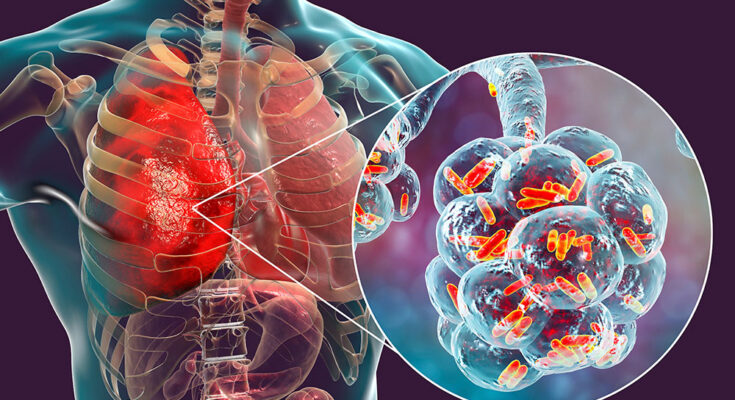
Legionnaires’ Disease Symptoms: Legionnaires’ Disease is a severe form of pneumonia caused by Legionella bacteria, which thrive in water systems including hot tubs, cooling towers, hot water tanks, and large plumbing systems.
Often misunderstood or misdiagnosed, understanding its symptoms and causes is crucial for timely and effective treatment.
Understanding Legionnaires’ Disease
Legionnaires’ disease is a severe form of pneumonia caused by the bacteria Legionella. This bacterium thrives in water systems such as hot tubs, cooling towers, hot water tanks, large plumbing systems, and decorative fountains where conditions are suitable for growth. People contract Legionnaires’ disease by inhaling aerosol droplets of water contaminated with the bacteria, not through person-to-person contact.
The History of Legionnaires’ Disease
The disease was first identified in 1976 during an outbreak at an American Legion convention in Philadelphia, hence the name “Legionnaires’.” Over 200 attendees were affected, leading to the discovery of the previously unknown bacterium. This outbreak prompted significant changes in water system management to prevent the disease.
Incidence Rates of Legionnaires’ Disease
- United States: The Centers for Disease Control and Prevention (CDC) reports approximately 10,000 cases of Legionnaires’ disease annually, but many cases go unreported, suggesting the actual number could be higher.
- Europe: The European Centre for Disease Prevention and Control (ECDC) estimates that there are about 7,000 confirmed cases each year across European Union countries.
- Global Reach: Incidence rates vary significantly worldwide, depending largely on water system maintenance and public health practices.
However, ongoing efforts to monitor water quality and educate the public on preventive measures remain key strategies in managing the risks associated with this disease.
Causes of Legionnaires’ Disease
Understanding the sources and transmission pathways of this bacteria is crucial in preventing and managing outbreaks. Here’s an in-depth look at the causes and risk factors associated with Legionnaires’ disease.
Sources of Legionella Bacteria
- Water Systems: Legionella bacteria thrive in warm water environments. Large plumbing systems, hot water tanks, decorative fountains, and hot tubs that are not properly maintained can become breeding grounds for these bacteria.
- Cooling Towers: These structures, part of the cooling systems for buildings like hotels, offices, and hospitals, can harbor Legionella if not regularly cleaned and disinfected.
- Humidifiers and Air Conditioners: Devices that use water to operate can spread contaminated mist or steam if not properly maintained.
- Medical Equipment: Equipment like respiratory machines and other hospital devices can also be sources if they are not properly sterilized.
Transmission of Legionella Bacteria to Humans
Legionella bacteria are primarily transmitted to humans when they inhale microscopic water droplets (aerosols) contaminated with the bacteria. It is important to note that Legionnaires’ disease does not spread from person to person but through inhalation of aerosols from water sources contaminated with Legionella.
Risk Factors for Contracting Legionnaires’ Disease
- Age: Individuals over 50 years are at a higher risk.
- Smoking: Current or former smokers are particularly susceptible due to decreased lung function.
- Chronic Lung Disease: People with chronic obstructive pulmonary disease (COPD) or other chronic lung conditions are more vulnerable.
- Weakened Immune System: Those with weakened immune systems, from HIV/AIDS, chemotherapy, or long-term use of corticosteroids, face a higher risk.
