Mitral Valve Stenosis Treatment: Mitral Valve Stenosis (MVS) is a serious heart condition where the mitral valve does not fully open, restricting blood flow from the left atrium to the left ventricle.
This article provides an in-depth analysis of the diagnosis and treatment options for Mitral Valve Stenosis, aiming to offer comprehensive insights for patients and healthcare providers alike.
Understanding Mitral Valve Stenosis
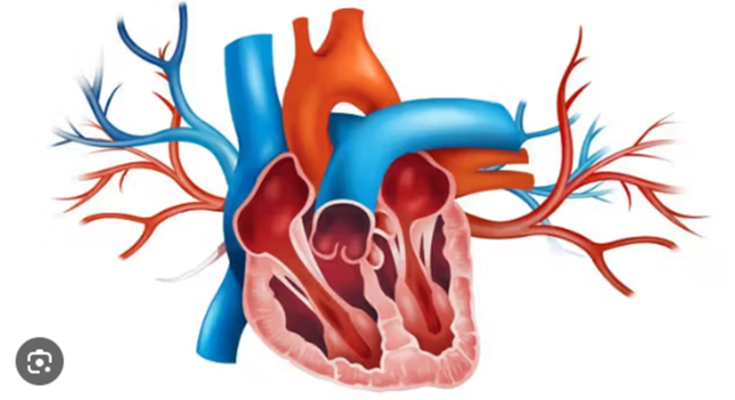
Mitral Valve Stenosis (MVS) is a heart condition characterized by the narrowing of the mitral valve, which restricts blood flow from the left atrium to the left ventricle. This section delves into the prevalence and risk factors associated with MVS, along with its pathophysiological impact on heart function.
Statistics: Prevalence and Risk Factors
Mitral Valve Stenosis predominantly affects individuals in their middle ages but can be diagnosed at any age depending on underlying causes such as rheumatic heart disease. Here are some key statistics and risk factors:
Prevalence: It is estimated that about 0.1% to 0.2% of the global population is affected by MVS.
Risk Factors:
- Rheumatic Fever: The most common cause worldwide, resulting from untreated streptococcal throat infections.
- Age: The risk increases with age, particularly due to the degeneration of heart tissues.
- Gender: Women are more commonly affected than men, with a ratio of about 2:1.
- Hereditary Factors: A family history of valvular disease can predispose individuals to MVS.
- Other Health Conditions: Conditions like connective tissue disorders can increase the risk of developing MVS.
Pathophysiology: How MVS Affects Heart Function
The pathophysiological effects of Mitral Valve Stenosis on heart function are significant and complex:
- Blood Flow Restriction: The narrowed mitral valve limits the blood volume that can flow into the left ventricle, reducing overall cardiac output.
- Pressure Overload: To compensate, the left atrium must work harder, leading to increased pressure and atrial enlargement.
- Pulmonary Hypertension: Elevated atrial pressures can be transmitted back into the pulmonary circulation, leading to increased pressure in the pulmonary arteries (pulmonary hypertension).
- Atrial Fibrillation: As the left atrium enlarges, there is a higher risk of developing atrial fibrillation, which further complicates heart rhythm and function.
- Heart Failure: Chronic pressure overload can eventually lead to heart failure if the condition is not managed effectively.
However, understanding these dynamics is crucial for diagnosing and managing Mitral Valve Stenosis effectively, ensuring that patients receive timely and appropriate care to mitigate the progression of the disease.
Symptoms of Mitral Valve Stenosis
Mitral valve stenosis is a heart condition where the mitral valve narrows, restricting blood flow from the left atrium to the left ventricle. This can lead to a variety of symptoms that affect individuals differently depending on the severity of the condition.
Common Symptoms Experienced by Patients
Patients with mitral valve stenosis may experience a range of symptoms, including:
- Shortness of Breath: This typically occurs during exertion or when lying down. It is caused by fluid build-up in the lungs due to poor blood flow out of the left atrium.
- Fatigue: Reduced blood flow can limit oxygen delivery to the body, resulting in persistent tiredness.
- Heart Palpitations: Irregular heartbeats or a feeling of fluttering in the chest can occur as the heart struggles to maintain a proper rhythm.
- Swollen Feet or Ankles: Fluid retention in the extremities is a common result of the heart’s reduced ability to pump effectively.
- Frequent Respiratory Infections: Due to fluid accumulation in the lungs, individuals may experience repeated respiratory infections.
Impact of Symptoms on Daily Life and Long-Term Health
The symptoms of mitral valve stenosis can significantly impact daily life and long-term health:
- Reduced Physical Activity: Shortness of breath and fatigue may limit physical activity, affecting overall fitness and quality of life.
