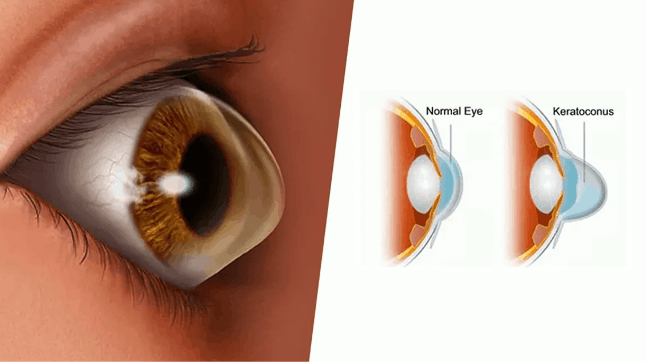
Keratoconus Treatment: Keratoconus is a progressive eye disorder where the normally round cornea thins and begins to bulge into a cone-like shape.
This deformation deflects light as it enters the eye on its way to the light-sensitive retina, causing distorted vision.
Typically manifesting in the teenage years or early twenties, the condition can cause significant visual impairment if not properly managed.
What is Keratoconus?
Keratoconus is a progressive eye disease where the normally round cornea thins and begins to bulge into a cone-like shape. This deformation deflects light as it enters the eye, leading to distorted vision. It is typically diagnosed in the teen or early adult years and can affect one or both eyes. Over time, keratoconus can lead to significant visual impairment if not managed effectively.
Epidemiology and At-Risk Populations
Keratoconus is relatively rare, affecting approximately 1 in 2,000 people worldwide. It generally begins to manifest in adolescence or early adulthood. There is no significant difference in prevalence between genders, though some studies suggest a slightly higher incidence in certain ethnic groups, such as South Asians and Middle Eastern populations.
Factors that increase the risk of developing keratoconus include:
- Genetic predisposition: Family history of keratoconus increases the likelihood of developing the condition.
- Environmental factors: Chronic eye rubbing and exposure to ultraviolet rays are believed to contribute to its progression.
- Associated conditions: Individuals with certain allergic conditions, like asthma and eczema, are also found to be at higher risk.
Symptoms and Signs of Keratoconus
The symptoms of keratoconus can vary as the disease progresses but typically include:
- Blurred or distorted vision: As the cornea begins to bulge, vision becomes progressively more distorted and blurred.
- Increased light sensitivity: Individuals may experience discomfort in bright light or see halos around lights, especially at night.
- Frequent changes in eyeglass prescription: As the shape of the cornea changes, there is often a need for frequent updates in prescription lenses.
- Sudden worsening or clouding of vision: In advanced cases, the cornea may swell rapidly, causing sudden visual impairment.
However, recognizing the signs and symptoms early is crucial for managing keratoconus effectively and can help prevent more severe vision loss.
Diagnosing Keratoconus
Early diagnosis is crucial for managing the condition effectively. Below, we explore the diagnostic criteria, essential tests and procedures, and the importance of differential diagnosis for keratoconus.
Diagnostic Criteria for Keratoconus
The diagnosis of keratoconus is primarily based on clinical findings and characteristic changes in the corneal structure. The key criteria include:
- Thinning of the Cornea: Progressive thinning leading to a cone-shaped bulge.
- Irregular Corneal Topography: Demonstrated by imaging techniques, showing a distorted corneal surface.
- Scissoring of the Retinoscopic Reflex: Observed during eye examination, indicating irregular curvature.
- Visual Distortion: Increased astigmatism and myopia, and symptoms such as ghosting, multiple images, glare, halos, and starbursts.
Diagnostic Tests and Procedures
Accurate diagnosis of keratoconus involves several tests to assess the shape, curvature, and thickness of the cornea:
- Corneal Topography: The most definitive test, providing detailed mapping of the cornea’s surface curvature. This helps in identifying early signs of keratoconus not visible through routine examinations.
- Corneal Tomography: Offers a three-dimensional map of the cornea, including the back surface, which is vital for diagnosing early-stage keratoconus.