- Underlying Health Conditions: People with diabetes, kidney failure, or liver failure are more susceptible to infection.
By being aware of these causes and risk factors, individuals and health authorities can take proactive steps to mitigate the risk of Legionnaires’ disease through regular maintenance of water systems and adherence to safety protocols.
Symptoms of Legionnaires’ Disease
Here’s a comprehensive guide to recognizing the symptoms, understanding their progression, and knowing when to seek medical attention.
Early Symptoms of Legionnaires’ Disease
The early symptoms of Legionnaires’ disease often resemble those of the flu and can appear 2 to 10 days after exposure to the bacteria. Initially, individuals may experience:
- Headaches: A persistent and sometimes severe headache can be one of the first signs.
- Muscle aches: Unexplained muscle pain, which can be widespread or localized, is another early symptom.
- Fatigue: A noticeable feeling of tiredness or weakness that doesn’t seem to go away with rest.
- Fever: A high fever, typically above 104 degrees Fahrenheit (40 degrees Celsius), is common and can develop suddenly.
- Chills: Along with fever, chills are a frequent companion, signaling the body’s attempt to fight off infection.
These initial symptoms can easily be mistaken for those of other respiratory illnesses, which makes vigilant observation crucial.
Progression of Symptoms and Comparison to Similar Illnesses
As Legionnaires’ disease progresses, the symptoms become more pronounced and severe, typically developing into respiratory issues within a few days after the initial flu-like signs:
- Cough: A dry cough that can become productive, producing mucus or even blood.
- Shortness of breath: Difficulty breathing or shortness of breath can occur, even when resting.
- Chest pain: Pain in the chest when breathing deeply or coughing.
- Gastrointestinal symptoms: Nausea, vomiting, and diarrhea can also manifest, which are less common in other types of pneumonia.
Comparatively, while both Legionnaires’ disease and other forms of pneumonia affect the lungs, Legionnaires’ disease is more likely to involve gastrointestinal symptoms and a higher fever. The confusion and other neurological symptoms like disorientation can also be more pronounced than in typical pneumonia cases.
When to Seek Medical Attention
Immediate medical attention is essential if you suspect Legionnaires’ disease, especially if you experience the following:
- Persistent high fever and chills
- Cough with mucus or blood
- Severe chest pain or difficulty breathing
- Signs of mental confusion or changes in alertness
However, early intervention is crucial, as Legionnaires’ disease can rapidly worsen and lead to life-threatening complications like respiratory failure, kidney failure, or septic shock if not treated promptly.
Diagnosis and Detection of Legionnaires’ Disease
Identifying this disease involves a combination of medical history review, physical examinations, and specific tests. This article outlines the critical steps and procedures used in the diagnosis and detection of Legionnaires’ disease.
Tests and Procedures for Diagnosing Legionnaires’ Disease
Several tests and procedures are essential for diagnosing Legionnaires’ disease effectively:
- Urine Antigen Test: This is the most common test used to diagnose Legionnaires’ disease. It detects the presence of Legionella antigens in the urine and can provide results quickly. This test is highly specific for Legionella pneumophila serogroup 1, the most common cause of outbreaks.
- Culture of Respiratory Secretions: This test involves culturing a sample of sputum, or lung tissue if available, on a special medium that promotes the growth of Legionella bacteria. It is the gold standard for diagnosing Legionnaires’ disease as it can identify the specific species and serogroups responsible for the infection.
- Direct Fluorescent Antibody (DFA) Stain: This test uses fluorescent antibodies to stain the bacteria in a sample, allowing for the visualization of Legionella under a microscope. However, it is less commonly used due to its technical complexity and lower sensitivity compared to other tests.
- Chest X-ray: A chest X-ray is commonly performed to look for pneumonia-like signs in the lungs, which are indicative of Legionnaires’ disease.
- Polymerase Chain Reaction (PCR) Test: This test detects the DNA of Legionella bacteria in respiratory secretions. PCR testing is useful for its speed and specificity, although it is not as widely available as the urine antigen test.
