Metachromatic Leukodystrophy Symptoms: Metachromatic Leukodystrophy (MLD) is a rare genetic disorder that affects the body’s ability to produce healthy myelin, the protective sheath surrounding nerves.
This disease is part of a group of disorders known as leukodystrophies, which cause progressive deterioration of the central nervous system.
Understanding the symptoms and causes of MLD is crucial for early diagnosis and management.
What is Metachromatic Leukodystrophy?
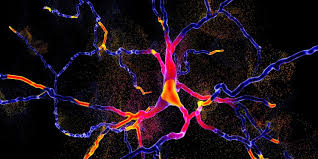
Metachromatic leukodystrophy (MLD) is a rare genetic disorder characterized by the accumulation of fats called sulfatides in cells, particularly affecting the nervous system. This accumulation leads to the progressive deterioration of intellectual and motor functions. The disease is caused by a deficiency of the enzyme arylsulfatase A, which is essential for breaking down sulfatides. As a result, these substances accumulate in various tissues, particularly in the white matter of the brain and spinal cord, leading to severe neurological symptoms.
Types of Metachromatic Leukodystrophy
Metachromatic leukodystrophy is classified into three main types based on the age of onset and progression of symptoms:
- Late Infantile MLD: This is the most common form, typically presenting symptoms between 12 and 24 months of age. Children with late infantile MLD may experience difficulty walking, muscle wasting, and a loss of motor skills, progressing to more severe neurological impairment.
- Juvenile MLD: Symptoms of juvenile MLD begin between the ages of 3 and 16 years. Early signs may include behavioral problems and poor school performance, followed by motor dysfunction and dementia.
- Adult MLD: The least common form, adult MLD, can start anytime in adulthood, sometimes as late as the 40s or 50s. It often manifests subtly with psychiatric symptoms or as progressive cognitive decline, making it difficult to diagnose initially.
Statistics on Prevalence and Demographics
Metachromatic leukodystrophy is a rare condition, affecting approximately 1 in 40,000 to 160,000 individuals worldwide. The disease does not have a predilection for any specific gender or ethnic group, appearing across various populations globally. However, certain genetic mutations linked to MLD may be more common in specific populations, which can affect the incidence rates in those groups.
Despite its rarity, the impact of MLD is profound, emphasizing the importance of genetic counseling and awareness to manage and potentially mitigate its effects in affected families.
Symptoms of Metachromatic Leukodystrophy
Here we explore the symptoms specific to different types of MLD, their progression, and how they vary across stages.
Early Symptoms Specific to Different Types
MLD is categorized into three main types based on the age of onset: late infantile, juvenile, and adult. Each type presents unique early symptoms:
- Late Infantile MLD: Symptoms typically appear between 12 and 18 months of age. Early signs include muscle weakness, difficulty walking, and a decrease in motor skills that had been previously acquired.
- Juvenile MLD: This type affects children between 4 and 12 years old. Early symptoms often involve behavioral changes, decline in school performance, and difficulty in understanding and processing information.
- Adult MLD: Onset occurs in teenage years or later. Early symptoms are usually psychiatric, such as personality changes, and may include physical symptoms like weakness and numbness in the extremities.
List of Symptoms in Late Infantile MLD
- Loss of muscle tone and coordination
- Difficulty walking or inability to walk
- Decreased intellectual function and learning difficulties
- Behavioral changes
- Seizures
List of Symptoms in Juvenile MLD
- Behavioral changes and mood swings
- Cognitive decline, particularly in problem-solving and spatial awareness
- Motor skills deterioration
- Vision problems and eventual blindness
- Seizures
List of Symptoms in Adult MLD
- Psychiatric symptoms such as delusions, depression, or bipolar disorder
- Progressive cognitive decline
- Motor neuropathy leading to difficulties in movement
- Impaired speech and communication
- Loss of bladder and bowel control
Progression of Symptoms
As MLD progresses, regardless of the onset type, patients experience a similar pattern of worsening symptoms:
Neurological Decline
- Cognitive Impairment: There is a gradual but significant loss of cognitive abilities, affecting memory, judgment, and reasoning.
- Sensory Loss: Patients may experience loss of sensation, particularly in the limbs, leading to difficulties in movement and coordination.
Physical Disabilities
- Mobility Issues: As the disease advances, muscle weakness intensifies, often leading to the need for wheelchair use.
- Communication Challenges: Speech becomes increasingly difficult, affecting the ability to communicate effectively.
Comparison of Symptoms Across Different Stages
- Early Stage: Symptoms are often subtle and vary significantly based on the type of MLD. In late infantile, symptoms are primarily physical, while in juvenile and adult types, cognitive and psychiatric symptoms are more pronounced.
- Mid Stage: Common symptoms across all types include motor dysfunction, cognitive decline, and worsening behavioral issues.
- Late Stage: Patients experience severe physical and neurological decline, including profound disabilities, communication difficulties, and complete dependency for care.
