Meniere’s Disease Treatment: Meniere’s Disease is a complex disorder characterized by a combination of symptoms including vertigo, tinnitus (ringing in the ears), hearing loss, and a feeling of pressure deep within the ear.
These symptoms are caused by an abnormality in the fluid balance in the inner ear. The condition predominantly affects adults and can significantly impact quality of life.
Understanding Meniere’s Disease
Meniere’s Disease is a chronic, often debilitating inner ear disorder that primarily affects the balance and hearing systems. Understanding this condition begins with recognizing its key characteristics, understanding who it affects most, and appreciating the role of the inner ear in its development.
Key Characteristics of Meniere’s Disease
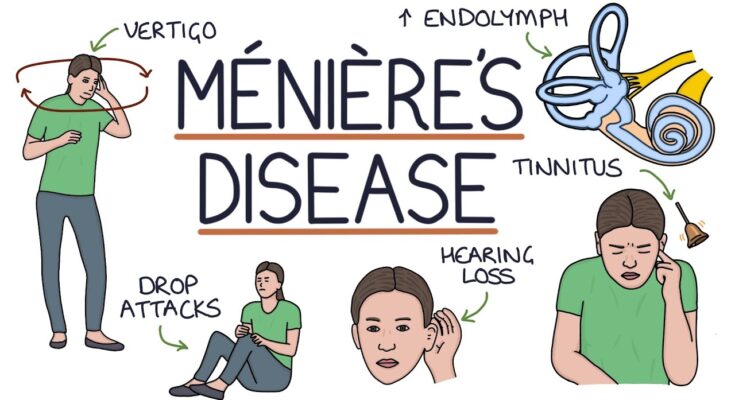
Meniere’s Disease is marked by a combination of symptoms that can significantly impact quality of life. The primary features include:
- Vertigo: Sudden and severe episodes of dizziness that can cause a spinning sensation, typically lasting from 20 minutes to several hours.
- Hearing Loss: Fluctuating, progressive hearing loss that typically affects one ear. This hearing loss can become permanent over time.
- Tinnitus: The presence of ringing, buzzing, or hissing sounds in the ear.
- Aural Fullness: A sensation of fullness or pressure in the affected ear, which can fluctuate in intensity.
Epidemiology: Who is Most Affected?
Meniere’s Disease can occur at any age, but it most commonly begins between the ages of 40 and 60. Both men and women are equally likely to be diagnosed with this condition. It is relatively rare, affecting about 0.2% of the population. While the exact cause of Meniere’s Disease is unknown, factors like genetics, viral infections, and autoimmune reactions are thought to contribute to its development.
The Inner Ear and Its Role in Meniere’s Disease
The inner ear is critical in the process of hearing and balance, comprising two main structures: the cochlea for hearing and the vestibular system for balance. In Meniere’s Disease, fluid build-up in the inner ear (endolymphatic hydrops) disrupts the normal balance and hearing signals processed by the brain. This disruption is what leads to the symptoms of vertigo, hearing loss, and tinnitus.
However, understanding these components is crucial for recognizing and managing Meniere’s Disease effectively. Awareness and early diagnosis can help manage symptoms and improve the quality of life for those affected.
Symptoms of Meniere’s Disease
Understanding these symptoms, how they contribute to a diagnosis, and their effects on daily activities is crucial for those affected by the condition.
Detailed List of Symptoms
Meniere’s Disease is characterized by a specific set of symptoms that can vary in intensity and frequency among individuals:
- Vertigo: Sudden episodes of dizziness that can last from a few minutes to several hours, often described as a feeling that the room is spinning.
- Hearing Loss: Fluctuating hearing impairment in the affected ear, which may become permanent over time.
- Tinnitus: A persistent ringing, buzzing, or whistling sound in the ear that is not caused by external noise.
- Aural Fullness: A sensation of pressure or fullness in the ear, which can be particularly uncomfortable.
How Symptoms Lead to Diagnosis
The diagnosis of Meniere’s Disease typically involves a combination of clinical evaluation and diagnostic tests. The recurring nature of the symptoms, especially vertigo, hearing loss, and tinnitus, plays a crucial role in diagnosis. Medical professionals often use the following criteria to diagnose the condition:
- Recurrent episodes of vertigo: Each lasting 20 minutes to several hours.
- Audiometrically documented hearing loss: On at least one occasion, confirming the fluctuating nature of the impairment.
- Tinnitus or fullness of the ear: Present in the affected ear during symptomatic periods.
Exclusion of other conditions that might mimic Meniere’s Disease is also essential, and this is typically achieved through detailed medical history, physical examination, and sometimes imaging and balance tests.