- Pachymetry: Measures the thickness of the cornea, crucial for detecting thinning associated with keratoconus.
- Computerized Videokeratography: Allows detailed visualization of the cornea’s shape changes over time, aiding in monitoring the progression of the disease.
- Slit-Lamp Examination: A microscope examination to inspect the cornea, iris, and lens for any structural abnormalities.
Importance of Differential Diagnosis
Differential diagnosis is vital in the evaluation of keratoconus to exclude other conditions that can mimic its symptoms, such as:
- Corneal dystrophies: A group of genetic eye disorders that can cause similar corneal changes.
- Pellucid marginal degeneration: Characterized by thinning of the lower cornea, similar to keratoconus but typically in a different pattern.
- Contact lens-induced corneal warpage: Temporary changes in corneal shape due to long-term contact lens wear.
Accurately distinguishing keratoconus from these and other conditions ensures appropriate management and therapy, preventing unnecessary interventions and focusing on the specific needs of the patient.
By adhering to these diagnostic practices, healthcare providers can effectively diagnose and manage keratoconus, improving patient outcomes through tailored treatments and regular monitoring.
Advancements in Keratoconus Diagnosis
Keratoconus is a progressive eye disease that can lead to severe vision impairment if not detected and managed properly. Recent advancements in diagnostic technology have significantly improved the ability to diagnose this condition early and accurately. This section explores the latest tools in keratoconus diagnosis and the benefits of early and precise detection.
Recent Technological Advancements in Diagnostic Tools
- Corneal Topography: Advanced corneal topography systems now offer detailed mapping of the cornea’s surface curvature. This technology helps in detecting subtle corneal changes that indicate the early stages of keratoconus.
- High-Resolution Optical Coherence Tomography (OCT): OCT provides high-resolution images of the corneal structure, allowing for precise measurements of corneal thickness and detailed visualization of the corneal layers, which are crucial in diagnosing keratoconus and monitoring its progression.
- Wavefront Aberrometry: This technology measures how light waves travel through the eye, detecting irregularities that might be caused by keratoconus. It helps in customizing vision correction solutions as the disease progresses.
- Scheimpflug Imaging: A diagnostic tool that uses a rotating camera to create three-dimensional images of the anterior eye segment, providing detailed analysis of the cornea, which is essential for early detection of keratoconus.
- Artificial Intelligence (AI) and Machine Learning: AI algorithms are being developed to analyze data from imaging tests more quickly and accurately. This can lead to earlier detection of keratoconus, even before clinical symptoms appear.
Benefits of Early and Accurate Diagnosis in the Management of Keratoconus
- Improved Treatment Outcomes: Early diagnosis allows for interventions such as corneal cross-linking or specialized contact lenses to slow or even halt the progression of the disease, leading to better long-term visual outcomes.
- Customized Management Plans: Accurate diagnosis helps in tailoring treatment plans that are specific to the severity and progression of keratoconus in each individual, enhancing the effectiveness of the treatments.
- Prevention of Severe Vision Loss: By detecting keratoconus in its early stages, it is possible to implement preventive measures before significant vision loss occurs.
- Enhanced Patient Comfort: Early and precise diagnosis often leads to less invasive treatments, which can significantly improve patient comfort and reduce the need for more radical interventions like corneal transplants.
- Cost-Effectiveness: Early intervention can reduce the overall cost of managing keratoconus by minimizing the need for more complex surgeries and frequent changes in vision correction prescriptions.
The continuous evolution of diagnostic technologies not only enhances the ability to manage keratoconus effectively but also contributes to broader advancements in ophthalmic care, ensuring better vision health for patients.
Treatment Options for Keratoconus
Fortunately, several treatment options are available, ranging from non-surgical methods to more invasive surgical procedures. The choice of treatment depends on the severity of the condition and the specific needs of the patient.
