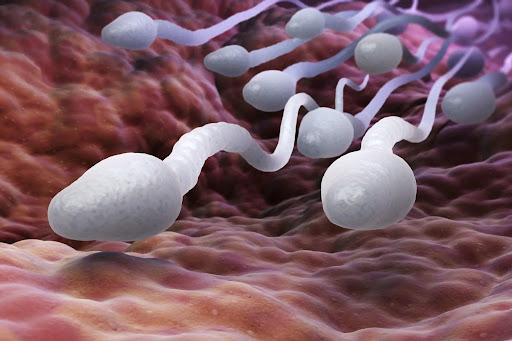
Low Sperm Count Symptoms: Low sperm count, medically referred to as oligospermia, is a prevalent male fertility issue affecting millions worldwide.
This condition is characterized by the presence of fewer than 15 million sperm per milliliter of semen, a threshold set by the World Health Organization.
Understanding the symptoms and causes of low sperm count is crucial for identifying potential health concerns and exploring effective treatment options.
Understanding Low Sperm Count
Low sperm count, medically known as oligospermia, is a common fertility issue affecting many men worldwide. This condition is characterized by a sperm count that falls below the threshold of 15 million sperm per milliliter of semen, as defined by the World Health Organization. It’s important to highlight why understanding and addressing low sperm count is critical for couples trying to conceive.
General Statistics
- Prevalence: Studies estimate that low sperm count affects approximately 10-15% of the male population globally.
- Impact on Fertility: About one-third of infertility cases are attributed to male reproductive issues, with low sperm count being a leading factor.
- Age Factor: The quality and quantity of sperm generally decrease with age, particularly affecting men over 40.
Why It’s a Concern
Low sperm count is a concern for many because it directly impacts the ability to conceive naturally. For couples planning a family, this can be a significant emotional and psychological challenge. Furthermore, a low sperm count can sometimes indicate underlying health issues, such as hormonal imbalances, genetic problems, or environmental factors, which might require medical attention.
However, awareness leads to better management options, such as lifestyle changes, medical interventions, or assisted reproductive technologies, thus improving the chances of conception for many couples.
Symptoms of Low Sperm Count
Recognizing the signs can be crucial for addressing reproductive issues. Here are the common symptoms associated with low sperm count:
- Reduced Sexual Function: This may include a decrease in libido, difficulty maintaining an erection (erectile dysfunction), or other sexual function issues.
- Pain, Swelling, or a Lump in the Testicle Area: Any discomfort, swelling, or noticeable changes in the testicles could be a sign of underlying issues affecting sperm production.
- Decreased Facial or Body Hair or Other Signs of a Hormonal Imbalance: In some cases, a low sperm count is linked to lower hormone levels, which can also affect hair growth and other physical characteristics.
- Infertility: The most direct symptom of low sperm count is an inability to conceive a child after a year of regular, unprotected sexual intercourse.
When to See a Doctor: Guidance on Seeking Medical Advice
It’s important to consult a healthcare provider if you experience any of the above symptoms, especially if you and your partner are trying to conceive without success. Here are specific situations when seeing a doctor becomes essential:
- Persistent Sexual Problems: If issues like reduced sexual desire or erectile difficulties last for an extended period.
- Pain or Discomfort: Any unexplained pain, swelling, or lumps in the testicle area should be evaluated promptly.
- Infertility Concerns: If you and your partner have not achieved pregnancy after a year of regular, unprotected intercourse, it’s advisable to undergo a medical evaluation to determine the underlying cause.
- Signs of Hormonal Problems: Such as reduced body or facial hair associated with other symptoms of hormonal imbalances.
However, early medical intervention can be crucial in diagnosing and effectively treating low sperm count, enhancing the chances for successful conception and addressing any related health concerns.
Causes of Low Sperm Count
Understanding these causes can help in addressing the issue effectively. Below, we explore the medical, environmental, and lifestyle and health-related causes of low sperm count.
