Meniere’s Disease Symptoms: Meniere’s Disease is a complex chronic disorder of the inner ear that can significantly impact an individual’s quality of life.
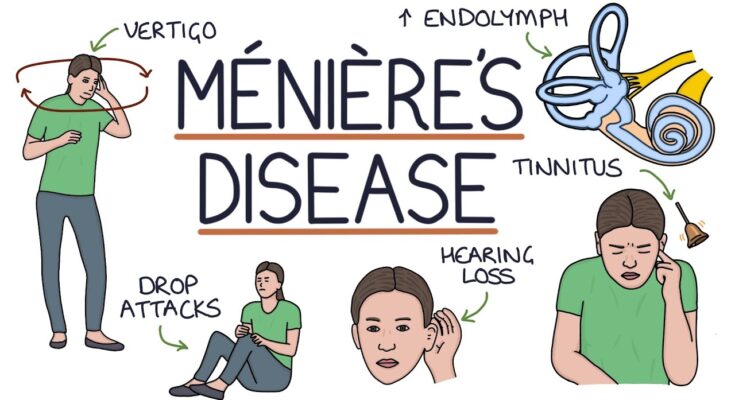
Characterized by episodes of vertigo, hearing loss, tinnitus (a ringing or buzzing in the ear), and a feeling of fullness in the affected ear, the condition can cause considerable disruption to daily activities.
It typically affects adults and is thought to occur due to abnormalities in the volume or composition of fluid in the inner ear.
What is Meniere’s Disease?
Meniere’s Disease is a chronic, potentially debilitating condition of the inner ear that affects balance and hearing. It is characterized by episodes of vertigo (a sensation of spinning), fluctuating hearing loss, tinnitus (ringing in the ears), and a feeling of pressure or fullness in the affected ear. Although the exact cause of Meniere’s Disease is unknown, it is believed to be related to abnormal fluid buildup in the inner ear. This fluid, called endolymph, helps regulate hearing and balance, and its disruption can lead to the symptoms associated with the disease.
Statistics on Prevalence and Demographics Affected
Meniere’s Disease is relatively rare, impacting between 0.1% to 0.2% of the global population. It typically first appears in adults and can affect both genders, although some studies suggest a slightly higher incidence in women. The condition most commonly begins between the ages of 40 and 60, but it can start at any age.
Regarding demographics, there is no significant difference in the prevalence of Meniere’s Disease across different racial or ethnic groups. However, geographic variations in diagnosis rates may occur, possibly due to differences in access to healthcare or diagnostic practices. The disease is considered chronic, with symptoms potentially lasting for years, although interventions can help manage its effects and improve quality of life for those affected.
However, Meniere’s Disease is a complex inner ear disorder notable for its impact on hearing and balance. It affects a small but significant number of individuals, with a fairly equal distribution across genders and no particular ethnic or racial predisposition.
Symptoms of Meniere’s Disease
Understanding these symptoms is crucial for early recognition and effective management. Below, we explore the primary symptoms of Meniere’s Disease, helping you identify and respond to early signs.
Primary Symptoms of Meniere’s Disease
- Vertigo: The most characteristic symptom of Meniere’s Disease is vertigo, a severe form of dizziness that feels as though you or your surroundings are spinning. These vertigo attacks can last anywhere from 20 minutes to several hours and are often unpredictable.
- Hearing Loss: Individuals with Meniere’s Disease commonly experience fluctuating hearing loss, particularly in one ear. This hearing impairment may worsen during an episode but can improve between attacks. Over time, however, some degree of permanent hearing loss may occur.
- Tinnitus: A persistent ringing, buzzing, or whistling sound in the ears, known as tinnitus, is another frequent symptom. Tinnitus associated with Meniere’s Disease typically affects one ear.
- Aural Fullness: Many people with Meniere’s Disease report a sensation of fullness or pressure in the ear affected by the disease. This feeling can vary in intensity and may be more pronounced during an episode.