Impact of These Symptoms on Daily Life
The symptoms of Meniere’s Disease can have a profound effect on daily life, influencing both physical and emotional well-being:
- Mobility Issues: Episodes of vertigo can make driving, operating machinery, or even walking extremely dangerous.
- Workplace Challenges: Fluctuating hearing loss and vertigo attacks can make it difficult to perform at work, attend meetings, or communicate effectively.
- Social and Emotional Impact: Chronic tinnitus and the unpredictability of symptoms can lead to anxiety, depression, and social isolation.
- Sleep Disturbances: Vertigo and ear fullness can disrupt sleep patterns, leading to fatigue and decreased energy during the day.
However, managing these symptoms often requires a combination of medication, lifestyle adjustments, and sometimes therapy or counseling to cope with the emotional stress of the disease.
Diagnosing Meniere’s Disease
Diagnosing this condition promptly and accurately is crucial for effective management and treatment. This guide provides a clear step-by-step overview of the diagnostic process, outlines the key methods used, explains the importance of differential diagnosis, and highlights why early detection is critical.
Step-by-Step Guide to the Diagnostic Process
- Patient History and Symptoms Review: The initial step involves a detailed discussion with the patient about their symptoms, including the duration, frequency, and intensity of vertigo attacks, hearing loss, and occurrences of tinnitus. Understanding the history of these symptoms is pivotal.
- Physical Examination: A thorough physical examination helps rule out other causes of the symptoms. The doctor may perform a series of tests to assess hearing and balance.
- Hearing Assessment: Audiometric tests are conducted to evaluate the extent of hearing loss. These tests can help in identifying typical patterns of hearing impairment associated with Meniere’s disease.
- Balance Tests: To examine the inner ear and balance, tests like the Videonystagmography (VNG) or Electronystagmography (ENG) may be used. These tests measure eye movements that correspond to inner ear functions and can pinpoint abnormalities.
- Imaging Tests: In some cases, MRI or CT scans are necessary to visually assess the inner ear and surrounding structures for any anomalies that could be causing the symptoms.
Methods of Diagnosing Meniere’s Disease
- Electrocochleography (ECoG): This test measures the electrical potentials generated in the inner ear as a response to sound, helping to detect increased fluid pressure in the inner ear.
- Glycerol Test: This involves administering glycerol to the patient and measuring hearing before and after intake, observing for significant improvement, which suggests Meniere’s disease.
- Vestibular Evoked Myogenic Potentials (VEMP) Testing: VEMP testing assesses the function of sensors in the vestibule of the ear, which are part of the balance system.
The Role of Differential Diagnosis
Differential diagnosis is essential in the process as it helps distinguish Meniere’s disease from other conditions with similar symptoms, such as vestibular migraine or benign paroxysmal positional vertigo (BPPV). By ruling out these conditions, clinicians can focus on the specific treatment needed for Meniere’s.
Importance of Early and Accurate Diagnosis
An early and precise diagnosis is vital for several reasons:
- Effective Management: Early intervention can help manage symptoms more effectively, preventing severe attacks and potential complications.
- Treatment Planning: Accurate diagnosis allows for a tailored treatment plan that can include lifestyle changes, medications, or even surgery, thereby improving the overall prognosis.
- Quality of Life: Prompt diagnosis and treatment can significantly enhance the patient’s quality of life by reducing the frequency and intensity of the episodes.
However, understanding the diagnostic process for Meniere’s disease is crucial for patients and healthcare providers alike, ensuring timely and appropriate management of this challenging condition.
Treatment Options for Meniere’s Disease
Below, we explore various strategies, including medications, non-pharmacological treatments, lifestyle modifications, and surgical options that contribute to achieving these goals.
Treatment Goals and Strategies
The overarching aims of treating Meniere’s disease include:
- Minimizing Vertigo: Controlling and reducing the severity of vertigo episodes is a key treatment goal.
- Improving Hearing: Efforts are made to stabilize or improve hearing levels.
- Managing Tinnitus: Reducing the ringing or noise in the ears associated with Meniere’s.
- Enhancing Quality of Life: Addressing the psychological and emotional impact of the disease.
Medications
Medications are frequently used to manage symptoms of Meniere’s disease:
- Diuretics: Sometimes called “water pills,” these help reduce fluid retention in the body and potentially in the inner ear, helping to control vertigo.
- Betahistine: Increases blood flow in the inner ear, which might reduce vertigo and hearing loss.
- Anti-nausea and Antiemetics: These medications help manage nausea and vomiting during vertigo attacks.
- Steroids: Can be injected into the middle ear to help reduce inflammation and control vertigo episodes.
Non-Pharmacological Treatments
In addition to medication, several non-drug therapies can be beneficial:
- Vestibular Rehabilitation Therapy (VRT): A form of physical therapy aimed at helping the brain adapt to the changes in the inner ear, improving balance and minimizing dizziness.