The Role of Medical History and Physical Examination in Diagnosis
The initial evaluation for Legionnaires’ disease involves a detailed medical history and physical examination:
- Medical History: The doctor will ask about symptoms such as cough, shortness of breath, high fever, muscle aches, and headaches. They will also inquire about recent travel, hotel stays, or exposure to potential sources of Legionella, such as hot tubs or large plumbing systems.
- Physical Examination: During the physical examination, the doctor will listen to the patient’s lungs with a stethoscope for abnormal sounds and check for other signs of respiratory distress.
However, combining the results from these tests and procedures with the information gathered during the medical history and physical examination allows healthcare providers to make a timely and accurate diagnosis of Legionnaires’ disease.
Treatment Options for Legionnaires’ Disease
Here, we explore the most effective treatment options available for Legionnaires’ disease, emphasizing the importance of hydration and hospital care in severe cases.
Antibiotics
The primary treatment for Legionnaires’ disease is antibiotics. These medications are effective in killing the bacteria causing the infection. The choice of antibiotic often depends on the patient’s health profile and the severity of the disease. Commonly prescribed antibiotics include:
- Azithromycin: This is often the first-line treatment due to its effectiveness against Legionella bacteria.
- Levofloxacin and Moxifloxacin: These fluoroquinolones are alternatives that may be used based on the patient’s medical history and specific health needs.
- Doxycycline: This may be used as an alternative, particularly in less severe cases or when other antibiotics are not suitable.
Hospitalization
Severe cases of Legionnaires’ disease often require hospitalization. This allows for close monitoring and treatment of complications, such as respiratory failure or other organ dysfunctions. Hospital care typically includes:
- Oxygen therapy: To help maintain adequate oxygen levels in the blood.
- Intravenous (IV) antibiotics: For more effective delivery of medications.
- Respiratory support: Including assistance from ventilators in cases of severe respiratory distress.
Hydration
Hydration is a critical component of treating Legionnaires’ disease, especially given the fever and potential for severe illness associated with the infection. Proper hydration helps maintain essential bodily functions and supports the immune system in fighting the infection. Hydration can be managed through:
- Oral fluids: Encouraging the intake of water, juices, or oral rehydration solutions.
- IV fluids: For patients who cannot maintain hydration orally, especially in severe cases.
Monitoring and Supportive Care
Alongside specific treatments, supportive care plays a vital role in managing symptoms and preventing further complications. This includes:
- Regular monitoring: Vital signs, fluid status, and kidney function are monitored closely.
- Pain management: Analgesics may be used to manage pain and discomfort.
- Nutritional support: Ensuring the patient receives adequate nutrition during recovery.
It is essential for patients and healthcare providers to recognize symptoms early and initiate treatment promptly to ensure the best possible recovery.
Prevention and Risk Reduction of Legionnaires’ Disease
The bacteria thrive in warm water environments, making certain facilities particularly vulnerable. Here are essential strategies for prevention and risk reduction, targeting building owners and policymakers:
Measures to Prevent Legionnaires’ Disease
- Regular Water System Maintenance: Implement routine inspections and maintenance of all water systems, including cooling towers, hot tubs, and plumbing systems. This prevents the growth and spread of Legionella bacteria.
- Temperature Control: Ensure that water temperatures are either kept high enough (above 140°F) to kill the bacteria or low enough (below 68°F) to inhibit bacterial growth.
- Use of Biocides: Regularly apply biocides in water systems prone to Legionella outbreaks. Biocides can effectively control the population of the bacteria when used as part of a regular maintenance program.
- Flushing Water Systems: In buildings with low usage, it is crucial to regularly flush out the water system to avoid water stagnation, which promotes bacterial growth.
- Installation of Filters: Fit water systems with Legionella-specific filters, especially in areas like healthcare facilities where people with weakened immune systems may be at higher risk.
- Regular Testing for Legionella: Conduct periodic testing to detect the presence of Legionella bacteria. Early detection can prevent outbreaks by enabling timely intervention.
- Certified Legionella Risk Assessment: Engage qualified professionals to carry out a detailed risk assessment periodically or when any changes to the water system or its use occur.
Guidelines for Building Owners
- Develop a Water Safety Plan: Create and implement a comprehensive water management plan that includes procedures for regular maintenance, monitoring, and corrective actions if Legionella is detected.
