Metachromatic Leukodystrophy Treatment: Metachromatic Leukodystrophy (MLD) is a rare genetic disorder that primarily affects the nervous system.
This article provides a comprehensive overview of the diagnosis and treatment options for MLD, aiming to be a vital resource for patients, families, and healthcare providers.
Understanding Metachromatic Leukodystrophy
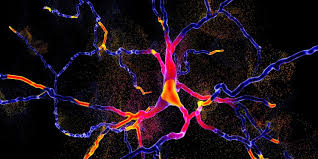
Metachromatic leukodystrophy (MLD) is a rare genetic disorder that affects the nervous system. It primarily impacts the metabolism of sphingolipids, which are fats that are essential components of cell membranes in the brain and other parts of the body. The disorder results from the accumulation of sulfatides, leading to progressive damage in the white matter of the central nervous system. This damage impairs the functioning of nerves, leading to severe physical and cognitive decline over time.
Types of Metachromatic Leukodystrophy
MLD is classified into three main types based on the age of onset and the progression of symptoms:
- Late Infantile MLD: The most common form, it typically begins between 12 and 18 months of age. Symptoms include muscle weakness, motor skill regression, and severe coordination problems.
- Juvenile MLD: This type manifests between the ages of 4 and 12. Children may experience behavioral problems, declining school performance, and difficulty walking.
- Adult MLD: Also known as late-onset MLD, it can start anytime from adolescence to the 40s or later. Initial symptoms often include psychiatric issues and motor disturbances.
Epidemiology: Prevalence and Demographics
Metachromatic leukodystrophy is estimated to occur in 1 in 40,000 to 160,000 live births worldwide. However, the incidence can vary significantly between populations due to genetic factors. For example, certain subgroups in Israel and the Navajo population in the United States exhibit a higher prevalence of MLD. The disorder affects both males and females equally and does not show a preference for any specific ethnic group.
Genetic Causes and Risk Factors
The primary cause of metachromatic leukodystrophy is mutations in the ARSA gene, which is responsible for producing the enzyme arylsulfatase A. This enzyme is crucial for breaking down sulfatides. Without functional arylsulfatase A, sulfatides accumulate in cells, particularly in the nervous system, leading to the symptoms of MLD.
Risk factors include:
- Genetic Inheritance: MLD is inherited in an autosomal recessive pattern, meaning that a child must inherit two copies of the mutated gene, one from each parent, to develop the disorder.
- Family History: Having parents or siblings with MLD increases the risk of inheriting the defective genes.
However, advances in genetic testing and therapies are providing some hope for affected families, although there is currently no cure for MLD.
Symptoms and Progression of Metachromatic Leukodystrophy
Understanding the symptoms and how MLD progresses can help in managing the disease more effectively.
Early Symptoms and Signs
The onset of metachromatic leukodystrophy varies by the form of the disease (late infantile, juvenile, or adult), but there are common early signs across these types:
- Motor Skills Decline: Difficulty in coordination and motor skills, such as walking or grasping objects, is often one of the first signs.
- Behavioral Changes: Affected individuals may exhibit irritability, withdrawal, and a decrease in performance at school or work.
- Muscle Weakness: There may be a noticeable decrease in muscle tone and strength.
- Nerve Sensitivity: Loss of sensation in the arms and legs, leading to difficulties in balance and movement.
Stages of Disease Progression
- Initial Neurological Symptoms: As mentioned, initial signs involve motor and behavioral changes. These symptoms gradually worsen.
- Advancement in Neurological Damage: Over time, the disease affects speech, vision, and mental abilities. Seizures may also occur.
- Severe Debilitation: In the late stages, individuals lose the ability to walk and communicate effectively. They become completely dependent on caregivers for daily activities.
- Life-Threatening Complications: In its final stages, MLD can lead to more severe complications, such as complete paralysis and unresponsiveness.
Impact on Quality of Life
MLD significantly impacts the quality of life not only for those affected but also for their families and caregivers:
- Physical Limitations: Progressive loss of motor functions and sensitivity impair the ability to perform daily tasks independently.
- Cognitive Decline: Memory, thinking, and reasoning skills deteriorate, which affects interpersonal interactions and personal independence.