Non-Surgical Treatments
Non-surgical treatments for keratoconus are primarily aimed at improving vision and managing mild to moderate symptoms. These options include:
- Eyeglasses or Soft Contact Lenses: In the early stages of keratoconus, standard eyeglasses or soft contact lenses may be sufficient to correct mild refractive errors caused by the cornea’s changing shape.
- Hard Contact Lenses: As the condition progresses, soft lenses may no longer provide adequate vision correction. Rigid gas permeable (RGP) contact lenses are often recommended because they maintain a more regular shape over the cornea, thereby providing clearer vision than soft lenses.
- Hybrid Contact Lenses: These lenses have a rigid center and a soft outer ring. Hybrid lenses offer the visual clarity of hard lenses with a comfort level closer to that of soft lenses, suitable for those who find RGPs uncomfortable.
- Scleral and Semi-Scleral Lenses: Larger in diameter than typical contact lenses, scleral and semi-scleral lenses rest on the sclera, the white part of the eye, rather than the cornea. This design can be more comfortable for people with keratoconus and provides excellent vision correction.
- Collagen Cross-Linking (CXL): This relatively new non-surgical treatment helps to strengthen the corneal tissue to halt the progression of keratoconus. During the procedure, vitamin B2 (riboflavin) is applied to the cornea, which is then activated by ultraviolet light.
Surgical Treatments
Surgical options are considered when keratoconus progresses to a stage where vision can no longer be adequately corrected with lenses, or if the patient cannot tolerate contact lenses. Surgical treatments include:
- Corneal Inserts or Intacs: These are small plastic rings inserted into the mid layer of the cornea to help flatten the corneal shape, thereby improving vision. Intacs may be recommended when contact lenses fail to provide adequate vision correction or become uncomfortable.
- Corneal Transplant: In severe cases, when the cornea becomes extremely thin or scarred, a corneal transplant may be necessary. This involves replacing the damaged cornea with healthy donor tissue.
- Topography-Guided Conductive Keratoplasty: This is a less common procedure where radiofrequency energy is applied to specific areas of the cornea to reshape it. This technique is generally used for less advanced cases of keratoconus.
- Mini Asymmetric Radial Keratotomy (MARK): This is a newer surgical method that involves making precise radial cuts in the cornea to improve its shape and stability.
By understanding the range of treatment options available, patients with keratoconus can make informed decisions in consultation with their eye care professionals to manage their condition effectively.
Choosing the Right Treatment for Keratoconus
Selecting the appropriate treatment for keratoconus is crucial and depends on several factors that ensure the management of the condition is as effective as possible. Here’s how you can make an informed decision about the right treatment path.
Factors Influencing Treatment Decisions
- Severity of the Condition: The stage of keratoconus greatly influences the treatment approach. In early stages, eyeglasses or soft contact lenses might be sufficient to correct vision. As the condition progresses, rigid gas permeable (RGP) contact lenses, or advanced therapies such as corneal cross-linking, might be required to slow the progression and improve vision.
- Patient’s Lifestyle: The daily activities and lifestyle of the patient play a significant role in selecting an appropriate treatment. For example, individuals involved in physical activities or those with a highly active lifestyle might find it challenging to manage RGP lenses and might prefer other treatment options that fit their lifestyle better.
- Patient’s Preferences and Expectations: Understanding the patient’s expectations and their readiness to comply with certain treatments, such as the frequent follow-up visits required with contact lenses, is essential. Patients need to be comfortable with their chosen method of treatment to ensure consistency and effectiveness in managing keratoconus.
Role of Ophthalmologists and Patient Discussions
The dynamic between the patient and the ophthalmologist is pivotal in managing keratoconus effectively. Here’s how this relationship facilitates the selection of the right treatment:
- Educational Role: Ophthalmologists play a critical role in educating patients about keratoconus, the implications of various treatments, and the progression of the condition. This information helps patients make informed decisions about their treatment options.
- Tailored Recommendations: Based on a detailed examination and considering the factors mentioned above, ophthalmologists can tailor their recommendations to best suit the individual needs of the patient.