- Complications in Other Body Systems: Persistent symptoms can strain the heart and other organs, potentially leading to heart failure or pulmonary hypertension.
- Social and Emotional Effects: The limitations caused by this condition can also affect mental health, leading to feelings of isolation or depression.
- Progressive Deterioration: If untreated, mitral valve stenosis can progressively worsen, increasing the risk of severe complications, including stroke.
However, regular consultations with a healthcare provider are essential for monitoring the condition and making appropriate adjustments to treatment plans.
Diagnosing Mitral Valve Stenosis
Proper diagnosis is crucial for effective treatment and management. Below, we outline the steps involved in diagnosing this condition, focusing on initial evaluations, key diagnostic tests, and the advanced role of cardiac MRI.
Initial Evaluation and Medical History
- Patient Interview: The process begins with a detailed interview where the doctor asks about symptoms such as breathlessness, fatigue, or chest pain. Understanding the patient’s medical history, including any previous heart conditions or rheumatic fever, is also essential.
- Physical Examination: A physical exam helps identify any physical signs of mitral valve stenosis. This includes listening to the heart for abnormal heart sounds, such as a heart murmur, which is common in mitral stenosis.
- Family History: Gathering information about family health history can provide clues about the potential genetic predispositions to heart issues.
Key Diagnostic Tests
- Echocardiogram: This is the primary diagnostic tool for mitral valve stenosis. It uses sound waves to create a detailed image of the heart, showing the structure of the mitral valve and the flow of blood through it.
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart and can detect arrhythmias, which often accompany mitral valve stenosis.
- Chest X-ray: This test checks for signs of heart enlargement and assesses the condition of the lungs, which can be affected by changes in heart function due to mitral valve stenosis.
The Role of Cardiac MRI in Advanced Diagnosis
While echocardiography is the standard in diagnosing mitral valve stenosis, Cardiac Magnetic Resonance Imaging (MRI) plays a crucial role in advanced diagnosis. Cardiac MRI provides detailed images of the heart’s structure and function, offering valuable insights that are not available with other imaging methods. This test is particularly useful in assessing the severity of the stenosis and planning for potential surgical interventions. It can also provide a more comprehensive assessment of the heart’s overall health, aiding in a more accurate diagnosis and better treatment planning.
Through these diagnostic steps, healthcare providers can effectively assess and manage mitral valve stenosis, improving patient outcomes and quality of life.
Treatment Options for Mitral Valve Stenosis
Mitral Valve Stenosis (MVS) is a heart condition that requires timely intervention to manage symptoms and improve heart function. This section outlines the various treatment options available, aiming to enhance patient outcomes through effective strategies.
General Treatment Goals for MVS
The primary goals for treating Mitral Valve Stenosis include:
- Alleviating symptoms such as breathlessness and fatigue.
- Preventing complications like atrial fibrillation and pulmonary hypertension.
- Improving heart function and quality of life.
- Monitoring the progression of the disease to adjust treatments as necessary.
Medical Management
Medical management for MVS focuses on symptom control and slowing the progression of the disease. Common approaches include:
- Diuretics: Used to reduce fluid accumulation and ease the strain on the heart.
- Beta-blockers: Help in managing heart rate, improving heart function and reducing symptoms.
- Anticoagulants: Prescribed to prevent blood clots, especially in patients with atrial fibrillation.
- Regular follow-ups and echocardiograms to monitor heart function and valve condition.
Interventional Procedures
When medical management is not sufficient, interventional procedures may be necessary:
- Balloon Valvuloplasty: A catheter with a balloon is inserted and inflated to widen the mitral valve, improving blood flow.
- This procedure is typically recommended for selected patients, particularly those who are not ideal candidates for surgery.
Mitral Valve Repair or Replacement
Surgical options are considered when symptoms are severe or the valve is extensively damaged:
- Valve Repair: Involves modifying the existing valve to improve function. It is often preferred over replacement as it preserves the natural heart structure and function.
- Valve Replacement: Involves removing the diseased valve and replacing it with a mechanical or biological valve. This option is chosen when repair is not feasible.
Innovations in Minimally Invasive Surgery
Advancements in minimally invasive techniques have significantly improved the treatment of MVS:
- Robotic-assisted Surgery: Offers precision and smaller incisions, which lead to quicker recovery and reduced hospital stays.
- Transcatheter Mitral Valve Repair (TMVR): A less invasive option compared to traditional surgery, where devices are used to clip parts of the valve together, improving valve function without the need for open heart surgery.