- Emotional and Social Effects: The emotional burden of MLD can lead to social isolation and depression in patients and stress and anxiety in family members.
- Care Requirements: As the disease progresses, the need for comprehensive medical and supportive care increases, often involving specialized healthcare services and home adjustments.
However, understanding these aspects of metachromatic leukodystrophy is crucial for timely intervention and support, enhancing the life quality of affected individuals and their families.
Diagnostic Approaches of Metachromatic Leukodystrophy
Proper diagnosis is crucial for management and care planning. Here, we explore the diagnostic approaches for MLD, focusing on clinical assessments, key diagnostic tests, and differential diagnosis.
Clinical Assessment and Medical History
The initial step in diagnosing MLD involves a thorough clinical evaluation and detailed medical history. Key aspects include:
- Neurological Examination: Assessing motor skills, coordination, muscle strength, and reflexes to identify any neurological deficits.
- Developmental Milestones: Reviewing the patient’s developmental history to identify any delays or regression in skills.
- Family History: Gathering information about any family members who may have had similar symptoms or diagnosed neurological disorders, as MLD is inherited.
Key Diagnostic Tests
To confirm a diagnosis of MLD, several diagnostic tests are typically employed:
- MRI Scan: Magnetic resonance imaging (MRI) can show changes in white matter that are indicative of leukodystrophy.
- Genetic Testing: Identifying mutations in the ARSA gene, which are responsible for most cases of MLD.
- Nerve Conduction Studies: Measuring the speed and strength of electrical signals in nerves to detect impairments.
- Enzyme Assay: A critical test that measures the activity of the enzyme arylsulfatase A in white blood cells or skin fibroblasts. Reduced or absent enzyme activity confirms MLD.
Differential Diagnosis: Distinguishing MLD from Similar Disorders
Differential diagnosis is essential to distinguish MLD from other disorders with similar symptoms, such as:
- Krabbe Disease: Like MLD, it affects the white matter of the brain, but it is caused by a deficiency in a different enzyme (galactocerebrosidase).
- Multiple Sclerosis (MS): MS can also lead to similar neurological and MRI findings but typically occurs in adults and follows a different progression pattern.
- Adrenoleukodystrophy (ALD): Although similar in its effects on the nervous system and adrenal glands, ALD has distinct genetic markers and enzyme assay results compared to MLD.
However, diagnosing metachromatic leukodystrophy involves a combination of clinical evaluation, specific diagnostic tests, and careful differential diagnosis to ensure accuracy and appropriate management.
Current Treatments for Metachromatic Leukodystrophy
Metachromatic leukodystrophy (MLD) is a rare genetic disorder that affects the nervous system. Despite ongoing research, there is currently no cure for MLD, but several treatment options aim to manage symptoms and improve quality of life. Here, we explore the goals of available treatments, the methods employed, and the promising developments in gene therapy.
Goals of Available Treatments
The primary goals of treating metachromatic leukodystrophy include:
- Alleviating Symptoms: Managing the neurological symptoms to improve the patient’s quality of life.
- Slowing Disease Progression: Attempting to slow the deterioration of physical and mental functions.
- Supportive Care: Providing therapies that help manage day-to-day difficulties and complications associated with MLD.
- Enhancing Life Quality: Ensuring the patient’s environment and care routines are optimized to make living with MLD as comfortable as possible.
Methods of Treatments for Metachromatic Leukodystrophy
Treatment approaches for MLD vary depending on the severity and progression of the disease and may include:
- Enzyme Replacement Therapy (ERT): Although still under research for MLD, ERT has shown promise in managing similar lysosomal storage disorders by replacing the deficient enzyme.
- Bone Marrow Transplant (BMT): This procedure can be effective, especially in early stages of the disease, by providing healthy cells capable of producing the enzyme that MLD patients lack.
- Stem Cell Transplantation: Similar to BMT, this method involves replacing the diseased cells with healthy stem cells, potentially halting disease progression.
- Symptomatic Treatments: These include physical therapy, occupational therapy, and medications to manage pain and muscle spasms.
Gene Therapy: Recent Advances and Future Prospects
Gene therapy represents a frontier in the treatment of genetic disorders like MLD. Recent advances include:
- Development of Targeted Gene Therapies: Researchers are working on therapies that introduce a correct copy of the defective gene responsible for MLD. This approach aims to restore the normal function of the enzyme.
