Microscopic Colitis Symptoms: Microscopic colitis is a chronic condition characterized by inflammation of the colon that is only visible under a microscope.
Unlike more common types of colitis, its inflammation cannot be detected by the naked eye or standard imaging tests.
This article delves deep into the symptoms and causes of microscopic colitis, offering essential insights for those affected by or interested in this less understood condition.
What is Microscopic Colitis?
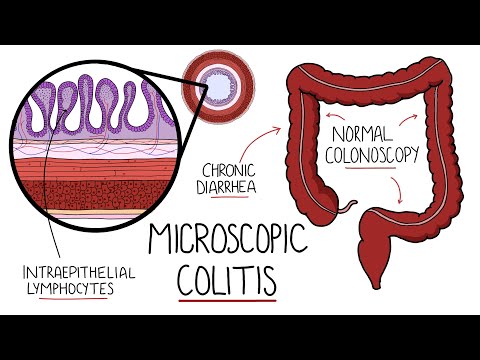
Microscopic colitis is an inflammatory bowel disease that affects the colon (large intestine). It is termed “microscopic” because the inflammation or changes to the tissue are not visible to the naked eye; instead, they can only be seen under a microscope. This condition is characterized by chronic, watery diarrhea and abdominal discomfort, but unlike other forms of colitis, it typically does not cause bloody stools or visible signs of inflammation during a colonoscopy or flexible sigmoidoscopy.
Differences Between Microscopic Colitis and Other Forms of Colitis
Microscopic colitis differs from other types of colitis in several key ways:
- Visibility of Inflammation: Unlike ulcerative colitis or Crohn’s disease, where inflammation is visible during a colonoscopy, the inflammation in microscopic colitis can only be detected through microscopic examination of colon tissue samples.
- Symptoms: While ulcerative colitis and Crohn’s disease often cause bloody diarrhea and significant abdominal pain, microscopic colitis usually presents with non-bloody, watery diarrhea and minimal pain.
- Location of Inflammation: Microscopic colitis affects the colon uniformly, whereas Crohn’s disease can affect any part of the gastrointestinal tract and ulcerative colitis typically starts at the rectum and extends continuously to part of the colon.
- Complications: The risk of severe complications like colon perforations or significant bleeding is lower in microscopic colitis compared to Crohn’s disease or ulcerative colitis.
- Demographic: Microscopic colitis is more commonly diagnosed in middle-aged and older adults, especially women, while other forms of colitis can occur in younger age groups and show less gender disparity.
However, understanding these differences is crucial for accurate diagnosis and effective treatment. While the symptoms of microscopic colitis can be disruptive, the overall prognosis is good, and management strategies can significantly improve quality of life.
Symptoms of Microscopic Colitis
Understanding the common symptoms associated with microscopic colitis is crucial for timely diagnosis and management.
Common Symptoms of Microscopic Colitis
- Chronic Watery Diarrhea: This is the hallmark symptom of microscopic colitis. Unlike other forms of diarrhea, it is typically non-bloody.
- Abdominal Pain: Patients may experience mild to moderate cramping that can vary in intensity.
- Weight Loss: Unintentional weight loss can occur as the condition progresses due to malabsorption of nutrients.
- Fatigue: Persistent diarrhea and nutrient loss can lead to general fatigue and weakness.
- Dehydration: Due to frequent watery stools, dehydration is a common concern and can present with symptoms such as dry mouth and increased thirst.
- Bloating and Gas: Abdominal bloating and gas are frequently reported by patients.
How Symptoms of Microscopic Colitis Differ from Other Gastrointestinal Disorders
Microscopic colitis shares several symptoms with other gastrointestinal disorders, which can sometimes complicate the diagnosis. However, there are distinct differences that help differentiate it:
- Absence of Blood in Stools: Unlike ulcerative colitis or Crohn’s disease, microscopic colitis usually does not involve bloody stools.
