Ischemic Colitis Symptoms: Ischemic colitis occurs when blood flow to a part of the large intestine (colon) is temporarily reduced.
This condition is predominantly observed in older individuals but can affect anyone. It often causes pain and can lead to severe health issues, including colon damage.
Understanding the symptoms and causes of ischemic colitis is crucial for timely diagnosis and management.
Understanding Ischemic Colitis
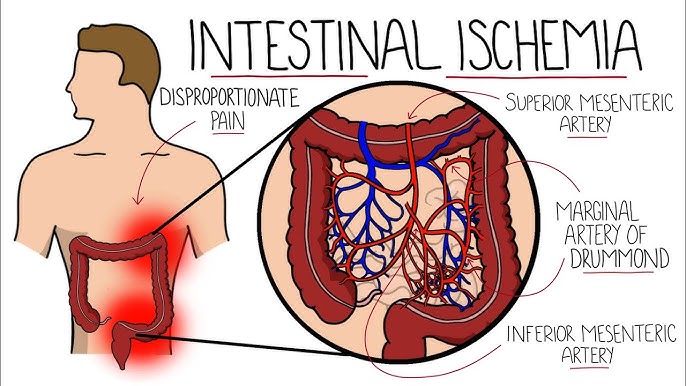
Ischemic colitis occurs when there is a temporary reduction in blood flow to the colon, leading to inflammation and injury of the large intestine. This condition can vary in severity, often causing pain and leading to complications if not promptly treated. Understanding how ischemic colitis differs from other forms of colitis, and looking at its prevalence, can help in recognizing and managing this condition effectively.
How It Differs from Other Forms of Colitis
Ischemic colitis stands out from other types of colitis in several key ways:
- Cause: Unlike ulcerative colitis and Crohn’s disease, which are caused by immune system dysfunction, ischemic colitis is primarily caused by reduced blood flow to the colon, often due to blood vessel constriction or blockage.
- Age of Onset: Ischemic colitis more commonly affects older adults, typically those over 60, whereas other types like ulcerative colitis can begin in younger adults or even teenagers.
- Symptoms: The symptoms of ischemic colitis such as sudden abdominal pain, rectal bleeding, and an urgent need to defecate are similar to other forms of colitis but often come on suddenly and can resolve quickly if blood flow is restored.
- Diagnosis: Diagnosis of ischemic colitis often involves imaging studies like a CT scan to observe blood flow to the colon, distinguishing it from other types which may require colonoscopy and biopsy.
Statistics on Prevalence
Ischemic colitis is relatively common among gastrointestinal disorders, especially in the elderly. Here are some key statistics:
- Age Group: Over 90% of cases occur in people over the age of 60.
- Incidence Rate: It is estimated that ischemic colitis affects about 4.5 to 44 cases per 100,000 people per year.
- Gender Disparity: Women are slightly more likely to develop ischemic colitis than men.
- Recovery: Approximately 80% of patients recover with conservative treatment, but severe cases can require surgery.
However, understanding these differences and statistics can aid in the early recognition and treatment of ischemic colitis, potentially preventing more severe outcomes. Awareness and timely medical consultation are crucial, particularly for those in higher-risk groups.
Causes of Ischemic Colitis
Understanding the primary causes and risk factors is essential for both prevention and early treatment.
Primary Causes of Reduced Blood Flow Leading to Ischemic Colitis
- Atherosclerosis: The most common cause of reduced blood flow to the colon is atherosclerosis, where plaque builds up in the arteries, narrowing them and limiting blood flow.
- Blood Clots: Blood clots can block an artery, severely reducing or cutting off blood supply to part of the colon.
- Low Blood Pressure: Severe drops in blood pressure, which may occur during surgery, with heart failure, or other conditions, can reduce blood flow to the intestine.
- Vascular Disease: Diseases that cause inflammation and narrowing of blood vessels, like vasculitis or radiation arteritis, can lead to ischemic colitis.
- Surgical Procedures: Certain types of abdominal surgeries can inadvertently impair blood flow to the colon.
Risk Factors Enhancing the Likelihood of Developing Ischemic Colitis
- Age: People over the age of 60 are at higher risk for ischemic colitis because blood flow to the colon naturally decreases with age.
