworthy and provide the most current and comprehensive information available on Myasthenia Gravis, ensuring readers have access to reliable data for better understanding and management of the condition.