- Clinical Trials: Several ongoing clinical trials are testing the safety and efficacy of gene therapies in treating MLD. Early results are promising, showing potential for significant slowing of disease progression.
- Future Prospects: Scientists are optimistic about refining gene therapy techniques to increase their effectiveness and safety. The goal is to develop a definitive cure that can be widely accessible to all MLD patients.
However, while current treatments focus on management and symptom relief, the future holds potential for curative therapies through innovative approaches like gene therapy.
Supportive Care and Management of Metachromatic Leukodystrophy
Effective management of MLD requires a comprehensive approach focusing on supportive care to enhance the quality of life for patients and their families. Here, we detail essential aspects of supportive care including physical therapy, nutritional support, and psychological assistance.
Physical Therapy and Mobility Aids
- Routine Physical Therapy: Engaging in regular physical therapy is crucial for maintaining muscle strength and flexibility. Therapists can tailor exercises to the patient’s capabilities, focusing on gentle stretches and low-impact activities that help manage spasticity and muscle degeneration.
- Mobility Aids: As mobility becomes a challenge, the use of aids such as wheelchairs, walkers, and orthotic devices can provide independence and improve quality of life. Customized seating and positioning aids also help in maintaining comfort and preventing skin breakdown.
Nutritional Support and Management of Complications
- Dietary Adjustments: A well-balanced diet tailored to the patient’s specific needs is vital. Nutritional plans may include high-calorie formulas or supplements to prevent weight loss and support overall health.
- Feeding Assistance: With the progression of MLD, patients might experience difficulties in swallowing. The use of feeding tubes may become necessary to ensure adequate nutrition and hydration, thus preventing aspiration and other complications.
- Management of Gastrointestinal Issues: Common issues such as constipation or gastroesophageal reflux disease (GERD) require proactive management. A healthcare provider might recommend medications or dietary adjustments to alleviate these symptoms.
Psychological Support for Patients and Families
- Counseling Services: Psychological counseling for patients and their families is essential. It helps in coping with the emotional and mental stress of living with a chronic, progressive illness.
- Support Groups: Participating in support groups can provide emotional solace and practical advice, connecting patients and families with others who face similar challenges.
- Education and Resources: Providing families with educational resources about MLD and its management can empower them to make informed decisions regarding care and support.
By addressing these key areas, it’s possible to enhance the well-being and quality of life for those affected by metachromatic leukodystrophy.
Research and Future Directions in Metachromatic Leukodystrophy Treatment
Recent advancements in clinical trials for Metachromatic Leukodystrophy (MLD) spotlight innovative approaches aimed at altering the course of this genetic disorder. Current trials primarily focus on gene therapy, which holds promise for correcting the underlying genetic defects responsible for MLD. Additionally, enzyme replacement therapies are being tested to see if they can provide a functional enzyme to those lacking it, potentially reducing the accumulation of sulfatides in the nervous system. Stem cell transplantation is another area of intense research, exploring its efficacy in providing enzyme-producing cells to patients.
Emerging Therapies and Innovations
The landscape of MLD treatment is evolving with several exciting therapies on the horizon:
- Gene Therapy: Techniques such as using viral vectors to deliver functional copies of the ARSA gene directly into patient cells.
- Enzyme Replacement Therapy (ERT): Developments in biotechnology have led to more stable enzyme formulations that can be administered directly to patients, aiming to replace the missing or malfunctioning enzyme.
- Combination Therapies: Researchers are investigating the synergy between pharmacological chaperones and substrate reduction therapies, which could enhance enzyme functionality and reduce toxic metabolite buildup respectively.
- Advanced Stem Cell Transplantation: Innovations in stem cell therapy include genetically modifying the patient’s own cells to correct the genetic defect before reinfusion.
The Role of Patient Registries in Advancing Research
Patient registries are crucial in MLD research, serving multiple vital functions:
- Data Collection: Registries gather comprehensive data on patient demographics, treatment outcomes, and progression of MLD, providing a wealth of information for researchers.
- Enhancing Clinical Trials: By identifying suitable candidates for clinical trials quickly, registries help in accelerating the pace of research.
