Mesenteric Ischemia Treatment: Mesenteric ischemia, a critical condition characterized by inadequate blood flow to the intestines, can lead to severe complications if not promptly diagnosed and treated.
Understanding the intricacies of this medical emergency is essential for timely intervention and effective management.
Understanding Mesenteric Ischemia
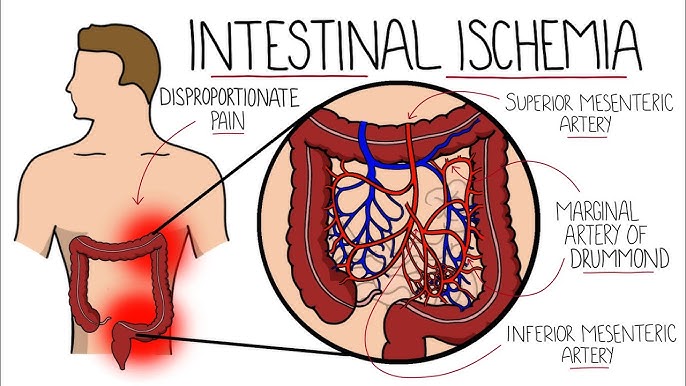
Mesenteric ischemia is a medical condition characterized by a reduction in blood flow to the small intestine, which can lead to severe abdominal pain and other digestive issues. Understanding the types, causes, and risk factors associated with mesenteric ischemia is essential for early diagnosis and effective treatment.
Types of Mesenteric Ischemia
Mesenteric ischemia can be categorized into four primary types, each with its distinct characteristics and underlying mechanisms:
- Acute Mesenteric Ischemia (AMI): This is a sudden onset condition that occurs due to a blockage in the blood flow to the intestines. It is a medical emergency requiring immediate attention.
- Chronic Mesenteric Ischemia (CMI): Developing gradually over time, CMI results from progressively diminished blood flow caused by atherosclerosis or other slow-developing conditions.
- Mesenteric Venous Thrombosis (MVT): This type involves a clot in the mesenteric veins, which impedes the outflow of blood from the intestines, leading to congestion and ischemia.
- Nonocclusive Mesenteric Ischemia (NOMI): Common in patients with low blood flow states, NOMI occurs without a physical blockage in the mesenteric arteries but is due to reduced blood flow caused by other systemic conditions.
Causes and Risk Factors Contributing to Mesenteric Ischemia
Several causes and risk factors can contribute to the development of mesenteric ischemia, varying by the type of ischemia:
- Atherosclerosis: The most common cause of chronic mesenteric ischemia, where plaque builds up in the arteries, leading to reduced blood flow.
- Blood Clots: Acute mesenteric ischemia is often caused by emboli or thrombi that block the mesenteric arteries.
- Heart Conditions: Conditions such as heart failure, arrhythmias, or recent myocardial infarction can increase the risk of clots that lead to mesenteric ischemia.
- Cancer and Inflammatory Disorders: These can increase the risk of venous thrombosis, including in the mesenteric veins.
- Surgical Procedures: Surgeries involving the heart or blood vessels can sometimes lead to mesenteric ischemia as a complication.
- Medications: Certain medications, like diuretics or digitalis, can decrease blood flow to the intestines, increasing the risk of nonocclusive mesenteric ischemia.
However, early recognition and treatment are key to managing mesenteric ischemia effectively, improving outcomes and quality of life for those affected.
Signs and Symptoms of Mesenteric Ischemia
Here we break down the common symptoms associated with both acute and chronic mesenteric ischemia, and explain how these symptoms can differ between the types and progress over time.
Common Symptoms of Acute Mesenteric Ischemia
Acute mesenteric ischemia occurs suddenly and is often severe. The common symptoms include:
- Sudden, severe abdominal pain: The pain may not correspond with the severity of the condition, making it a critical diagnostic challenge.
- Nausea and vomiting: These symptoms can accompany the abdominal pain.
- Diarrhea: This may occur and can sometimes contain blood.
- Urgent need to defecate: A sudden and intense urge to have a bowel movement.
- Rapid heartbeat: Increased heart rate is a common response to the pain and stress of the condition.
Common Symptoms of Chronic Mesenteric Ischemia
Chronic mesenteric ischemia develops gradually over time and its symptoms are often less intense initially but can become more severe as the condition progresses. The symptoms include:
- Abdominal pain after eating: Known as “food fear” due to pain post-meal, which can lead to weight loss.
- Weight loss: Often unintentional, due to reduced food intake from the pain or fear of pain after eating.
- Bloating or a feeling of fullness: This can occur, especially after meals.
- Changes in bowel habits: Including diarrhea or constipation.