Medical Causes
- Varicocele: A swelling of the veins that drain the testicle, varicocele is the most common reversible cause of male infertility.
- Infections: Infections like epididymitis, orchitis, or sexually transmitted infections (STIs) such as HIV or gonorrhea can impair sperm production or cause scarring that blocks the passage of sperm.
- Ejaculation Problems: Conditions such as retrograde ejaculation occur when semen enters the bladder during orgasm instead of emerging out of the penis.
- Antibodies that Attack Sperm: Immune system cells may mistakenly identify sperm as a harmful invader and attempt to eliminate them.
- Hormone Imbalances: Disorders of the testicles, pituitary gland, or hypothalamus can affect hormone levels and diminish sperm production.
- Defects of Tubules that Transport Sperm: Blockages in the tubes that carry sperm can be caused by various conditions, including congenital defects or infections.
- Chromosome Defects: Disorders such as Klinefelter’s syndrome—a condition in which a male is born with two X chromosomes and one Y chromosome—can affect male fertility.
- Celiac Disease: A digestive disorder caused by an adverse reaction to gluten, which may also impact fertility.
- Certain Medications: Long-term use of medications like anabolic steroids, cancer therapies, or certain antifungal and ulcer drugs can impair sperm production.
Environmental Causes
- Exposure to Heavy Metals: Exposure to lead or other heavy metals can affect sperm quantity and quality.
- Radiation or X-rays: Exposure to radiation can reduce sperm production, with effects that can be temporary or permanent.
- Overheating the Testicles: Frequent use of saunas or hot tubs, wearing tight clothing, or working in hot environments can increase the scrotal temperature, impairing sperm production.
Lifestyle and Health-Related Causes
- Drug Use: Anabolic steroids used to build muscle and enhance athletic performance can significantly decrease sperm production. Use of cocaine or marijuana can also reduce the number and quality of sperm.
- Alcohol Use: Heavy drinking can lead to lower testosterone levels and decreased sperm production.
- Occupational Factors: Jobs that involve exposure to toxic chemicals, heavy metals, radiation, or high heat can all reduce sperm count.
- Tobacco Smoking: Smoking significantly lowers both sperm count and sperm cell motility.
- Emotional Stress: Stress can interfere with certain hormones needed to produce sperm.
- Weight: Obesity can directly impact sperm count by altering hormone levels and causing hormone imbalances.
By addressing these factors, individuals may improve their sperm production and overall fertility. Understanding the root cause is crucial for effective treatment and lifestyle adjustments.
Diagnosing Low Sperm Count
Diagnosing a low sperm count is a crucial step for individuals facing difficulties in conceiving. Understanding the diagnosis process can help in taking informed steps towards managing or treating this condition. Here’s a detailed guide on how the diagnosis is typically conducted and the additional tests that may be required.
Process of Diagnosis
- Initial Consultation: The diagnosis process begins with a detailed medical consultation. During this session, the doctor will inquire about your medical history, lifestyle, and any symptoms you might be experiencing. This also includes discussing any past or present illnesses, surgeries, and family history of fertility issues.
- Semen Analysis: The cornerstone of diagnosing low sperm count is a semen analysis. You will be asked to provide a semen sample, which will be analyzed in a laboratory to measure the quantity, shape, and mobility of the sperm. This test might need to be repeated two to three times over several weeks to confirm the diagnosis, as sperm count can vary over time.
- Physical Examination: A thorough physical examination is often performed to check for any physical anomalies in the reproductive system that could affect sperm production.
- Hormonal Profile: Hormonal imbalances can impact sperm production. A blood test to check levels of testosterone and other hormones is commonly recommended.
Additional Tests
- Ultrasound: An ultrasound of the scrotum can help identify any issues with the testicles or supporting structures that might be affecting sperm production.
- Genetic Tests: If there’s an indication of a possible genetic cause of low sperm count, genetic tests may be suggested. These tests can detect chromosomal abnormalities or specific genetic faults.
