Legionnaires’ Disease Treatment: Legionnaires’ disease is a severe form of pneumonia caused by Legionella bacteria, which thrives in water systems including hot tubs, cooling towers, hot water tanks, large plumbing systems, and decorative fountains.
People contract Legionnaires’ disease by inhaling microscopic water droplets containing the bacteria. Despite being highly treatable, the disease requires prompt and effective medical attention to prevent serious complications.
What is Legionnaires’ Disease?
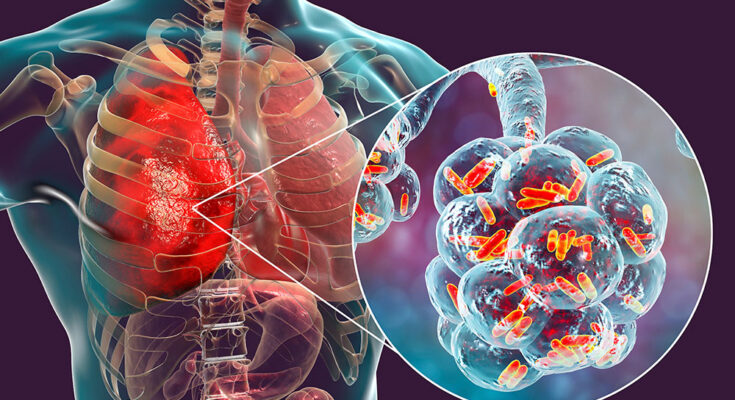
Legionnaires’ disease is a severe form of pneumonia — lung inflammation usually caused by infection. It is triggered by the bacteria Legionella pneumophila, found in both potable and non-potable water systems. Unlike the common cold or flu, which are airborne viral infections, Legionnaires’ disease does not spread from person to person. Instead, individuals contract the disease when they inhale aerosol droplets of water contaminated with the bacteria.
Causes and How It Spreads
The primary cause of Legionnaires’ disease is the Legionella bacteria, which naturally occurs in freshwater environments. However, it becomes a health concern when it grows and spreads in human-made water systems like:
- Showerheads and sink faucets
- Cooling towers (structures that contain water and a fan as part of centralized air cooling systems for building or industrial processes)
- Hot tubs that aren’t drained after each use
- Decorative fountains and water features
- Hot water tanks and heaters
- Large plumbing systems
Inhalation of aerosolized droplets containing the bacteria from these sources leads to infection. For instance, someone might inhale contaminated steam or mist from a hot tub or shower. The disease does not spread by drinking contaminated water or through direct contact with a person who is affected.
Statistics on Incidence Rates Globally and Locally
Globally, the incidence rates of Legionnaires’ disease can vary significantly, reflecting differences in climate, regulation, and water system management. In the United States, for example, the Centers for Disease Control and Prevention (CDC) reports an estimated 10,000 to 18,000 hospitalizations due to Legionnaires’ disease each year. The actual numbers may be higher due to underreporting. Incidence rates have been on the rise, with cases increasing by nearly five times since 2000.
In Europe, reported cases have also increased, with over 10,000 cases reported annually. European countries with notably higher reports include France, Germany, and Italy. This rise is attributed to better surveillance, aging populations, and perhaps more frequent travel.
Local statistics can vary even more significantly. For instance, in regions with well-maintained water systems and stringent safety regulations, such as Scandinavia, the incidence rates tend to be lower. Conversely, in areas where infrastructure is aging or maintenance is lax, outbreaks can be more frequent.
Awareness of the causes and risks associated with Legionnaires’ disease can help in the prevention and prompt treatment of this serious condition. Proper maintenance of water systems and adherence to safety regulations are crucial in controlling the spread of the disease.
Symptoms of Legionnaires’ Disease
Here’s a detailed look at the symptoms of Legionnaires’ disease, its progression, and how it differs from other respiratory conditions.
Early Symptoms to Watch For
The initial symptoms of Legionnaires’ disease can be misleadingly mild and often resemble those of the flu. Recognizing these early signs can lead to quicker diagnosis and treatment:
- High fever: This typically rises above 104 degrees Fahrenheit (40 degrees Celsius).
- Chills: Sudden chills or shivering without an apparent cause.
- Muscle aches: Unexplained muscle pain, which is often severe.
- Headaches: Persistent or severe headaches not relieved by standard painkillers.
- Fatigue: Increased tiredness that isn’t usual for the individual.
These symptoms usually begin 2 to 10 days after being exposed to the bacteria, a period known as the incubation time.
Progression of the Disease
As Legionnaires’ disease progresses, the symptoms become more pronounced and respiratory issues become apparent:
- Cough: This can be dry or produce mucus and sometimes blood.