- Long-term Monitoring: Registries facilitate the long-term monitoring of patients, crucial for assessing the lifelong efficacy and safety of new treatments.
- Global Collaboration: They enable researchers from different regions to collaborate, share findings, and standardize care protocols across borders, which is essential for rare diseases like MLD.
However, the ongoing research and patient-centered innovations continue to push the boundaries of what’s possible in treating Metachromatic Leukodystrophy, offering hope for effective management and improved quality of life for affected individuals.
FAQs about Metachromatic Leukodystrophy Treatment
What is Metachromatic Leukodystrophy (MLD)?
Metachromatic Leukodystrophy (MLD) is a rare genetic disorder affecting the metabolism of sphingolipids, fats crucial to the function of nerve cells in the brain. It results in the accumulation of these fats, leading to the progressive deterioration of motor skills, cognition, and function.
How is MLD treated?
Currently, there is no cure for MLD, but treatments focus on managing symptoms and improving quality of life. Options may include gene therapy, bone marrow transplant, enzyme replacement therapy, and supportive care to manage symptoms and complications.
Who can undergo gene therapy for MLD?
Gene therapy for MLD is still experimental and typically offered through clinical trials. Eligibility depends on various factors, including the stage of the disease, specific genetic mutations, and overall health of the patient.
What is the role of a bone marrow transplant in treating MLD?
A bone marrow transplant can potentially slow or halt the progression of MLD in some patients, especially if performed early in the disease’s course. It involves replacing the defective cells that produce enzymes with healthy ones from a donor.
Is physical therapy beneficial for MLD patients?
Yes, physical therapy is crucial for maintaining mobility and function in MLD patients. It helps manage spasticity and mobility issues, providing patients with better quality of life and potentially delaying the progression of physical symptoms.
Are there any new treatments on the horizon for MLD?
Researchers are continuously exploring new treatments, including advanced gene therapies and enzyme therapies that target the underlying causes of MLD. Participation in clinical trials can provide access to cutting-edge therapies not yet widely available.
Where can patients and families find support and resources?
Support for MLD can be found through specialized healthcare providers, genetic counselors, and organizations dedicated to leukodystrophy. These resources offer support groups, educational materials, and assistance in managing the financial aspects of care.
Conclusion
In summary, metachromatic leukodystrophy (MLD) treatment currently revolves around symptom management, supportive care, and emerging therapies such as gene therapy and stem cell transplantation. While there are significant challenges in treating this disorder, the ongoing research and clinical trials offer a beacon of hope.
Advancements in genetic understanding and therapeutic techniques continue to unfold, bringing us closer to more effective treatments. It is crucial for the medical community and researchers to persist in their efforts, as every small breakthrough can potentially lead to substantial improvements in the lives of those affected by MLD.
The future holds promise, and with continued support and investment in research, we can aspire to not only extend life expectancy but also enhance the quality of life for individuals with metachromatic leukodystrophy.
References
For further reading and validation of the information provided on treatments for Metachromatic Leukodystrophy, the following sources are highly recommended:
- National Institute of Neurological Disorders and Stroke (NINDS) – This site offers a comprehensive overview of Metachromatic Leukodystrophy, detailing symptoms, causes, treatment options, and ongoing research. Visit NINDS for more information.
- Mayo Clinic – Known for its credible and thorough medical content, Mayo Clinic provides an insightful article on the diagnosis, treatment, and management of Metachromatic Leukodystrophy. Read the Mayo Clinic article.
- Genetics Home Reference – U.S. National Library of Medicine – Here you can find genetic information and an explanation of how Metachromatic Leukodystrophy is inherited, as well as details on genetic counseling. Explore Genetics Home Reference.
- PubMed Central – A valuable resource for scientific articles offering in-depth research studies and clinical trial results related to Metachromatic Leukodystrophy treatments. Search PubMed Central.
- Orphanet – Orphanet provides a portal to services for rare diseases, including extensive resources on Metachromatic Leukodystrophy. Their reports cover epidemiology, diagnosis protocols, and treatment avenues. Visit Orphanet.
These sources are reputable within the medical community and provide a solid foundation for understanding the complex nature of Metachromatic Leukodystrophy and the current approaches to its treatment.