- Post-ejaculation Urinalysis: This test checks for sperm in the urine, helping to identify whether sperm are traveling backward into the bladder instead of out of the penis during ejaculation (retrograde ejaculation).
- Testicular Biopsy: In cases where the semen analysis shows very few or no sperm, a biopsy may be necessary to determine the cause.
- Specialized Sperm Function Tests: These tests include assessing how well sperm survive after ejaculation, how they penetrate an egg, or whether there’s an issue with the sperm’s DNA.
Remember, a diagnosis of low sperm count doesn’t necessarily mean it’s impossible to conceive; it simply guides further steps in fertility management or treatment.
Treatment Options for Low Sperm Count
Understanding and choosing the right treatment option can lead to successful outcomes for many couples.
Medical Treatments
- Hormonal Therapy: Hormonal imbalances can impact sperm production. Treatment with medications such as gonadotropins or clomiphene citrate can help improve hormone levels and stimulate sperm production.
- Antibiotics: Infections that affect sperm count can be treated with antibiotics. However, this does not always restore fertility.
- Surgery: Surgical interventions can correct obstructions or varicoceles (enlarged veins in the scrotum) that impair sperm production and quality. Procedures such as varicocelectomy or a vasectomy reversal can significantly impact sperm count.
- Medication: Certain medications, like alpha blockers, can assist with ejaculation issues, improving the chances of natural conception.
Lifestyle Changes
- Diet and Exercise: Improving diet, maintaining a healthy weight, and engaging in regular physical activity can boost fertility. Antioxidants, which are abundant in fruits and vegetables, have been shown to improve sperm quality.
- Avoiding Toxins: Limit exposure to environmental toxins and chemicals, such as pesticides and heavy metals, which can affect sperm count.
- Reduce Stress: High stress levels can affect hormone levels and sperm production. Stress management techniques such as meditation, yoga, and counseling can be beneficial.
- Quit Smoking and Limit Alcohol: Smoking and excessive alcohol consumption have been linked to reduced sperm production. Quitting smoking and reducing alcohol intake can improve sperm quality.
Assisted Reproductive Technologies (ART)
- In Vitro Fertilization (IVF): IVF involves combining sperm and eggs outside the body in a lab. Once an embryo forms, it is placed in the uterus. IVF can be particularly useful when sperm count is low.
- Intracytoplasmic Sperm Injection (ICSI): ICSI is a specialized form of IVF that involves directly injecting a single sperm into an egg. This method is highly effective if the sperm count is extremely low.
- Sperm Donation: When other treatments are not viable or effective, using sperm from a donor can be an option.
However, consulting with a fertility specialist can provide guidance tailored to an individual’s specific condition, increasing the likelihood of conceiving a child.
Prevention Tips for Low Sperm Count
Maintaining a healthy sperm count is crucial for fertility and overall well-being. Here are proactive measures and lifestyle choices that can help prevent low sperm count.
Proactive Measures to Prevent Low Sperm Count
- Maintain a Healthy Diet: Consuming a balanced diet rich in antioxidants can improve sperm health. Foods high in vitamin C, vitamin E, zinc, and selenium are known to boost sperm count and quality.
- Exercise Regularly: Moderate physical activity can increase levels of powerful antioxidant enzymes, which can help protect sperm cells from damage.
- Avoid Substance Abuse: Limiting alcohol intake and avoiding tobacco and recreational drugs are essential steps in protecting sperm health.
- Manage Stress: Chronic stress can interfere with certain hormones needed to produce sperm. Techniques such as mindfulness, yoga, and regular exercise can be effective in stress management.
- Keep Cool: Elevated temperatures can affect sperm production. Avoid hot tubs, saunas, and tight clothing around the groin to maintain a temperature conducive to sperm production.
- Limit Exposure to Toxins: Minimize exposure to environmental toxins like pesticides, heavy metals, and other harmful chemicals that can affect sperm count and quality.