- Training for Maintenance Staff: Ensure that all personnel involved in water system maintenance are trained in Legionella prevention and control strategies.
- Record Keeping: Maintain detailed records of all maintenance, inspections, and actions taken to control Legionella. This documentation can be crucial for legal and health safety requirements.
Public Health Policies
- Establishment of Health Regulations: Implement health regulations that require building owners and managers to adhere to Legionella prevention standards.
- Public Awareness Campaigns: Conduct campaigns to raise awareness about the risks of Legionnaires’ disease and the importance of prevention measures.
- Support for Research: Encourage and support research into more effective prevention technologies and strategies for controlling Legionella.
- Reporting and Tracking: Develop a system for the reporting and tracking of Legionnaires’ disease cases to monitor and respond to outbreaks more effectively.
By adhering to these preventive measures and guidelines, building owners can significantly reduce the risk of Legionnaires’ disease outbreaks, thereby safeguarding public health.
FAQs about Legionnaires’ Disease Symptoms
What are the common symptoms of Legionnaires’ disease?
Legionnaires’ disease often starts with symptoms similar to those of the flu. Common signs include high fever, chills, cough, muscle aches, and headaches. As the disease progresses, symptoms may intensify, potentially leading to pneumonia.
How quickly do symptoms of Legionnaires’ disease appear after exposure?
Symptoms typically develop 2 to 10 days after exposure to the bacteria. This period, known as the incubation period, varies slightly depending on the individual’s health and the severity of the bacterial exposure.
Can Legionnaires’ disease cause symptoms other than respiratory issues?
Yes, aside from respiratory symptoms, Legionnaires’ disease can cause gastrointestinal symptoms such as nausea, vomiting, and diarrhea. Some people may also experience confusion or changes in mental status due to the infection.
Are the symptoms of Legionnaires’ disease different in children and adults?
Symptoms of Legionnaires’ disease are generally similar in children and adults. However, children, especially those with underlying health conditions, might display symptoms more quickly and with greater severity.
What should I do if I suspect I have symptoms of Legionnaires’ disease?
If you suspect that you have symptoms of Legionnaires’ disease, especially after exposure to a potential source of Legionella bacteria, seek medical attention promptly. Early diagnosis and treatment with antibiotics are crucial for recovery.
Conclusion
Understanding the symptoms and causes of Legionnaires’ disease is crucial for prompt and effective treatment. This disease, caused by the Legionella bacteria, often manifests with flu-like symptoms, including coughing, shortness of breath, high fever, muscle pains, and headaches. Being aware of how it spreads, primarily through inhalation of contaminated water droplets, can help in preventing its onset.
If you or someone you know experiences symptoms that resemble those of Legionnaires’ disease, especially after exposure to potential sources like hot tubs, cooling towers, or complex water systems in buildings, it is vital to seek medical advice promptly.
Staying informed about this disease is key to managing its risks and impacts effectively. Always consult healthcare professionals for guidance and to ensure the right preventative measures are taken. Stay safe and stay informed!
References
For those interested in delving deeper into the topic of Legionnaires’ disease and its symptoms, the following reputable sources offer comprehensive insights and further reading. These resources have been carefully selected to ensure accurate and trustworthy information:
- Centers for Disease Control and Prevention (CDC): Explore the CDC’s extensive resources on Legionnaires’ disease for information on symptoms, causes, and prevention strategies. Learn more about Legionnaires’ disease at the CDC.
- World Health Organization (WHO): The WHO provides detailed information on the disease’s global impact, treatment options, and prevention guidelines. Read the WHO guidelines on Legionnaires’ disease.
- Mayo Clinic: Access a patient-focused overview of Legionnaires’ disease, including symptoms, diagnosis, and treatment options at the Mayo Clinic’s website. Visit the Mayo Clinic’s page on Legionnaires’ disease.
- PubMed: For those looking for more scientific detail or research studies, PubMed offers a vast database of peer-reviewed articles and studies on Legionnaires’ disease. Search for articles on Legionnaires’ disease on PubMed.
These sources are valuable for anyone seeking to understand more about Legionnaires’ disease, whether for academic purposes, professional knowledge, or personal interest. They provide a reliable foundation for further exploration of the disease’s complexities and management.