However, these treatment options for Mitral Valve Stenosis are designed to tailor interventions to individual patient needs, maximizing the efficacy of the treatment while minimizing the risks and recovery time.
Choosing the Right Treatment Approach
Selecting the appropriate treatment approach is pivotal in managing any health condition effectively. This process involves various factors and requires active collaboration between healthcare professionals and patients. Here’s an insightful look into the components that influence treatment decisions and how these decisions are made:
Factors Influencing Treatment Choice
- Diagnosis and Stage of Condition: Understanding the specific diagnosis and the stage of the condition is crucial as it dictates the treatment options available.
- Patient’s Overall Health: The general health status of the patient, including any underlying conditions or comorbidities, significantly influences the choice of treatment.
- Evidence-based Recommendations: Treatments backed by scientific research and clinical trials often provide the best outcomes and guide decision-making.
- Availability of Treatments: Accessibility and availability of certain treatments can affect choice, especially in areas with limited healthcare resources.
- Potential Side Effects: Considering the possible side effects and weighing them against the benefits of the treatment is essential.
- Cost and Insurance Coverage: Financial aspects, including treatment costs and insurance coverage, can play a decisive role in choosing a treatment.
The Role of the Healthcare Team in Treatment Planning
- Assessment and Diagnosis: Medical professionals use their expertise to accurately diagnose and assess the patient’s condition.
- Discussion of Options: Healthcare providers present all viable treatment options, explaining the benefits and risks associated with each.
- Coordinating Care: The healthcare team coordinates various aspects of care, ensuring all treatments are harmoniously integrated.
- Monitoring Progress: Ongoing evaluation of the treatment effectiveness and making adjustments as necessary is a critical role of the healthcare team.
Patient Participation in Treatment Decisions
- Expressing Preferences and Concerns: Patients are encouraged to share their values, preferences, and concerns which influence treatment choices.
- Informed Consent: Patients receive comprehensive information about the potential benefits and risks of treatments to make informed decisions.
- Self-Management of Care: Educating patients on managing aspects of their care at home promotes better health outcomes.
- Feedback on Treatment Efficacy: Patients’ feedback on the effectiveness of treatments helps tailor future care plans.
However, understanding these elements can empower patients and clinicians to make well-informed treatment decisions that best meet the individual’s health needs.
Living with Mitral Valve Stenosis
Adapting your lifestyle and ensuring consistent medical monitoring are crucial for maintaining your health and quality of life. Additionally, leveraging support groups and resources can provide valuable emotional and informational support.
Lifestyle Adjustments and Home Care
- Regular Exercise: Engage in gentle activities such as walking or swimming, which can help maintain heart health without overexertion.
- Healthy Diet: Opt for a low-salt diet to reduce the risk of fluid retention and swelling, common issues in heart valve diseases.
- Weight Management: Maintain a healthy weight to decrease the workload on your heart and reduce symptoms.
- Avoid Smoking: Smoking can worsen heart conditions and should be avoided. If needed, seek help to quit smoking.
- Limit Alcohol: Minimize alcohol intake as it can affect your heart rate and rhythm, impacting the mitral valve.
- Stress Management: Use relaxation techniques such as yoga, meditation, or deep breathing exercises to manage stress effectively.
Importance of Regular Follow-Up and Monitoring
- Routine Check-Ups: Regular visits to your cardiologist are essential to monitor the progression of your condition and adjust treatments as necessary.
- Echocardiograms: Frequent echocardiograms can help assess valve function and detect changes or complications early.
- Medication Adherence: Follow your prescribed medication regimen closely to prevent complications and manage symptoms.
- Symptom Tracking: Keep a log of any new or worsening symptoms and report them to your healthcare provider promptly.
Support Groups and Patient Resources
- Local Support Groups: Join support groups where you can meet others living with heart valve diseases. Sharing experiences can provide emotional relief and practical tips.
- Online Communities: Participate in online forums and social media groups which offer a platform to discuss daily challenges and learn from others’ experiences.
- Educational Materials: Utilize resources provided by heart health organizations like the American Heart Association, which offer comprehensive guides on managing heart valve conditions.
- Professional Counseling: Consider professional counseling to help cope with the emotional aspects of living with a chronic condition.
However, managing mitral valve stenosis effectively involves a comprehensive approach that includes lifestyle modifications, consistent medical care, and a supportive community.
Advancements in Mitral Valve Stenosis Treatment
Recent years have seen significant advancements in the treatment of MVS, driven by cutting-edge research, innovative therapies, and emerging technologies.