Differences and Progression Over Time
The progression and differentiation of symptoms between acute and chronic mesenteric ischemia are key to diagnosis:
- Onset of Symptoms: Acute mesenteric ischemia presents suddenly and with severe symptoms, whereas chronic mesenteric ischemia starts gradually, with symptoms intensifying over time.
- Nature of Abdominal Pain: In acute cases, the abdominal pain is sharp and severe without a clear trigger. In chronic cases, the pain typically occurs after eating and may progressively worsen as the disease advances.
- Associated Symptoms: While both types may present with nausea and changes in bowel habits, the urgency and severity of these symptoms are typically greater in acute cases.
However, early recognition and medical intervention can significantly impact the prognosis of both acute and chronic forms of this condition.
Diagnostic Approaches to Mesenteric Ischemia
Understanding the diagnostic pathways for mesenteric ischemia is crucial due to its potentially life-threatening nature. This condition, where blood flow to the small intestine is restricted, requires prompt and accurate diagnosis. Below, we explore the key diagnostic steps including initial assessment, imaging tests, and the role of angiography.
Initial Assessment and Medical History Evaluation
The first step in diagnosing mesenteric ischemia involves a thorough initial assessment and evaluation of the patient’s medical history. Key aspects include:
- Symptom Assessment: Identifying acute or chronic symptoms such as sudden abdominal pain, nausea, vomiting, or a fear of eating due to pain which might suggest a compromise in intestinal blood flow.
- Medical History Review: Checking for risk factors such as atrial fibrillation, recent myocardial infarction, or a history of vascular disease which can predispose an individual to mesenteric ischemia.
- Physical Examination: Conducting a detailed abdominal examination to check for any signs of tenderness, distension, or peritoneal irritation which might indicate ischemic changes.
Imaging Tests Used in the Diagnosis of Mesenteric Ischemia
Imaging studies play a pivotal role in confirming the diagnosis of mesenteric ischemia. The most commonly used imaging tests include:
- Computed Tomography (CT) Scan: A CT angiogram is particularly valuable as it provides detailed images of both blood vessels and intestinal structures, helping to identify blockages or other abnormalities.
- Ultrasound: Doppler ultrasound can be used to assess blood flow in the mesenteric arteries and veins, although it may be limited by bowel gas and patient body habitus.
- Magnetic Resonance Imaging (MRI): MRI can offer high-resolution images of soft tissues and blood vessels, useful in chronic cases where other modalities might be inconclusive.
Role of Angiography in Diagnosing Mesenteric Ischemia
Angiography remains a gold standard for the definitive diagnosis of mesenteric ischemia. This procedure involves:
- Visualizing Blood Flow: Angiography allows for direct visualization of the blood flow in the mesenteric arteries, clearly outlining any occlusions or narrowing.
- Interventional Options: During an angiography, therapeutic procedures like balloon angioplasty or stent placement can be performed if a significant stenosis or blockage is identified.
- Diagnostic Precision: It provides precise details that are often not visible with non-invasive imaging techniques, making it crucial for planning subsequent management strategies.
However, through a combination of medical history evaluation, targeted imaging tests, and detailed angiography, healthcare providers can effectively diagnose and manage mesenteric ischemia, potentially saving lives by preventing severe intestinal damage.
Treatment Strategies for Mesenteric Ischemia
Understanding the treatment modalities for both acute and chronic forms, including surgical interventions and medications, is crucial for effective management and improved patient outcomes.
Treatment Modalities for Acute versus Chronic Mesenteric Ischemia
Acute Mesenteric Ischemia (AMI):
- Immediate Revascularization: Essential to restore blood flow and prevent bowel necrosis. Techniques include surgical embolectomy, thrombectomy, and angioplasty with or without stenting.
- Anticoagulation Therapy: Administered to prevent further clot formation. Common agents include heparin, which is often used initially, followed by long-term anticoagulants like warfarin.
- Supportive Care: Includes fluid resuscitation, electrolyte management, and bowel rest.
Chronic Mesenteric Ischemia (CMI):
- Angioplasty and Stenting: Preferred for patients with significant stenosis or blockages in the mesenteric arteries. This less invasive approach can effectively relieve symptoms and restore blood flow.
- Surgical Revascularization: Bypass surgery may be considered for cases where angioplasty is not feasible or effective. It involves creating a new route for blood flow using a graft.
- Dietary Management: Adjustments in diet and meal frequency can help reduce symptoms by minimizing the intestines’ workload.
Surgical Interventions and Their Outcomes
Surgical treatment options vary based on the severity and progression of the disease:
- Embolectomy and Thrombectomy: These are critical for AMI to quickly remove blockages. Successful outcomes largely depend on the rapidity of intervention.
- Bypass Surgery: In CMI, bypass surgery can significantly improve quality of life and is generally successful, particularly when performed before irreversible intestinal damage occurs.