- Shortness of breath: Difficulty breathing, which can escalate quickly.
- Chest pain: Pain when breathing deeply or coughing.
- Gastrointestinal symptoms: Nausea, vomiting, and diarrhea, which are less common but significant.
- Mental changes: Confusion or changes in mental clarity, which may indicate the severity of the infection.
Prompt medical attention is critical if these symptoms appear, especially if you suspect exposure to Legionella.
Differences Between Legionnaires’ Disease and Other Respiratory Conditions
While symptoms of Legionnaires’ disease can mimic those of other respiratory infections, there are key differences that help distinguish it:
- Cause: Unlike the common cold or flu caused by viruses, Legionnaires’ disease is caused by bacteria.
- Severity: Symptoms are typically more severe than those of a regular respiratory infection.
- Transmission: Legionnaires’ disease does not spread from person to person. Instead, it spreads through inhalation of aerosolized water droplets containing Legionella bacteria.
- Risk groups: People with compromised immune systems, chronic lung disease, or elderly individuals are more susceptible to Legionnaires’ than to the common cold or flu.
By recognizing the early signs and understanding the progression of Legionnaires’ disease, individuals can seek timely medical help, potentially mitigating the severity of the disease.
Diagnosis of Legionnaires’ Disease
Early diagnosis of Legionnaires’ disease is crucial for effective treatment and prevention of severe complications. This bacterial infection, caused by the Legionella pneumophila bacterium, primarily affects the lungs and can lead to severe pneumonia and other health issues if not addressed promptly.
Importance of Early Diagnosis
- Improves Treatment Outcomes: Early detection allows for the timely administration of appropriate antibiotics, which are most effective when started early.
- Reduces Risk of Complications: Prompt diagnosis can prevent the progression of the disease to more severe forms, such as respiratory failure, septic shock, and acute kidney failure.
- Prevents Outbreaks: Identifying the disease early can help in implementing control measures to prevent the spread of the bacteria, especially in high-risk environments like hospitals and hotels.
Common Diagnostic Tests and Procedures
- Urine Antigen Test: This is the most common test for Legionnaires’ disease. It detects the presence of Legionella antigens in the urine and can provide results quickly.
- Culture Test: This involves taking a sample from the lung (sputum) or respiratory tract and growing the bacteria in a lab to confirm the presence of Legionella.
- Serology: This test measures the body’s immune response to Legionella bacteria by detecting specific antibodies in the blood.
- Chest X-ray: Used to identify pneumonia, which is common in cases of Legionnaires’ disease, though not specific to Legionella infection.
- PCR Test: Molecular testing to detect the DNA of Legionella bacteria directly from respiratory samples, providing a highly specific diagnosis.
Challenges in Diagnosing Legionnaires’ Disease
- Similarity to Other Pneumonias: The symptoms of Legionnaires’ disease are similar to other forms of pneumonia, making it difficult to diagnose based solely on clinical presentation.
- Specialized Laboratory Tests: Many of the more definitive tests require specialized laboratory facilities not available in all hospitals.
- Variability of Symptoms: Symptoms can vary widely among individuals, ranging from mild cough and fever to severe pneumonia, complicating the diagnosis process.
- Delayed Urine Antigen Results: Although the urine antigen test is quick, it can sometimes only detect the disease several days after the onset of symptoms, potentially delaying treatment.
- Limited Sensitivity and Specificity: Some tests may not detect all strains of Legionella or can occasionally give false positive results, especially in populations with low disease prevalence.
Proper and prompt diagnostic measures are essential for effectively managing Legionnaires’ disease, ensuring better health outcomes, and preventing wider outbreaks.
Treatment Options for Legionnaires’ Disease
Effective treatment is crucial for recovery, especially since this infection can be severe, particularly in older adults, smokers, or those with weakened immune systems. Here, we explore the comprehensive treatment strategies for managing and overcoming Legionnaires’ disease.
General Approach to Treatment
The primary treatment for Legionnaires’ disease is antibiotics. Since it’s a bacterial infection, prompt antibiotic therapy is critical and can significantly influence outcomes. The choice of antibiotic and the mode of administration (oral or intravenous) depend on the severity of the symptoms and the patient’s overall health. Commonly used antibiotics include:
- Macrolides: such as azithromycin, which is often preferred for its effectiveness and minimal side effects.
- Fluoroquinolones: such as levofloxacin and moxifloxacin, which are used for their broad range of activity against bacteria.
- Tetracyclines: doxycycline may also be used, particularly in cases involving antibiotic resistance.
Early diagnosis and treatment initiation are essential to reduce the risk of complications and improve survival rates.