However, understanding the symptoms of MLD at different stages helps in managing the disease more effectively, allowing for better planning of care and support for affected individuals and their families.
Causes of Metachromatic Leukodystrophy
Understanding the causes of MLD involves exploring both its genetic basis and biochemical mechanisms.
Genetic Basis of MLD
MLD is primarily caused by mutations in the ARSA gene, which is crucial for the production of the enzyme arylsulfatase A. This enzyme plays a vital role in the breakdown of sulfatides, which are complex molecules found in the myelin sheath surrounding nerve cells. There are three main types of MLD, each linked to different patterns of inheritance and severity:
- Late Infantile MLD: The most common form, usually manifesting between ages 1 and 2. It is caused by severe mutations leading to very low or absent enzyme activity.
- Juvenile MLD: Occurs in children aged 4 to 12. These mutations often result in slightly higher enzyme activity compared to the late infantile form.
- Adult MLD: Manifests in adolescence or adulthood, typically due to mutations that allow low but better residual enzyme activity than in the more severe forms.
These mutations are autosomal recessive, meaning a child must inherit one defective gene from each parent to develop the disorder.
Biochemical Mechanisms
The biochemical pathway of MLD involves the disruption in the metabolism of sulfatides due to insufficient activity of arylsulfatase A. This disruption leads to several key biochemical changes:
- Accumulation of Sulfatides: Without adequate enzyme activity, sulfatides accumulate in various body tissues, primarily in the central and peripheral nervous systems. This accumulation disrupts the normal function of nerve cells.
- Demyelination: Accumulated sulfatides lead to the breakdown of the myelin sheath, the protective layer that surrounds nerve fibers. This demyelination impairs the transmission of nerve signals, leading to neurological symptoms.
- Neurological Impact: The progressive demyelination combined with the toxic buildup of sulfatides leads to a decline in motor skills, cognitive abilities, and eventually severe neurological dysfunction.
However, researchers continue to explore these mechanisms in hopes of finding effective therapies to halt or reverse the progression of the disease.
Diagnosing Metachromatic Leukodystrophy
Diagnosing MLD accurately is crucial for managing its progression and optimizing patient care. Here, we explore common diagnostic methods, the challenges in early diagnosis, and the importance of differential diagnosis.
Common Diagnostic Methods
- Genetic Testing: This involves analyzing the patient’s DNA to look for mutations in the ARSA gene, which are indicative of MLD. This method can confirm the diagnosis and help in family planning and genetic counseling.
- Enzyme Assay: Reduced activity of the enzyme arylsulfatase A (ARSA) in white blood cells or skin fibroblasts is a hallmark of MLD. Enzyme assays can determine the activity level of ARSA, aiding in diagnosis.
- MRI Scans: Magnetic resonance imaging (MRI) of the brain can show characteristic patterns that suggest demyelination, a key feature of MLD. These patterns help differentiate MLD from other demyelinating diseases.
- Nerve Conduction Studies: These studies measure how quickly nerves send electrical signals. A slowing of nerve conduction can indicate MLD, as the myelin sheath is damaged.
- Urine Sulfatide Levels: Elevated levels of sulfatides in urine are a potential indicator of MLD. This test can support findings from other diagnostic methods.
Challenges in Early Diagnosis
- Symptom Overlap: Early symptoms of MLD, such as behavioral changes and motor skill regression, are often nonspecific and can overlap with more common conditions like ADHD or autism, leading to misdiagnosis.
- Lack of Awareness: Due to its rarity, there is a general lack of awareness about MLD among healthcare professionals, which can delay consideration of MLD as a potential diagnosis.
- Variable Onset: The age of onset varies widely in MLD, from infancy to adulthood, complicating the diagnostic process as symptoms differ significantly across age groups.
- Access to Testing: Genetic testing and specialized enzyme assays may not be readily available in all regions or could be cost-prohibitive, further delaying diagnosis.
Importance of Differential Diagnosis
- Tailoring Treatment: Effective management strategies can be significantly influenced by the specific type of leukodystrophy diagnosed. Differential diagnosis ensures that treatment is appropriately tailored to MLD rather than another similar condition.
- Avoiding Unnecessary Treatments: Accurate diagnosis prevents the application of unnecessary and potentially harmful treatments intended for other diseases with similar symptoms.
- Prognostic Planning: Understanding whether a patient has MLD or another form of leukodystrophy impacts long-term care and prognostic planning, including family genetic counseling and future healthcare needs.
However, advancements in medical technology and increased awareness among healthcare providers can help overcome challenges in the early detection of this debilitating disease.
Impact of Metachromatic Leukodystrophy on Patients and Families
Metachromatic leukodystrophy (MLD) is a rare genetic disorder that significantly impacts the lives of patients and their families. Understanding the broad range of challenges they face is crucial for providing comprehensive support.
Physical and Emotional Challenges
Physical Challenges: MLD primarily affects the nervous system, leading to a progressive loss of motor skills, coordination, and mobility. Patients may experience difficulty in walking, talking, and completing daily activities independently. As the disease progresses, it can lead to more severe disabilities, including paralysis.