- Endarterectomy: Removal of the diseased portion of the artery can be effective in certain cases, restoring normal blood flow and alleviating symptoms.
Surgical outcomes are influenced by the timeliness of the diagnosis and the general health of the patient, with early intervention correlating with better results.
Medications and Their Role in Treatment
Medications play a supportive role in both acute and chronic mesenteric ischemia:
- Anticoagulants: Used in both AMI and CMI to prevent new clots and the growth of existing clots. Warfarin and newer oral anticoagulants are commonly prescribed.
- Vasodilators: These medications can help increase blood flow by widening blood vessels. However, their use must be carefully monitored.
- Pain Management: Chronic pain associated with CMI may require treatment with analgesics or antispasmodic medications to improve quality of life.
- Antibiotics: In cases of AMI leading to bowel necrosis, antibiotics are critical to prevent or treat sepsis.
However, each treatment strategy is tailored to the individual patient’s condition and the specific characteristics of their disease, making a multidisciplinary approach essential for optimal care and improved outcomes.
Recent Advances in Mesenteric Ischemia Treatment
Innovations in minimally invasive surgeries, new medications, and interdisciplinary treatment approaches have all contributed to improved patient outcomes. This section explores these recent developments, ensuring that healthcare professionals stay informed about the latest options for managing this life-threatening condition.
Innovations in Minimally Invasive Surgeries
Minimally invasive surgeries have revolutionized the treatment of mesenteric ischemia, offering less traumatic options with faster recovery times. Key innovations include:
- Endovascular Surgery: This technique involves the use of catheters and stents to open blocked arteries, significantly reducing the need for open surgery.
- Balloon Angioplasty: Often performed alongside stenting, this procedure dilates narrowed arteries, improving blood flow with minimal incisions.
- Laparoscopic Bypass Procedures: Surgeons can now perform bypass surgeries laparoscopically, redirecting blood flow around blocked arteries with only small abdominal incisions.
These techniques not only reduce hospital stays and recovery times but also diminish the risks associated with more invasive procedures.
New Medications and Their Clinical Trial Results
Recent pharmaceutical developments have also provided new hope in the treatment of mesenteric ischemia. Some notable advancements include:
- Vasodilators: New formulations have been tested in clinical trials, showing potential in increasing blood flow to the intestines by expanding blood vessels.
- Anticoagulants: Improved anticoagulant drugs help prevent the formation of new clots while minimizing the risk of bleeding, a common side effect in older treatments.
- Direct Oral Anticoagulants (DOACs): These have shown promise in phase III clinical trials for their efficacy and reduced side effects compared to traditional therapies.
The introduction of these medications offers practitioners more tools to tailor treatments based on individual patient needs and conditions.
Importance of Interdisciplinary Treatment Approaches
Interdisciplinary treatment approaches have become crucial in managing mesenteric ischemia effectively. These approaches typically involve:
- Collaboration between Vascular Surgeons and Gastroenterologists: This ensures that all aspects of the disease, from blood flow to intestinal health, are addressed.
- Nutritional Support Teams: Dieticians play a vital role in managing patients’ dietary needs to support intestinal health and recovery.
- Pain Management Specialists: They are essential in providing relief and improving the quality of life for patients during recovery.
However, this holistic approach not only enhances the effectiveness of the treatment but also supports the patient’s overall well-being and recovery process.
Prevention and Management of Mesenteric Ischemia Treatment
The effective management of mesenteric ischemia, a severe condition affecting the blood flow to the intestines, often hinges on adopting specific lifestyle changes and dietary modifications. Here are key strategies:
- Increase Fiber Intake: Incorporate a variety of fiber-rich foods such as fruits, vegetables, and whole grains. Fiber helps in improving digestion and maintaining a healthy weight, which can reduce pressure on the arteries.
- Stay Hydrated: Adequate hydration is vital. Drinking sufficient water daily helps improve blood flow and digestion, aiding in the prevention of vascular issues that can lead to mesenteric ischemia.
- Limit Fats and Cholesterol: High-fat diets can exacerbate the buildup of plaques in arteries, including those supplying the intestines. Opt for lean proteins, and reduce intake of saturated fats and cholesterol to help keep arteries clear.
- Moderate Exercise: Regular physical activity can improve cardiovascular health and promote good circulation. However, individuals should consult their healthcare provider for tailored exercise recommendations, especially if they have underlying health conditions.
- Avoid Smoking: Smoking is a significant risk factor for vascular diseases as it contributes to arterial constriction and stiffness. Quitting smoking can markedly improve overall vascular health.
- Control Blood Sugar: For individuals with diabetes, maintaining controlled blood sugar levels is crucial. High blood sugar can damage blood vessels, worsening mesenteric ischemia.