Recognizing Early Signs of Meniere’s Disease
Early detection of Meniere’s Disease can lead to more effective management of its symptoms. Here are key indicators to watch for:
- Sudden, Severe Dizziness: Early stages of Meniere’s often include unexpected bouts of severe dizziness or vertigo. If you experience these episodes without any apparent reason, consider consulting a healthcare provider.
- Changes in Hearing: Pay attention to any fluctuation in your hearing abilities, especially if these changes occur suddenly or are limited to one ear.
- Ear Discomfort: Be aware of any feelings of pressure or fullness in one ear, as this might be an early sign of fluid buildup typical in Meniere’s Disease.
- Tinnitus Onset: New or changing tinnitus in one ear can also be a precursor to further symptoms of Meniere’s.
If you notice any of these symptoms, especially in combination, it is advisable to seek medical advice for a thorough evaluation and appropriate treatment plan.
Causes of Meniere’s Disease
The exact cause of Meniere’s Disease remains unknown, but researchers have identified several potential factors that contribute to its development. Understanding these factors can help in managing symptoms and developing treatment strategies.
Known and Speculated Causes of Meniere’s Disease
The primary suspect in Meniere’s Disease is the abnormal fluid accumulation in the inner ear, but the reasons behind this buildup are not fully understood. Several factors are believed to contribute to this condition:
- Biological Factors: Changes in the fluid, either in its volume or its concentration, can lead to Meniere’s symptoms.
- Genetic Influences: There is some evidence suggesting a genetic component, as Meniere’s Disease sometimes runs in families.
- Autoimmune Responses: The body’s immune system may mistakenly attack healthy cells in the inner ear, leading to inflammation and fluid buildup.
- Viral Infections: Some researchers believe that viral infections could initiate or worsen the condition.
- Blood Flow Issues: Poor circulation or irregularities in blood vessels supplying the inner ear may also be involved.
Explanation of the Inner Ear Anatomy Related to Meniere’s Disease
The inner ear is a complex system crucial for hearing and balance, consisting of the cochlea (for hearing) and the vestibular system (for balance). Meniere’s Disease primarily affects the labyrinth, which contains both the semicircular canals and the otolithic organs, and is filled with a fluid called endolymph. When the volume or pressure of this fluid increases, it can lead to the symptoms of Meniere’s Disease.
Role of Fluid Buildup and Biological Factors
The excessive accumulation of endolymph in the inner ear’s compartments, a condition known as endolymphatic hydrops, is central to the development of Meniere’s Disease. This fluid imbalance disrupts the normal functioning of the inner ear sensors, leading to vertigo and other auditory symptoms. Biological factors such as autoimmune reactions, genetic predisposition, and possibly infections contribute to this fluid mismanagement.
Potential Genetic, Environmental, and Lifestyle Factors
In addition to genetic predisposition, environmental and lifestyle factors may exacerbate or trigger the onset of Meniere’s Disease:
- Allergies: Some evidence links allergies to increased risk of Meniere’s, possibly due to inflammatory responses affecting the inner ear.
- Smoking: Tobacco use may impair blood flow to the inner ear, worsening symptoms.
- Diet: High salt intake can alter fluid balances, potentially leading to symptom flare-ups.
- Stress: Emotional stress is often reported as a trigger for Meniere’s symptoms, possibly due to its physiological effects on the body.
However, ongoing research continues to uncover more about the causes and mechanisms of this condition, hoping to lead to more effective treatments and preventative measures.
Diagnosing Menière’s Disease
Diagnosing it accurately is crucial as it can significantly affect quality of life. Here, we explore the common methods and criteria for diagnosing Menière’s Disease, the importance of medical history and physical examination, and the various tests and procedures used in the diagnosis.
Common Methods and Criteria for Diagnosing Menière’s Disease
The diagnosis of Menière’s disease primarily involves clinical evaluation by a healthcare provider, often a specialist in ear disorders (otologist or ENT specialist). The criteria set by the American Academy of Otolaryngology—Head and Neck Surgery for diagnosing Menière’s disease include:
- Two or more episodes of vertigo: Each lasting 20 minutes to 12 hours.