Supportive Treatments in Hospitals
Patients with severe cases of Legionnaires’ disease often require hospitalization. In a hospital setting, supportive treatments are critical to assist the body in fighting off the infection and to manage symptoms. These may include:
- Oxygen therapy: to help maintain oxygen levels in the blood, especially if the patient is experiencing breathing difficulties.
- Intravenous (IV) fluids: to prevent dehydration and maintain electrolyte balance.
- Respiratory support: including ventilation support for patients who cannot breathe adequately on their own.
- Monitoring and managing complications: such as kidney failure or septic shock, which can occur in severe cases.
Duration of Treatment and Follow-up Care
The duration of antibiotic treatment for Legionnaires’ disease typically ranges from 5 to 14 days but may vary based on the individual’s response to treatment and the severity of the disease. Follow-up care is crucial to ensure complete recovery and to monitor for any potential complications. This might include:
- Follow-up appointments: to assess recovery progress and to adjust treatment plans as needed.
- Chest X-rays: to confirm that the infection has been cleared.
- Monitoring for lingering symptoms: such as fatigue or difficulty breathing, which can persist even after the infection is resolved.
By adhering to these treatment protocols, healthcare providers can significantly improve patient outcomes in cases of Legionnaires’ disease, emphasizing the importance of timely and effective treatment strategies.
Complications and Risks of Legionnaires’ Disease
Understanding these complications and the risk factors that can exacerbate the severity of the disease is crucial for both patients and healthcare providers.
Common Complications from Untreated or Late-Treated Legionnaires’ Disease
- Respiratory Failure: This is one of the most serious complications, where the lungs are unable to provide enough oxygen to the body or remove enough carbon dioxide.
- Septic Shock: This occurs when Legionnaires’ disease leads to a severe and widespread infection that causes dangerously low blood pressure and organ failure.
- Acute Kidney Failure: The kidneys may be unable to filter waste from the blood, which can be life-threatening if not promptly treated.
- Endocarditis: An infection of the inner lining of the heart that can damage heart valves and impact heart function.
Risk Factors That Can Exacerbate Disease Severity
Several factors can increase the severity of Legionnaires’ disease, including:
- Age: Individuals over the age of 50 are more susceptible to severe infections.
- Smoking: Current or former smokers may have compromised lung function, which can worsen the disease’s impact.
- Chronic Lung Disease: Conditions like COPD or asthma can make patients more vulnerable to severe respiratory complications.
- Weakened Immune System: Those with weakened immune systems, due to conditions such as HIV/AIDS, cancer treatments, or organ transplants, are at higher risk of severe disease.
- Underlying Medical Conditions: Diabetes, kidney failure, or liver failure can exacerbate the effects of the disease.
Long-term Outlook for Patients
The long-term outlook for patients with Legionnaires’ disease varies based on the severity of the disease and the timeliness of treatment. Patients who receive prompt and effective treatment typically recover completely, but some may experience lingering effects, such as fatigue and respiratory issues. Early detection and management are key to preventing severe complications and improving the long-term health outcomes for patients with Legionnaires’ disease.
By recognizing the potential complications and understanding the risk factors associated with Legionnaires’ disease, individuals can seek timely medical attention, thereby reducing the risk of severe health outcomes.
Preventing Legionnaires’ Disease
Here’s a comprehensive guide on how to prevent this disease through strategic measures, role of water system management, and adherence to the latest guidelines and practices.
Strategies for Prevention in Communities and Healthcare Settings
- Regular Water System Maintenance: Ensuring that all water systems, including cooling towers, hot tubs, and large plumbing systems, are properly maintained and regularly disinfected can significantly reduce the risk of Legionella growth.
- Temperature Control: Legionella bacteria thrive in water temperatures between 20°C and 50°C. Maintaining hot water temperatures at or above 60°C and cold water temperatures below 20°C helps prevent the bacteria from multiplying.
- Avoid Stagnation: Ensure that water does not stagnate within the plumbing systems. Regularly flush out seldom-used taps and showerheads, and eliminate dead ends in piping where water can stagnate.
- Use of Disinfectants: Chlorine and other biocides are effective in killing Legionella bacteria. Regularly applying these disinfectants in appropriate concentrations can help maintain a safe water system.
- Risk Assessments and Training: Conducting routine risk assessments to identify potential sources of Legionella and training staff on prevention strategies are crucial, especially in healthcare settings where individuals are more vulnerable.
Role of Water System Management in Prevention
Effective water system management is critical in preventing Legionnaires’ disease. This involves:
- System Design and Maintenance: Design water systems to minimize areas where stagnant water might collect. Regular maintenance and cleaning of water tanks, pipes, and faucets are essential to prevent biofilm (where bacteria can grow) from developing.