- Symptom Pattern: The symptoms of microscopic colitis can be intermittent, with periods of worsening followed by periods of remission, which is less common in other inflammatory bowel diseases.
- Age of Onset: Microscopic colitis is more commonly diagnosed in middle-aged and older adults, which differs from Crohn’s disease and ulcerative colitis, often starting in younger individuals.
- Response to Treatment: Microscopic colitis typically responds well to certain medications like budesonide, which specifically targets the inflammation in the colon without the broader side effects of other corticosteroids.
By understanding these symptoms and their unique characteristics, individuals can seek appropriate medical attention for diagnosis and treatment, leading to better management of their condition.
Causes and Risk Factors of Microscopic Colitis
Understanding the causes and risk factors associated with this condition is crucial for prevention and management. Here’s a detailed look at what may lead to microscopic colitis and the factors that increase one’s risk.
Causes of Microscopic Colitis
The exact causes of microscopic colitis are not entirely understood, but several factors are thought to contribute to its development:
- Autoimmune Response: The body’s immune system mistakenly attacks the normal bacteria in the colon or the cells of the colon lining, leading to inflammation.
- Bacterial Infection: Certain bacteria, such as those that cause food poisoning, might trigger inflammation in the colon.
- Viral Infections: Some viral infections are known to cause transient inflammatory responses in the digestive system, which may evolve into microscopic colitis.
- Bile Acid Malabsorption: Improper handling of bile acids by the colon can cause irritation and inflammation in the colon lining.
Risk Factors of Microscopic Colitis
Several risk factors have been identified that may increase the likelihood of developing microscopic colitis:
- Age: Microscopic colitis is more commonly diagnosed in individuals over the age of 50.
- Gender: Women are more likely to develop this condition than men.
- Smoking: Current or former smokers have been shown to have a higher risk of developing microscopic colitis.
- Family History: Individuals with a family history of inflammatory bowel disease may have an increased risk of microscopic colitis.
Connection between Medications and the Development of Microscopic Colitis
Medications play a significant role in the development of microscopic colitis. Certain medications have been linked to its onset:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These drugs, such as ibuprofen and aspirin, can cause irritation and inflammation in the colon.
- Proton Pump Inhibitors (PPIs): Used to reduce stomach acid, long-term use of PPIs has been associated with an increased risk of microscopic colitis.
- Selective Serotonin Reuptake Inhibitors (SSRIs): Some studies suggest that SSRIs, commonly used as antidepressants, may increase the risk of microscopic colitis.
- Statins: These cholesterol-lowering medications might also be linked to an increased risk of developing microscopic colitis.
If you are experiencing symptoms and fall into one or more of the risk categories, consulting with a healthcare provider is advised for proper assessment and treatment.
Diagnosing Microscopic Colitis
Understanding the diagnostic process can help patients and healthcare providers effectively identify and manage this condition.
Importance of Medical History and Symptom Reporting
- Comprehensive Medical History Review: Gathering a detailed medical history is crucial. This includes discussing any previous health issues, family history of gastrointestinal diseases, and any medications that could influence colon health, such as nonsteroidal anti-inflammatory drugs (NSAIDs).
- Symptom Assessment: Patients typically report symptoms such as chronic watery diarrhea, abdominal pain, and unexplained weight loss. Accurate reporting of the onset, duration, and severity of these symptoms is essential for guiding further diagnostic investigations.
Diagnostic Tests and Procedures
- Blood Tests: These can help rule out other conditions that mimic microscopic colitis, such as infections or inflammatory bowel disease (IBD). Blood tests can check for signs of inflammation, anemia, or other markers that indicate underlying health issues.
- Stool Samples: Analyzing stool samples helps exclude infections caused by parasites, bacteria, or viruses, which can present symptoms similar to those of microscopic colitis.