- Certain Medications: Some medications, including hormone replacements, nonsteroidal anti-inflammatory drugs (NSAIDs), and some heart and migraine medications, can increase the risk of ischemic colitis by affecting blood flow or causing dehydration.
- Medical Conditions: Conditions such as diabetes, high cholesterol, and heart disease increase the risk of atherosclerosis, which in turn can lead to ischemic colitis.
- Dehydration: Severe dehydration can thicken blood and slow down blood circulation, increasing the risk of reduced blood flow to the colon.
- Physical Activity: Extreme physical exertion, especially in unfavorable conditions, can divert blood flow away from the colon to more critical organs like the heart and brain.
However, regular check-ups and consultations with healthcare providers are crucial, especially for those with heightened risk profiles.
Symptoms of Ischemic Colitis
Ischemic colitis, a medical condition characterized by reduced blood flow to the colon, manifests through various symptoms that can range from mild to severe. Understanding these symptoms is crucial for timely diagnosis and treatment.
Common Symptoms
The most frequently observed symptoms of ischemic colitis include:
- Abdominal Pain: Typically, the pain is sudden and may be accompanied by cramping. It often occurs on the left side of the abdomen but can be felt throughout the abdominal area.
- Blood in Stool: This is a hallmark symptom, where the stool may appear bright red or maroon, indicating fresh bleeding.
- Diarrhea: Loose and frequent stools are common, and they may include blood.
- Urgency to Defecate: A persistent need to pass a bowel movement, often unsuccessfully, can occur.
- Bloating and Nausea: Patients may experience general abdominal discomfort, including bloating and nausea.
Variability of Symptoms
The severity and presentation of symptoms can vary widely from one individual to another, influenced by the extent of the colon affected and the speed at which the condition progresses. Some patients might experience mild symptoms that resolve quickly without treatment, while others may have severe and persistent symptoms that require immediate medical attention.
Signs of Severe Cases and Complications
Recognizing signs of severe ischemic colitis and its potential complications is vital for preventing irreversible damage. These signs include:
- Severe Pain: Intense abdominal pain that does not improve may indicate that the colon tissue is severely damaged and could be dying.
- Persistent Bleeding: Continuous or heavy bleeding from the rectum is a serious concern, suggesting significant damage to the colon.
- Fever and Chills: These symptoms suggest an infection, which could be a complication of ischemic colitis.
- Rapid Heart Rate: A suddenly elevated heart rate can be a response to internal bleeding or infection.
- Low Blood Pressure: This might indicate shock, especially if accompanied by clammy skin, dizziness, or fainting.
If you notice any of these severe symptoms or suspect ischemic colitis, seek immediate medical attention to mitigate risks and manage the condition effectively.
Diagnosing Ischemic Colitis
The diagnosis of ischemic colitis involves a combination of clinical evaluation, imaging studies, and laboratory tests. Understanding the pivotal role of medical history and the various diagnostic methods can guide healthcare providers to a correct diagnosis, thereby optimizing patient outcomes.
List of Diagnostic Methods for Ischemic Colitis
1. Clinical Assessment: The initial step in diagnosing ischemic colitis involves a thorough clinical evaluation by a healthcare provider. Symptoms such as abdominal pain, blood in the stool, and urgent bowel movements are key indicators that may suggest ischemic colitis.
2. Blood Tests: Blood tests are crucial in the diagnostic process. They help to assess the overall health of the patient and can indicate inflammation or infection. Elevated white blood cell counts, for example, are common in patients with ischemic colitis.
3. Imaging Studies:
- Computed Tomography (CT) Scan: A CT scan of the abdomen is one of the most effective imaging methods for diagnosing ischemic colitis. It provides detailed images of the colon and can highlight areas with reduced blood flow and inflammation.
- Colonoscopy: This procedure allows direct visualization of the inner walls of the colon. It can detect the extent of ischemia and differentiate ischemic colitis from other forms of inflammatory bowel disease.
- Ultrasound: In some cases, an ultrasound can be used to evaluate blood flow in the abdominal arteries and veins.