- Ongoing Dialogue: Continuous communication between the patient and the ophthalmologist is crucial. Treatment effectiveness should be monitored, and adjustments should be made as the condition evolves or as the patient’s lifestyle changes.
However, choosing the right treatment for keratoconus involves a comprehensive understanding of the condition, careful consideration of the patient’s lifestyle, and active participation in discussions with an ophthalmologist.
Living with Keratoconus
Understanding how to manage the condition through lifestyle adjustments and regular medical care can help maintain vision and improve overall well-being.
Lifestyle Adjustments for Managing Symptoms
- Protect Your Eyes – Wear sunglasses to protect your eyes from UV rays and minimize further damage to the cornea.
- Use Appropriate Eyewear – Utilize prescribed corrective lenses or contact lenses as recommended by your eye care professional to correct vision changes and improve sight.
- Maintain a Healthy Diet – A diet rich in antioxidants (like vitamins A, C, and E) may contribute to eye health. Omega-3 fatty acids, often found in fish and flaxseeds, can also support eye function.
- Avoid Eye Rubbing – Rubbing your eyes can exacerbate the thinning of the corneal tissue and worsen keratoconus symptoms. It’s essential to break this habit to prevent progression of the disease.
- Create an Eye-friendly Environment – Adjust the lighting and screen settings on digital devices to reduce eye strain. Use humidifiers if needed to ensure your environment is not too dry, as dryness can irritate the eyes.
Importance of Regular Check-ups and Patient Education
- Early Detection and Monitoring – Regular visits to an eye care professional are crucial for monitoring the progression of keratoconus. Early detection can lead to more effective management strategies and potentially slow the progression through interventions like corneal cross-linking.
- Adaptation of Corrective Measures – As the condition progresses, your vision needs will change. Regular check-ups ensure that any necessary adjustments to your corrective lenses are made so that you can maintain the best possible vision.
- Patient Education – Understanding keratoconus and its impact on vision allows patients to make informed decisions about their treatment options. Education about the disease can reduce anxiety and empower patients to take active roles in their eye health.
Managing keratoconus effectively involves a combination of lifestyle adjustments and regular eye care. By taking proactive steps and staying informed, individuals with keratoconus can lead a more comfortable and productive life.
Conclusion
Regular visits to an eye care specialist are crucial for managing keratoconus effectively. By catching symptoms early and following a personalized treatment plan, patients can maintain better vision and overall eye health. It’s important to consult with eye care professionals who specialize in corneal diseases to receive the most accurate diagnosis and advanced treatment options.
Continued research in the field of keratoconus treatment is vital. Each breakthrough not only enhances our understanding of the disease but also leads to innovative treatments that can significantly improve patients’ quality of life. Staying informed about these developments can provide patients with the most effective strategies for managing their condition.
We encourage anyone experiencing changes in their vision or eye health to seek prompt and professional care. Protecting your vision begins with proactive and informed decisions about eye care.
References
For those seeking more in-depth information on keratoconus treatment and to verify the details discussed, here are several reputable sources that provide further reading and valuable insights:
- National Keratoconus Foundation – An extensive resource for understanding keratoconus, offering updates on the latest treatments and research. Learn more about managing this condition at National Keratoconus Foundation.
- American Academy of Ophthalmology – Find comprehensive articles and patient guides on the treatment options available for keratoconus, including the effectiveness and risks associated with each treatment. Visit American Academy of Ophthalmology for detailed patient education materials.
- Mayo Clinic – The Mayo Clinic provides a detailed overview of keratoconus, symptoms, and advancements in treatment techniques. Their resource is an excellent starting point for patients and healthcare providers alike. Access their materials at Mayo Clinic Keratoconus Treatment.
- PubMed Central – For academic research articles and clinical studies on keratoconus, PubMed Central offers a wealth of peer-reviewed papers. Explore the latest findings and historical data at PubMed Central.
Each of these sources is authoritative and provides extensive information that can help patients and their families better understand keratoconus and its current treatment protocols. Whether you are a patient seeking more information or a health professional looking to stay updated on the latest trends, these resources are invaluable.