- Colonoscopy with Biopsy: The definitive test for diagnosing microscopic colitis is a colonoscopy combined with a biopsy. During this procedure, a flexible tube equipped with a camera (colonoscope) is inserted into the rectum to visually examine the entire colon. Small samples of tissue (biopsies) are collected from the lining of the colon and examined under a microscope to detect inflammation and cellular changes indicative of microscopic colitis.
- Imaging Tests: Occasionally, imaging tests like CT scans or X-rays are used to assess the condition of the colon and rule out other diseases.
By carefully combining medical history with targeted tests, healthcare providers can accurately diagnose microscopic colitis, paving the way for effective treatment and management of the condition.
Treatment Options for Microscopic Colitis
There are various treatment strategies can effectively manage symptoms and improve quality of life. This guide outlines the current treatment modalities, medications, and lifestyle adjustments beneficial for managing microscopic colitis.
Current Treatment Modalities
Treatment for microscopic colitis is aimed at reducing inflammation, managing symptoms, and maintaining remission. Here are the primary treatment approaches:
- Medication Therapy: This is the cornerstone of treatment for managing and reducing the symptoms of microscopic colitis.
- Lifestyle Adjustments: Incorporating specific lifestyle changes can help lessen the severity of symptoms.
- Dietary Management: Adjusting your diet plays a crucial role in controlling symptoms and preventing flare-ups.
Medications and Their Roles in Managing Symptoms
Several medications are used to treat microscopic colitis, each serving a unique role in symptom management:
- Anti-inflammatory Drugs: Budesonide is a commonly prescribed corticosteroid that helps reduce intestinal inflammation effectively with fewer side effects than other steroids.
- Antidiarrheal Agents: Medications like loperamide and bismuth subsalicylate can help control diarrhea, a common symptom of microscopic colitis.
- Immunosuppressive Medications: For severe cases or those resistant to other treatments, drugs like azathioprine or methotrexate might be used to suppress the immune system’s activity.
- Bile Acid Binders: These medications, such as cholestyramine, help bind bile acids in the gut when diarrhea is not responsive to other treatments.
Lifestyle and Dietary Adjustments to Mitigate Symptoms
Lifestyle and dietary changes are often recommended to help manage microscopic colitis. Here are some effective strategies:
- Avoiding Irritants: Steer clear of tobacco, caffeine, and nonsteroidal anti-inflammatory drugs (NSAIDs), as these can exacerbate symptoms.
- Diet Modification: Implementing a low-fat, low-fiber, or gluten-free diet may help reduce symptoms. It’s essential to identify and avoid foods that trigger symptoms.
- Stress Management: Techniques like yoga, meditation, or therapy can reduce stress, which may in turn help manage flare-ups.
However, always consult with a healthcare provider to tailor the treatment plan to your specific needs and monitor the condition effectively.
Living with Microscopic Colitis
Managing this condition requires a careful approach to diet, lifestyle, and medical care. Here are some tips for navigating daily life with microscopic colitis, along with the importance of support from healthcare providers and support groups.
Tips for Managing Daily Life with Microscopic Colitis
- Follow a Suitable Diet: Identify and avoid foods that trigger symptoms. Common irritants include caffeine, dairy, spicy foods, and fatty foods. Consider working with a dietitian to develop a personalized eating plan.
- Stay Hydrated: Due to frequent diarrhea, it’s crucial to maintain hydration. Drink plenty of water throughout the day, and consider oral rehydration solutions if necessary.
- Use Medications Wisely: Be consistent with any prescribed medications. Anti-inflammatory drugs and steroids are commonly used to manage inflammation and symptoms. Always discuss potential side effects and treatment adjustments with your doctor.
- Manage Stress: Stress can exacerbate symptoms of microscopic colitis. Techniques such as yoga, meditation, and regular exercise can help manage stress levels.
- Plan Ahead: When going out, locate restrooms ahead of time to reduce anxiety about sudden symptom onset. Carrying a ‘just-in-case’ kit with essentials like extra clothing, wet wipes, and over-the-counter medications can also be helpful.