Importance of Regular Health Checks and Healthy Lifestyle Choices
- Early Detection: Regular health checks can help detect and address underlying health issues that may affect sperm production, such as hormonal imbalances or infections.
- Monitoring Hormonal Health: Hormonal health plays a crucial role in sperm production. Regular screenings can ensure that hormone levels are balanced and conducive to producing healthy sperm.
- Weight Management: Maintaining a healthy weight can improve sperm count. Obesity has been linked to decreased sperm production and can negatively affect hormone levels.
- Quit Smoking: Smoking has been shown to decrease sperm health and count significantly. Quitting smoking is not only beneficial for overall health but also for reproductive health.
- Review Medications: Some medications can impact sperm production. A regular review with a healthcare provider can help manage any adverse effects from current medications.
However, regular consultations with healthcare providers can tailor these suggestions to individual health needs and conditions.
FAQs about Low Sperm Count Symptoms
1. What are the common symptoms of a low sperm count?
Typically, there are no obvious signs of low sperm count. However, some associated symptoms might include reduced sexual desire, difficulty maintaining an erection, pain or swelling in the testicle area, and reduced facial or body hair which could suggest hormonal abnormalities.
2. Can a low sperm count cause infertility?
Yes, a low sperm count is a leading cause of male infertility. It decreases the likelihood of a sperm fertilizing the egg, thereby reducing the chances of conception.
3. How can I tell if I have a low sperm count?
The only definitive way to determine sperm count is through a semen analysis, which measures the volume of semen and the concentration of sperm in the semen.
4. Are there lifestyle factors that affect sperm count?
Yes, several factors can impact sperm production, including smoking, excessive alcohol consumption, stress, obesity, and exposure to environmental toxins. A healthy lifestyle can help maintain optimal sperm production.
5. Is low sperm count treatable?
Yes, treatments vary based on the underlying cause but can include medication, hormone treatments, and lifestyle changes such as improving diet, exercising, and reducing stress. In some cases, assisted reproductive technologies (ART) may be recommended.
6. What should I do if I suspect I have a low sperm count?
It is advisable to consult with a healthcare provider. They can perform a semen analysis and offer guidance on appropriate treatment options based on the results.
Conclusion
In conclusion, recognizing the symptoms of low sperm count is crucial for early intervention. Key indicators can include reduced semen volume, difficulties with sexual function, and less facial or body hair, which may suggest hormonal imbalances. If you experience any of these symptoms, it is essential to seek help and consult with a healthcare provider.
Addressing a low sperm count promptly not only enhances your chances of fertility but also helps maintain your overall health and well-being. Consulting a healthcare professional can lead to a proper diagnosis and appropriate treatment, thereby improving your reproductive health.
It’s important to remember that discussing fertility issues can be sensitive, but taking action is a positive step towards understanding and managing your health better. Do not hesitate to reach out for the support and guidance you need. Your health is invaluable, and taking the necessary steps to address any concerns, including low sperm count, is of paramount importance.
References
For additional information and validation of the details provided about low sperm count symptoms, you can refer to the following reputable sources. These references offer a deeper understanding and further exploration into the subject, ensuring that you have access to credible and well-researched information:
- Mayo Clinic – This site provides a comprehensive overview of the causes, symptoms, and treatment options for low sperm count. Read more about low sperm count on the Mayo Clinic website.
- World Health Organization (WHO) – WHO offers extensive resources and guidelines on reproductive health, including conditions affecting male fertility such as low sperm count. Explore WHO resources on male fertility.
- WebMD – A trusted resource for medical information, including detailed articles on the symptoms and impacts of low sperm count on fertility. Learn more about low sperm count at WebMD.
- National Health Service (NHS) – The NHS site provides reliable medical information and treatment guidelines for low sperm count, recognized by healthcare professionals globally. Visit the NHS page on low sperm count.
These resources are maintained by authoritative organizations in the field of health and medicine, ensuring that you receive accurate and up-to-date information.