- Audiometrically documented hearing loss: On at least one occasion, which may fluctuate, especially in the early stages of the disease.
- Tinnitus or aural fullness: In the ear affected by hearing loss.
- Exclusion of other causes: After thorough testing, other potential causes of these symptoms must be ruled out.
Importance of Medical History and Physical Examination
A thorough medical history and physical examination are foundational in diagnosing Menière’s disease:
- Medical History: Understanding the patient’s symptoms, their onset, duration, and any associated factors is critical. Past medical history, including any history of ear problems, allergies, and medications, is also vital.
- Physical Examination: This includes a detailed examination of the ears, head, and neck. The doctor may perform tests to assess the function of the inner ear and balance, including observing eye movements.
Tests and Procedures Used in the Diagnosis
Several tests help confirm the diagnosis of Menière’s disease or rule out other conditions:
- Hearing Tests (Audiometry): These tests assess the type and degree of hearing loss and are crucial for diagnosing Menière’s disease.
- Vestibular and Balance Tests: Tests like the Videonystagmography (VNG) or Electronystagmography (ENG) can evaluate balance function and the integrity of the inner ear and pathways to the brain.
- Electrocochleography (ECoG): This test measures the electrical activity in the inner ear and can be helpful in Menière’s disease diagnosis by detecting increased inner ear fluid pressure.
- Magnetic Resonance Imaging (MRI): An MRI can rule out other causes of vertigo and hearing loss, such as a tumor on the hearing and balance nerve (acoustic neuroma).
However, accurately diagnosing Menière’s disease is a stepwise process involving detailed patient history, careful physical examination, and specific diagnostic tests.
Managing Symptoms of Meniere’s Disease
Managing these symptoms effectively is crucial for improving life quality and functionality. Here, we explore various treatment options, lifestyle modifications, medical treatments, and support resources available for those living with Meniere’s Disease.
Treatment Options to Manage Symptoms
- Dietary Adjustments: Reducing salt intake can help decrease fluid retention, potentially minimizing the severity of symptoms. It’s also beneficial to maintain a balanced diet and stay hydrated.
- Stress Management: Stress can exacerbate symptoms. Techniques such as yoga, meditation, and counseling can be helpful.
- Routine Sleep Patterns: Consistent sleep schedules support overall body equilibrium, which might help reduce the frequency of Meniere’s episodes.
- Avoiding Triggers: Common triggers include caffeine, alcohol, and tobacco. Identifying and avoiding these can help manage symptoms.
Lifestyle Modifications and Their Effectiveness
Lifestyle changes can significantly impact the severity and frequency of Meniere’s disease symptoms:
- Low Sodium Diet: One of the most recommended strategies for fluid regulation in the inner ear, which can help reduce the pressure and severity of symptoms.
- Physical Activity: Regular exercise helps in overall circulation and health, potentially reducing the impact of Meniere’s disease.
- Positive Sleep Hygiene: Adequate sleep aids neurological health and stress reduction, which are critical in managing Meniere’s disease.
Medical Treatments: Medications and Surgical Options
- Medications:
- Diuretics: Help reduce fluid retention in the body.
- Anti-nausea and Anti-vertigo Medications: These can help manage acute attacks of vertigo.
- Steroids or Gentamicin Injections: These are used in severe cases to reduce inner ear fluid and inflammation.
- Surgical Options:
- Endolymphatic Sac Surgery: This procedure aims to relieve fluid pressure in the inner ear.
- Vestibular Nerve Section: A more invasive option that might be considered when other treatments fail.
- Labyrinthectomy: Usually a last resort when hearing preservation is not a concern.
Support and Resources for People Living with Meniere’s Disease
Living with Meniere’s Disease can be challenging, but there are numerous resources available for support:
- Support Groups: Many online and local support groups offer a platform for sharing experiences and coping strategies.
- Counseling and Therapy: Professional help can be vital in managing the psychological impacts of chronic illness.