- Keep a Symptoms Diary: Track your food intake, symptoms, and any other relevant factors like stress or medication changes. This diary can help identify triggers and monitor the effectiveness of your treatment.
Importance of Support from Healthcare Providers and Support Groups
- Expert Guidance: Regular consultations with gastroenterologists or other healthcare providers specializing in digestive disorders are essential. They can offer tailored advice, adjust treatments, and monitor the progression of the disease.
- Emotional and Practical Support: Living with a chronic illness can be emotionally taxing. Support groups provide a platform to share experiences, offer encouragement, and exchange practical advice on managing the condition.
- Access to Resources: Healthcare providers and support groups can provide valuable resources such as information about the latest treatments, tips for dietary management, and insights into coping mechanisms that have worked for others.
- Advocacy and Awareness: Healthcare providers and support organizations can advocate for greater awareness and better resources for those living with microscopic colitis, potentially leading to improved care and support systems.
By implementing these management strategies and utilizing available supports, individuals with microscopic colitis can lead fulfilling lives despite the challenges posed by the condition.
FAQs about Microscopic Colitis Symptoms
What is microscopic colitis?
Microscopic colitis is an inflammation of the colon that is only visible under a microscope. It’s characterized by chronic, watery diarrhea and is not typically associated with blood in the stool. This condition is most commonly diagnosed in middle-aged and older adults.
What are the main symptoms of microscopic colitis?
The primary symptom of microscopic colitis is chronic watery diarrhea that occurs without the presence of blood. Other common symptoms include abdominal pain or cramps, weight loss, and fatigue. Some individuals may also experience dehydration due to the frequent diarrhea.
How is microscopic colitis different from other forms of colitis?
Unlike ulcerative colitis or Crohn’s disease, which can cause visible inflammation and ulcers on the colon’s surface, the inflammation in microscopic colitis can only be detected through microscopic examination of colon tissue. Also, microscopic colitis does not typically lead to bloody stools or the severe complications often associated with other inflammatory bowel diseases.
Can diet affect microscopic colitis?
Yes, certain foods and beverages may exacerbate symptoms of microscopic colitis. Common triggers include caffeine, lactose, spicy foods, and fatty foods. Patients are often advised to modify their diet to help manage symptoms and identify specific triggers.
Is microscopic colitis curable?
While there is no cure for microscopic colitis, it can be effectively managed with medication and lifestyle changes. Treatment typically involves anti-inflammatory medications to reduce bowel inflammation and dietary adjustments to avoid symptom triggers. In many cases, symptoms can be well-controlled, allowing individuals to lead normal, active lives.
Conclusion
In summary, microscopic colitis, a condition characterized by inflammation of the colon, manifests through symptoms such as chronic watery diarrhea, abdominal pain, and unintended weight loss. Its exact causes remain unclear but are believed to involve autoimmune responses, certain medications, or genetic predispositions.
If you’re experiencing symptoms consistent with microscopic colitis, it’s crucial to consult a healthcare professional. Early diagnosis and appropriate treatment can significantly improve your quality of life. Remember, managing your symptoms effectively begins with expert advice and tailored medical intervention.
References
For further reading and to validate the information provided on Microscopic Colitis symptoms, consider exploring the following reputable sources:
- Mayo Clinic: Detailed overview of symptoms, causes, and treatment options for Microscopic Colitis. Available at: Mayo Clinic – Microscopic Colitis
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Comprehensive information on diagnosis, management, and research on Microscopic Colitis. Visit: NIDDK – Microscopic Colitis
- PubMed Central: Access a range of scientific articles and studies on the pathogenesis and treatment of Microscopic Colitis. Read more at: PubMed Central – Microscopic Colitis
These sources are maintained by reputable medical and research institutions, ensuring that the information is accurate and up-to-date.