- Hearing Aids: Used in cases where hearing loss has occurred, these devices can help manage the auditory symptoms of Meniere’s disease.
- Meniett Device: A device that uses pressure pulses to help normalize the fluid in the inner ear, potentially reducing the frequency of vertigo attacks.
Lifestyle Modifications
Lifestyle changes can also play a significant role in managing Meniere’s disease:
- Salt Reduction: Lowering sodium intake helps regulate fluid volumes in the body, potentially reducing inner ear fluid pressure.
- Avoiding Caffeine and Alcohol: These substances can exacerbate symptoms, so reducing or eliminating them may help control episodes.
- Stress Management: Techniques such as yoga, meditation, and counseling can be effective in managing the stress associated with Meniere’s.
- Regular Sleep Patterns: Consistency in sleep can help stabilize body functions, including those related to inner ear fluid dynamics.
Surgical Options
Surgery may be considered when other treatments have failed to control severe symptoms:
- Endolymphatic Sac Decompression: Surgery to alleviate fluid pressure within the inner ear.
- Vestibular Nerve Section: A procedure that involves cutting the nerve that sends balance signals to the brain from the inner ear, helping to reduce vertigo.
- Labyrinthectomy: Removing part or all of the inner ear structure, which can eliminate vertigo but also results in total hearing loss in the affected ear.
However, each treatment strategy for Meniere’s disease has its own benefits and risks, and a healthcare provider can help tailor an approach based on the individual’s specific symptoms and health profile.
Managing Meniere’s Disease
Below, we delve into the various aspects of managing Meniere’s Disease with a focus on long-term management strategies, the importance of physical therapy and rehabilitation, and the essential coping mechanisms and support systems.
Long-Term Management Strategies for Meniere’s Disease
- Dietary Adjustments: Reducing salt intake can help manage fluid retention, potentially minimizing the severity and frequency of vertigo attacks. It’s also beneficial to maintain a balanced diet and avoid caffeine and alcohol, which can trigger symptoms.
- Medication: Certain medications can be used to reduce fluid buildup, control allergies, and alleviate nausea and vertigo. Diuretics (water pills) and anti-vertigo medications are commonly prescribed.
- Regular Monitoring: Regular check-ups with an ENT specialist or audiologist are crucial. Monitoring the progress of the disease can help in adjusting treatment plans as needed.
- Stress Management: Stress can exacerbate symptoms, so incorporating stress-reduction techniques like meditation, yoga, or deep-breathing exercises can be beneficial.
- Hearing Aids: For those experiencing hearing loss, hearing aids may be recommended to improve hearing and communication.
The Role of Physical Therapy and Rehabilitation
- Vestibular Rehabilitation Therapy (VRT): This is a specialized form of therapy designed to alleviate both the primary and secondary problems caused by vestibular disorders. VRT involves exercises that help compensate for inner ear deficits and improve balance.
- Balance Training: Exercises that enhance balance can help reduce the risk of falls and improve stability, which is especially important for Meniere’s disease patients experiencing frequent vertigo.
- Customized Exercise Plans: Based on individual needs, physical therapists may develop tailored exercise routines to help manage specific symptoms effectively.
Coping Mechanisms and Support Systems
- Support Groups: Connecting with others who have Meniere’s disease can provide emotional support and practical advice. Support groups offer a platform to share experiences and coping strategies.
- Counseling and Therapy: Psychological counseling or cognitive-behavioral therapy can help individuals cope with the emotional and mental challenges posed by chronic illness.
- Education and Awareness: Understanding the disease and being aware of the potential triggers can help individuals avoid situations that may worsen their symptoms.
- Family and Friends: Educating family and friends about Meniere’s disease can help them provide better support during symptomatic episodes.
However, managing this condition is a continuous process that involves regular medical care, lifestyle adjustments, and emotional support, aiming to reduce the impact of symptoms and enhance overall well-being.
Advances in Meniere’s Disease Treatment
Meniere’s disease, a complex condition characterized by vertigo, tinnitus, and hearing loss, has seen promising advancements in treatment due to recent research and emerging therapies. Staying informed about these developments is crucial for both patients and healthcare providers.
Recent Research and Emerging Treatments
- Intratympanic Steroid Injections: These injections have become more prevalent as a treatment option. Research shows that steroids delivered directly into the middle ear can help reduce the frequency and intensity of vertigo attacks.
- Betahistine: Although not new, betahistine’s effectiveness continues to be studied, with recent trials suggesting improved dosing strategies to enhance its efficacy in reducing vertigo episodes.
- Dietary Management: Recent studies emphasize the role of a low-salt diet combined with proper hydration in managing symptoms, potentially reducing the need for more aggressive treatments.