4. Stool Tests: Analyzing stool samples can help rule out infections caused by bacteria or viruses, which can mimic the symptoms of ischemic colitis.
The Role of Medical History in Diagnosing Ischemic Colitis
The medical history of a patient is a cornerstone in diagnosing ischemic colitis. A comprehensive medical history can provide clues that point towards ischemia as a cause of colonic symptoms. Important factors include:
- Age and Pre-existing Conditions: Ischemic colitis is more common in the elderly and those with cardiovascular diseases, such as atherosclerosis or heart failure.
- Medication History: Some medications, especially those that constrict blood vessels or promote clotting, can increase the risk of ischemic colitis.
- Previous Episodes: A history of similar symptoms can suggest a recurrent pattern, indicative of ongoing issues with intestinal blood flow.
By integrating information from medical history with clinical and diagnostic findings, healthcare providers can effectively diagnose ischemic colitis, distinguishing it from other gastrointestinal disorders and ensuring that patients receive the most appropriate treatments.
Treatment and Management of Ischemic Colitis
Managing this condition effectively is crucial to prevent complications and improve quality of life. This article explores the various treatment options, lifestyle changes, and the significance of medical supervision and regular check-ups.
List of Treatment Options
The treatment for ischemic colitis is primarily based on the severity of the condition. Here are the most common approaches:
1. Medications:
- Antibiotics are often prescribed to prevent infections if necrosis (tissue death) is suspected.
- Vasodilators help widen blood vessels and improve blood flow to the affected area.
- Anti-inflammatory drugs can help reduce colon inflammation.
2. Intravenous Fluids: For severe dehydration, fluids are administered intravenously to help maintain fluid balance and support blood pressure.
3. Surgery: In cases where there is significant damage to the colon, surgery might be required to remove the affected part of the colon. Surgical intervention is also considered if there is a persistent risk of complications like perforation or gangrene.
4. Thrombolytic Therapy: This is used to dissolve blood clots that might be restricting blood flow to the colon, although it’s not commonly applied to all ischemic colitis cases.
Lifestyle Changes and Home Remedies
Managing ischemic colitis often involves making several lifestyle adjustments to help reduce symptoms and prevent recurrence:
- Diet: Adopting a diet low in residue can help minimize the workload on your colon. Foods that are easy to digest, such as cooked vegetables, fruits without skin or seeds, and lean meats are recommended.
- Hydration: Increasing fluid intake helps prevent dehydration and maintains proper digestion.
- Avoid Smoking: Smoking can constrict blood vessels and worsen blood flow, thereby increasing the risk of ischemic colitis.
- Stress Management: Techniques such as yoga, meditation, or therapy can reduce stress, which may indirectly benefit your colon health.
Importance of Medical Supervision and Regular Check-Ups
Regular follow-ups with a healthcare provider are essential in managing ischemic colitis effectively. These check-ups help in:
- Monitoring the condition: Regular assessments can help monitor the progress of the disease and the effectiveness of the treatment plan.
- Adjusting treatment: Depending on how the condition evolves, medications or dietary recommendations may need to be adjusted.
- Early detection of complications: Frequent monitoring allows for the early detection of potential complications, which can be critical in preventing severe outcomes.
Ischemic colitis requires a well-rounded approach that combines medical treatment, lifestyle adjustments, and ongoing care. With the right management strategies, individuals can lead a comfortable life and significantly reduce the risks associated with this condition.
Preventing Ischemic Colitis
Fortunately, adopting certain preventive measures can significantly lower the risk. Below, we explore effective lifestyle modifications, the crucial role of diet and exercise, and the importance of regular medical assessments for at-risk individuals.
Lifestyle Modifications
- Quit Smoking: Smoking is a major risk factor for reduced blood flow and can exacerbate ischemic conditions. Quitting smoking improves overall vascular health and reduces the risk of ischemic colitis.
- Manage Stress: Chronic stress can affect blood flow and contribute to various health issues, including ischemic colitis. Techniques such as mindfulness, yoga, and regular exercise can help manage stress effectively.
- Stay Hydrated: Adequate hydration is essential for maintaining the health of the digestive system and ensuring proper blood flow.