Recent Research and Clinical Trials
Recent research has focused on refining surgical techniques and developing minimally invasive procedures to treat MVS. Notable clinical trials include studies on balloon mitral valvuloplasty, which have demonstrated improved patient outcomes with reduced recovery times. Another area of active research is the use of 3D printing technology to create custom-fit prosthetic valves, which aim to improve the precision and effectiveness of valve replacement surgeries.
Emerging Therapies and Technologies
Emerging therapies for MVS are transforming the treatment landscape. One of the promising developments is the transcatheter mitral valve replacement (TMVR), a procedure that allows for the replacement of the mitral valve via a catheter, avoiding the need for open-heart surgery. Additionally, robotic-assisted surgeries are gaining traction, offering enhanced precision and reduced trauma for patients undergoing valve repair or replacement.
Future Outlook in MVS Treatment
The future of MVS treatment looks promising, with ongoing advancements in biomedical engineering and genetic research. Researchers are exploring the potential of gene therapy to reverse valve thickening and prevent stenosis at a molecular level. Moreover, advancements in imaging and diagnostic technologies are expected to lead to earlier and more accurate diagnoses, facilitating timely interventions and better management of the disease. As these technologies continue to evolve, they promise to further enhance the efficacy, safety, and accessibility of treatments for patients suffering from mitral valve stenosis.
FAQs about Mitral Valve Stenosis Treatment
What is mitral valve stenosis?
Mitral valve stenosis is a heart condition where the mitral valve, which lies between the left atrium and left ventricle, narrows. This narrowing impedes the flow of blood from the atrium to the ventricle, causing various cardiac complications.
What are the common symptoms of mitral valve stenosis?
Symptoms typically include shortness of breath, particularly during exertion or when lying down, fatigue, swollen feet or ankles, and a feeling of palpitations, which are sensations of a rapid, fluttering heartbeat.
How is mitral valve stenosis diagnosed?
Diagnosis generally involves a physical exam, listening for a heart murmur, and confirming through echocardiography, which provides detailed images of the heart’s structure and function.
What treatments are available for mitral valve stenosis?
Treatment options vary based on the severity of the condition and can range from medications to manage symptoms to more invasive procedures like balloon valvuloplasty or mitral valve replacement, depending on the individual case.
Is surgery always necessary for treating mitral valve stenosis?
Not always. Surgery is recommended when symptoms are severe or worsening. In less severe cases, monitoring and medication may suffice to manage the condition.
What are the risks of mitral valve stenosis treatment?
As with any treatment, risks are present. Surgical treatments carry risks such as bleeding, infection, and reactions to anesthesia. Non-surgical treatments can involve side effects from medications.
How can I prevent mitral valve stenosis?
While congenital issues cannot be prevented, minimizing rheumatic fever risks by treating strep throat and other infections promptly can help prevent rheumatic heart disease, a common cause of mitral valve stenosis.
Can lifestyle changes help with mitral valve stenosis?
Yes, lifestyle changes such as maintaining a healthy weight, managing blood pressure, and avoiding excessive alcohol can help manage the symptoms and progression of the disease.
Conclusion
Medical advancements have significantly improved the options available for managing this condition. Diagnostic methods such as echocardiography provide precise insights into the valve’s condition, facilitating targeted treatments. Depending on the severity of the stenosis, treatments may range from medication to control symptoms to more definitive interventions like balloon valvuloplasty or valve replacement surgery.
For patients diagnosed with Mitral Valve Stenosis, it is crucial to engage actively with healthcare providers to determine the most effective treatment plan. Adherence to prescribed treatments and regular follow-up appointments are fundamental to managing the condition successfully. Always consult your cardiologist or healthcare provider for advice tailored to your specific health needs.
Remember, dealing with Mitral Valve Stenosis is a journey that requires attention and care, but with the right approach, it can be managed effectively, allowing for a healthier and more active life.
References
For further reading and validation of the information provided on the treatment of Mitral Valve Stenosis, the following resources are highly recommended:
- American Heart Association (AHA) – Provides comprehensive details on various heart conditions, including mitral valve stenosis. Their resources are pivotal for understanding symptoms, causes, and treatments. Read more about Mitral Valve Stenosis at AHA.
- Mayo Clinic – Offers a thorough exploration of diagnosis and treatment options for mitral valve stenosis, supported by expert medical insights. Explore Mitral Valve Stenosis Treatment Options.
- Johns Hopkins Medicine – Features an in-depth guide to the surgical and nonsurgical treatment approaches for mitral valve stenosis. Learn about Surgical Options at Johns Hopkins.
These sources are reputable and provide valuable insights and data that are crucial for anyone seeking detailed and reliable information on mitral valve stenosis.