Emotional Challenges: The physical decline in health often brings significant emotional distress for both patients and their families. Patients might suffer from anxiety, depression, and frustration due to their increasing dependency and loss of function. Family members often experience emotional strain from watching their loved ones deteriorate and from the demanding nature of caregiving.
Financial and Social Implications
Financial Implications: The cost of managing MLD can be substantial. Medical expenses include diagnostic tests, treatment modalities, and ongoing care needs, which may not be fully covered by insurance. Additionally, the need for specialized care might necessitate home modifications or hiring of professional caregivers, adding to the financial strain.
Social Implications: Families often face social isolation due to the demanding care routines or the stigma associated with disability. Patients might withdraw from social interactions as their condition worsens, which can lead to a diminished support network for both the patients and their caregivers.
Role of Support Groups and Resources
Support groups play a critical role in helping families navigate the complexities of MLD. These groups provide a platform for sharing experiences, emotional support, and practical advice. They can also be a vital resource for accessing information about the latest treatments and research, as well as guidance on managing the financial and legal aspects of care.
Resources: Various organizations offer resources tailored to the needs of families dealing with MLD. These might include educational materials, access to medical experts, equipment lending programs, and respite care services. Engaging with these resources can significantly alleviate the burdens faced by patients and families, providing them with tools to manage their situation more effectively.
By focusing on both the challenges and available support, stakeholders can foster a more supportive and informed community around this debilitating condition.
FAQs about Metachromatic Leukodystrophy Symptoms
What is Metachromatic Leukodystrophy?
Metachromatic leukodystrophy (MLD) is a rare genetic disorder that affects the body’s ability to produce healthy myelin, the protective coating around nerve cells. This leads to progressive deterioration of nerve function.
What are the first symptoms of MLD?
The initial symptoms of MLD can vary but commonly include muscle weakness, difficulty walking, and a decrease in intellectual capabilities. In young children, symptoms may also manifest as behavioral changes and regression in motor skills.
How does MLD progress over time?
As MLD progresses, symptoms typically worsen. This can lead to severe complications such as loss of mobility, difficulty communicating, and more profound cognitive decline. The rate of progression can vary depending on the form of MLD, with some forms progressing more rapidly than others.
Are there different types of MLD?
Yes, MLD is categorized into three main types based on the age of onset: late infantile, juvenile, and adult. Each type has distinct symptoms and progression rates.
Can MLD be treated?
While there is no cure for MLD, treatment options focus on managing symptoms and improving quality of life. This can include physical therapy, medications to manage pain and seizures, and in some cases, stem cell transplantation, which may help slow the disease’s progression in certain individuals.
Is genetic testing available for MLD?
Genetic testing is available and recommended for families with a history of MLD. It can help identify carriers of the disease and aid in early diagnosis, which is crucial for managing the disease effectively.
Conclusion
In summary, Metachromatic Leukodystrophy (MLD) is a rare genetic disorder that significantly impacts the nervous system, leading to severe neurological problems. The symptoms vary but typically include muscle weakness, difficulty walking, and progressive loss of cognitive functions, manifesting due to the accumulation of sulfatides in the body, which damage the white matter in the brain and peripheral nerves.
Addressing MLD effectively requires enhanced research efforts and increased public awareness. There is a critical need for more comprehensive studies to develop advanced treatments and potentially find a cure. Raising awareness can facilitate early diagnosis, which is crucial for managing the condition more effectively.
If you or someone you know is experiencing symptoms related to MLD, it is essential to consult healthcare professionals who specialize in genetic disorders. Early intervention and professional guidance are key to managing the symptoms and improving the quality of life for those affected by this challenging condition. Let us all advocate for more research and spread the word to ensure that MLD receives the attention it deserves.
References
For additional information and validation of the symptoms associated with Metachromatic Leukodystrophy, the following resources are highly recommended:
- National Institute of Neurological Disorders and Stroke (NINDS) – Provides a comprehensive overview of Metachromatic Leukodystrophy, detailing symptoms, causes, and treatment options. Read more about Metachromatic Leukodystrophy on NINDS.
- Genetics Home Reference (MedlinePlus) – Offers detailed genetic information and an explanation of how Metachromatic Leukodystrophy is inherited. This resource includes symptoms and long-term management strategies. Explore Metachromatic Leukodystrophy on MedlinePlus.
- Mayo Clinic – Features a user-friendly guide on the diagnosis and treatment of Metachromatic Leukodystrophy, alongside real patient stories that illustrate the personal impact of the disease. Visit Mayo Clinic for more information.
- Orphanet Journal of Rare Diseases – Contains peer-reviewed research articles that delve into the complexities of Metachromatic Leukodystrophy, offering insights into recent scientific advancements and ongoing research. Read the latest research on Orphanet.
These resources provide credible and detailed information that will help deepen your understanding of Metachromatic Leukodystrophy and assist in further exploration of the disease’s symptoms and treatment options.