Monitoring and Management Strategies for At-Risk Individuals
For individuals at risk of mesenteric ischemia, proactive monitoring and management are essential to prevent the progression of the disease:
- Regular Check-Ups: Regular visits to a healthcare provider for blood tests and physical exams can help catch signs of vascular issues early.
- Monitoring Blood Pressure: Keeping blood pressure within recommended levels is crucial for preventing damage to blood vessels that could exacerbate mesenteric ischemia.
- Cholesterol Management: Regular monitoring of cholesterol and triglyceride levels with medication or diet adjustments as needed can help in managing risks associated with mesenteric ischemia.
- Watch for Warning Signs: Awareness of symptoms such as sudden abdominal pain, bloating, bloody stool, or changes in bowel habits is crucial. Prompt reporting of these signs to a healthcare provider can lead to early diagnosis and treatment.
- Stress Management: Chronic stress can affect the body’s ability to regulate inflammation and heal, impacting vascular health. Engaging in stress-reducing activities such as yoga, meditation, or deep breathing exercises can be beneficial.
- Medication Compliance: For those prescribed medication to manage risk factors such as hypertension or high cholesterol, adherence to treatment is essential for preventing complications related to mesenteric ischemia.
Implementing these lifestyle changes and monitoring strategies can significantly contribute to the prevention and management of mesenteric ischemia, enhancing both quality of life and health outcomes.
FAQs about Mesenteric Ischemia Treatment
What is mesenteric ischemia?
Mesenteric ischemia occurs when blood flow to the small intestine is restricted, potentially leading to tissue damage or death. It can be acute or chronic, with each type requiring different treatment approaches.
What are the symptoms of mesenteric ischemia?
Common symptoms include sudden abdominal pain, nausea, vomiting, and, in chronic cases, weight loss and fear of eating due to pain after meals. If you experience these symptoms, it’s crucial to seek medical attention promptly.
How is mesenteric ischemia diagnosed?
Diagnosis typically involves a combination of medical history assessment, physical examination, blood tests, and imaging studies such as an angiography, CT scan, or MRI. These help to identify the location and severity of the blockage.
What treatment options are available for mesenteric ischemia?
Treatment depends on the type and severity of the condition. Options include medications to manage pain and improve blood flow, minimally invasive procedures like angioplasty, or surgery to remove blockages or damaged sections of the intestine.
Is mesenteric ischemia curable?
With timely and appropriate treatment, the outlook for patients with mesenteric ischemia can be positive. However, the condition can recur, and ongoing medical supervision is often necessary.
Can lifestyle changes help with mesenteric ischemia?
Yes, lifestyle changes such as a balanced diet, regular exercise, and quitting smoking can improve overall vascular health and reduce the risk of complications associated with mesenteric ischemia.
When should I see a doctor for mesenteric ischemia?
Immediate medical evaluation is recommended if you experience sudden, severe abdominal pain or any symptoms of mesenteric ischemia. Early intervention is crucial for a better prognosis.
Conclusion
In summary, diagnosing and treating mesenteric ischemia effectively requires a keen understanding of its symptoms and the timely application of appropriate diagnostic tests. The key to managing this condition lies in early detection, which significantly improves treatment outcomes. Treatment options vary from surgical interventions to medication, depending on the severity and type of ischemia.
Equally crucial is the role of patient education in managing mesenteric ischemia. Patients must be well-informed about their condition to recognize symptoms early and seek prompt medical attention. Regular follow-ups with healthcare providers are vital to monitor the patient’s condition, adjust treatments as necessary, and prevent potential complications. Educating patients and ensuring consistent follow-up care are essential steps in improving the quality of life for those affected by this challenging medical condition.
References
For further reading and validation of the information provided on Mesenteric Ischemia Treatment, please refer to the following reputable sources:
- Mayo Clinic: Comprehensive overview of mesenteric ischemia, including symptoms, causes, and treatment options. Mayo Clinic – Mesenteric Ischemia
- Cleveland Clinic: Detailed insights into the diagnosis and management of mesenteric ischemia. Cleveland Clinic – Mesenteric Ischemia
- Johns Hopkins Medicine: In-depth information on chronic mesenteric ischemia, its surgical and non-surgical treatment options. Johns Hopkins Medicine – Chronic Mesenteric Ischemia
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Insights into mesenteric artery disease and its impact on digestive health. NIDDK – Mesenteric Artery Disease
- American College of Gastroenterology (ACG): Latest research and guidelines on the treatment of mesenteric ischemia. ACG – Mesenteric Ischemia
These sources provide authoritative and up-to-date information on mesenteric ischemia, ensuring you have access to reliable data and expert perspectives.