- Educational Resources: Organizations such as the Vestibular Disorders Association (VeDA) provide valuable information and support materials.
- Regular Check-ups: Ongoing medical support from healthcare professionals specializing in ear disorders is crucial.
However, tailoring these strategies to individual needs and symptoms can lead to better management of the condition and an improved quality of life.
FAQs about Meniere’s Disease Symptoms
1. What are the primary symptoms of Meniere’s Disease?
Meniere’s Disease is characterized by several key symptoms, including vertigo (a sensation of spinning), hearing loss, tinnitus (ringing in the ears), and a feeling of pressure or fullness in the affected ear. These symptoms can vary in intensity and duration.
2. How does vertigo affect those with Meniere’s Disease?
Vertigo, one of the most debilitating symptoms of Meniere’s Disease, involves severe dizziness that can last from a few minutes to several hours. This can significantly impact balance and mobility, often requiring individuals to rest until the episode passes.
3. Is hearing loss in Meniere’s Disease permanent?
Hearing loss associated with Meniere’s Disease may fluctuate, especially in the early stages. However, over time, some individuals may experience progressively worsening, permanent hearing loss.
4. Can symptoms of Meniere’s Disease appear suddenly?
Yes, the symptoms of Meniere’s Disease can occur suddenly and unexpectedly. The unpredictable nature of these episodes can make it challenging for individuals to manage their daily activities without prior warning.
5. What triggers Meniere’s Disease symptoms?
While the exact cause of Meniere’s Disease is unknown, symptom flare-ups can be triggered by factors such as stress, dietary habits (especially salt intake), and changes in barometric pressure. Identifying and avoiding individual triggers can help manage the condition.
6. Are there any age or demographic groups more at risk for Meniere’s Disease?
Meniere’s Disease typically affects adults between the ages of 20 and 50, but it can occur at any age. Both men and women are equally likely to develop the condition, and there is no clear demographic preference.
7. How can someone differentiate Meniere’s Disease from other forms of vertigo or dizziness?
Meniere’s Disease is usually distinguished by the combination of symptoms such as hearing loss, tinnitus, and ear fullness along with vertigo. Other forms of vertigo may not include these additional symptoms. Diagnosis typically involves audiometric tests and sometimes imaging studies to rule out other causes.
8. Is tinnitus always present in Meniere’s Disease?
While tinnitus is a common symptom of Meniere’s Disease, its presence and severity can vary among individuals. Some may experience mild tinnitus, while others might face more disruptive, louder ringing.
Conclusion
In summary, Meniere’s Disease is a complex condition characterized by a variety of symptoms including vertigo, tinnitus, hearing loss, and a sensation of fullness in the ear. The exact causes of Meniere’s Disease remain unclear, but they are believed to involve fluid imbalances in the inner ear, possibly influenced by genetic factors, viral infections, or autoimmune responses.
If you are experiencing any symptoms similar to those associated with Meniere’s Disease, it is crucial to seek professional medical advice. An early diagnosis can help manage the symptoms effectively and improve your quality of life. Remember, only a healthcare professional can provide a proper diagnosis and recommend appropriate treatment options tailored to your specific needs.
References
For a deeper understanding and validation of the information provided on Meniere’s Disease symptoms, the following reputable sources are highly recommended. These resources offer detailed insights and further reading:
- Mayo Clinic – An extensive overview of Meniere’s Disease, including symptoms, causes, and treatment options. Read more about Meniere’s Disease at Mayo Clinic.
- National Institute on Deafness and Other Communication Disorders (NIDCD) – Offers comprehensive information on Meniere’s Disease, helping patients and healthcare providers understand the condition better. Explore Meniere’s Disease on NIDCD.
- Healthline – Provides a detailed article on the symptoms, diagnosis, and management of Meniere’s Disease, written with patient-friendly language. Learn more about Meniere’s Disease on Healthline.
These resources are maintained by well-respected institutions and offer up-to-date and research-backed information, making them excellent references for anyone looking to learn more about Meniere’s Disease.