- Implementation of a Water Safety Plan: Develop and implement a comprehensive water safety plan that includes risk identification, management procedures, monitoring, and contingency plans to respond to Legionella detections.
Latest Guidelines and Practices for Prevention
Staying updated with the latest guidelines and practices is essential for preventing Legionnaires’ disease effectively. Key guidelines include:
- CDC Guidelines: The Centers for Disease Control and Prevention (CDC) offers extensive resources on managing building water systems to prevent Legionella outbreaks.
- ASHRAE Standard 188: Developed by the American Society of Heating, Refrigerating and Air-Conditioning Engineers, this standard provides critical guidelines on risk management for building water systems, especially concerning Legionella.
- WHO Guidelines: The World Health Organization provides international guidelines focusing on the safety of drinking-water, which includes measures to control Legionella in various water systems.
By taking proactive measures and following the latest recommendations, communities and healthcare facilities can significantly mitigate the risk posed by this dangerous bacteria.
FAQs about Legionnaires’ Disease Treatment
What is the primary treatment for Legionnaires’ disease?
The primary treatment for Legionnaires’ disease is antibiotics. Doctors typically prescribe antibiotics such as azithromycin, levofloxacin, or doxycycline to combat the Legionella bacteria responsible for the illness. Early diagnosis and prompt treatment are crucial to improve recovery outcomes.
How long does treatment for Legionnaires’ disease last?
The duration of antibiotic treatment for Legionnaires’ disease can vary but typically ranges from 5 to 14 days, depending on the severity of the infection and the patient’s overall health. It’s essential for patients to complete the full course of antibiotics even if they start feeling better sooner.
Can Legionnaires’ disease be treated at home?
Mild cases of Legionnaires’ disease may be treated at home with oral antibiotics. However, more severe cases require hospitalization, where patients might receive antibiotics intravenously and support for any complications like respiratory distress or organ failure.
Is there a vaccine for Legionnaires’ disease?
Currently, there is no vaccine available for Legionnaires’ disease. The best prevention involves controlling the environments where the Legionella bacteria thrive, such as water systems in large buildings, to reduce the risk of outbreaks.
What should I do if I think I have been exposed to Legionnaires’ disease?
If you believe you have been exposed to Legionnaires’ disease, especially if you experience symptoms such as high fever, chills, cough, muscle aches, and headaches, you should seek medical attention promptly. Early diagnosis and treatment are vital for effective recovery.
Conclusion
In summary, diagnosing and treating Legionnaires’ disease efficiently requires a keen understanding of its symptoms, such as high fever, cough, and muscle aches, along with specialized tests like urine antigen tests and chest X-rays. The disease is treatable with antibiotics, but early intervention is crucial for effective management.
If you suspect you or someone you know may be exhibiting symptoms of Legionnaires’ disease, it is essential to seek professional healthcare advice promptly. Delaying consultation can lead to severe complications, making timely medical attention critical.
Moreover, prevention plays a pivotal role in controlling the spread of this disease. Ensuring proper maintenance of water systems in buildings and adopting safety measures in facilities with susceptible water environments can significantly reduce the risk of outbreaks. Awareness and proactive prevention are key to safeguarding public health against Legionnaires’ disease. By staying informed and vigilant, individuals and healthcare providers can work together to combat the spread of this serious illness.
References
For those seeking further information on Legionnaires’ disease and its treatments, the following sources are highly recommended. Each offers reliable and comprehensive insights that are pivotal for understanding the complexities of managing this serious illness:
- Centers for Disease Control and Prevention (CDC) – The CDC provides detailed guidelines on the identification, treatment, and prevention of Legionnaires’ disease. This resource is invaluable for healthcare professionals and the public seeking current and authoritative information. Visit CDC’s Legionnaires’ Disease Page.
- World Health Organization (WHO) – WHO offers a global perspective on the spread and control of Legionnaires’ disease, including data on outbreaks and international public health strategies. Their documentation is essential for understanding the worldwide impact of the disease. Read more at WHO’s website.
- Mayo Clinic – As a leading healthcare provider, the Mayo Clinic offers a thorough overview of the symptoms, causes, diagnosis, and treatment of Legionnaires’ disease. This resource is excellent for patients and families looking for accessible, medically reviewed information. Explore Mayo Clinic’s Legionnaires’ Disease Resource.
- PubMed Central – For those interested in the scientific and medical research aspects of Legionnaires’ disease, PubMed Central provides access to numerous scholarly articles and research papers. This is a crucial resource for understanding the latest developments in treatment and epidemiology. Access Research on Legionnaires’ Disease at PubMed Central.
These resources are instrumental in offering credible information and the latest research on Legionnaires’ disease, supporting both the general public and healthcare professionals in their efforts to understand and combat this health threat.