- Vestibular Rehabilitation Therapy (VRT): This tailored therapy program helps patients manage balance issues resulting from Meniere’s disease. Recent advancements in VRT techniques have shown improved outcomes in patient stability and quality of life.
- Meniett device: This portable device, which applies pulsatile pressure to the middle ear to improve fluid exchange, has gained attention for its non-invasive approach to reducing vertigo episodes.
Potential Future Therapies and Ongoing Clinical Trials
- Gene Therapy: Ongoing research into the genetic bases of Meniere’s disease may open the door to gene therapies that target the underlying causes of the condition rather than just managing symptoms.
- Regenerative Medicine: Studies are exploring the potential of stem cells to regenerate damaged inner ear cells and tissues, a promising area that could revolutionize treatment options in the future.
- Novel Pharmacological Treatments: Researchers are continuously testing new drugs that target specific pathways involved in the disease process. These include antioxidants and anti-inflammatory agents that could help mitigate inner ear damage.
- Clinical Trials: Numerous clinical trials are underway, investigating everything from the effectiveness of different drug regimens to the long-term outcomes of surgical interventions. Patients interested in participating in these trials can look for information on clinical trial registries or through their healthcare providers.
By keeping abreast of these advancements, patients suffering from Meniere’s disease can foster a proactive approach in managing their condition, potentially leading to better overall outcomes and quality of life.
FAQs about Meniere’s Disease Treatment
What is Meniere’s disease?
Meniere’s disease is a chronic inner ear disorder that causes episodes of vertigo, hearing loss, ringing in the ear (tinnitus), and sometimes a feeling of fullness or pressure in the ear.
How is Meniere’s disease treated?
Treatment for Meniere’s disease aims to manage symptoms and may include diet changes (like reducing salt intake), medications to reduce fluid buildup and relieve vertigo, and therapy for hearing loss and tinnitus. In severe cases, surgery might be considered.
Can changes in diet really help with Meniere’s disease?
Yes, dietary changes, particularly reducing salt intake, can help decrease fluid retention in the body, which may reduce the severity and frequency of Meniere’s disease episodes.
Are there any effective natural remedies for Meniere’s disease?
Some people find relief through natural remedies like acupuncture, herbal supplements, and stress management techniques. However, it’s essential to consult with a healthcare provider before starting any natural treatment to ensure it’s safe and suitable for your specific condition.
Is Meniere’s disease curable?
While there is no cure for Meniere’s disease, the treatment focuses on managing symptoms and improving quality of life. Many people with Meniere’s disease find that their symptoms improve with treatment and lifestyle adjustments.
How long do treatment effects last?
The effects of treatment can vary widely among individuals. Some may experience prolonged relief, while others might have recurring symptoms. Regular follow-ups with a healthcare provider are crucial to adjust treatment plans as needed.
Can Meniere’s disease lead to permanent hearing loss?
Yes, Meniere’s disease can lead to progressive hearing loss over time. Managing the disease effectively with the help of healthcare providers can help slow down the progression of hearing loss.
Conclusion
If you or someone you know is experiencing symptoms suggestive of Meniere’s Disease, it is essential to seek professional healthcare advice. Early diagnosis and tailored treatment plans can significantly mitigate the impacts of the disease, helping patients lead more comfortable and fulfilling lives. Adhering to the prescribed treatment regimen, whether it involves medication, therapy, or lifestyle modifications, is vital for managing symptoms effectively.
We encourage patients to maintain regular follow-ups with their healthcare provider, stay informed about their condition, and actively participate in their treatment planning. With the right support and management strategies, living well with Meniere’s Disease is achievable.
References
For those seeking more in-depth information on Meniere’s Disease and its treatment options, the following reputable sources provide extensive insights and are essential for validating the information presented:
- Mayo Clinic: Comprehensive overview of Meniere’s Disease, including symptoms, causes, and treatment methods. Read more about Meniere’s Disease at Mayo Clinic.
- National Institute on Deafness and Other Communication Disorders (NIDCD): Offers detailed information on Meniere’s Disease, focusing on research, statistics, and potential treatment advances. Explore NIDCD’s resources on Meniere’s Disease.
- American Academy of Otolaryngology-Head and Neck Surgery: Provides guidelines and treatment protocols for practitioners, which can also be useful for patients looking for detailed treatment procedures. Visit the American Academy’s page on Meniere’s Disease.
- MedlinePlus: A resource from the U.S. National Library of Medicine offering accessible information on diseases, including Meniere’s. Learn more about Meniere’s Disease on MedlinePlus.
These sources are invaluable for patients, healthcare providers, and researchers interested in the latest developments and comprehensive treatments for Meniere’s Disease. They not only enhance understanding but also support the credibility of the information shared on this topic.