Role of Diet and Exercise
- Balanced Diet: Incorporating a diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain a healthy weight and reduce inflammation, which is crucial for preventing ischemic colitis.
- Limit Inflammatory Foods: Reducing the intake of foods that cause inflammation, such as red meats, processed foods, and high-fat dairy products, can decrease the risk of developing ischemic conditions.
- Regular Physical Activity: Engaging in regular exercise such as walking, swimming, or cycling for at least 150 minutes per week improves cardiovascular health and blood circulation, which is vital in preventing ischemic colitis.
Regular Medical Assessments
- Routine Check-Ups: Regular check-ups help in the early detection of risk factors related to ischemic colitis. At-risk individuals should have frequent vascular health assessments.
- Monitor Blood Pressure and Cholesterol Levels: High blood pressure and cholesterol can impair blood flow, increasing the risk of ischemic colitis. Monitoring these levels and keeping them within a healthy range is crucial.
- Personalized Risk Assessment: For individuals with a history of circulatory problems or ischemic conditions, personalized assessments tailored to their specific health needs are essential for effective prevention.
By integrating these preventive strategies into daily life, individuals can significantly reduce their risk of developing ischemic colitis.
FAQs about Ischemic Colitis Symptoms
What is ischemic colitis?
Ischemic colitis occurs when blood flow to part of the large intestine (colon) is reduced, typically due to narrowed or blocked blood vessels. This reduction in blood flow can cause pain and damage the colon’s tissues.
What are the common symptoms of ischemic colitis?
The most common symptoms of ischemic colitis include abdominal pain or cramping, a feeling of urgency to defecate, bloody diarrhea, and nausea. The pain is usually on the left side of the abdomen.
How quickly do symptoms of ischemic colitis appear?
Symptoms of ischemic colitis can develop suddenly or gradually. In acute cases, symptoms appear quickly and are often severe. In chronic cases, symptoms may be milder and develop over time.
Can ischemic colitis symptoms be mistaken for other conditions?
Yes, the symptoms of ischemic colitis can be similar to other gastrointestinal conditions like inflammatory bowel disease, diverticulitis, and gastrointestinal infections. It’s essential to consult a healthcare provider for an accurate diagnosis.
When should someone seek medical attention for ischemic colitis?
Immediate medical attention should be sought if you experience severe abdominal pain, bloody stools, or symptoms of dehydration such as dizziness and reduced urine output. These could be signs of a more serious condition or complications.
How is ischemic colitis diagnosed?
Ischemic colitis is typically diagnosed through a combination of medical history, physical examination, and diagnostic tests which may include blood tests, imaging tests like a CT scan, and a colonoscopy to examine the inner walls of the colon.
Are there any risk factors that increase the likelihood of developing ischemic colitis?
Risk factors for ischemic colitis include age (common in people over 60), a history of heart disease, diabetes, high cholesterol, and smoking. Certain medications that constrict blood vessels can also increase risk.
Conclusion
Understanding the early symptoms of ischemic colitis is crucial for prompt and effective treatment. Recognizing signs such as abdominal pain, blood in the stool, and urgent bowel movements can significantly mitigate the risks associated with this condition.
We strongly encourage individuals who are at risk, including older adults and those with underlying health issues like heart disease or diabetes, to consult with healthcare professionals regularly.
Early intervention can lead to better outcomes and prevent serious complications. Stay informed and proactive about your health to ensure long-term well-being.
References
For a deeper understanding of the symptoms and management of ischemic colitis, we recommend consulting the following reputable sources. These links provide additional information and validation of the details shared in our discussion on ischemic colitis symptoms:
- Mayo Clinic: Explore comprehensive details about the symptoms, causes, and treatment options for ischemic colitis. This trusted medical resource offers insights from healthcare professionals and up-to-date research findings. Read more about ischemic colitis on Mayo Clinic.
- MedlinePlus: A service of the U.S. National Library of Medicine, this site provides valuable health information that helps in understanding the risk factors and diagnostic approaches for ischemic colitis. Visit MedlinePlus for more information.
- WebMD: This resource gives a detailed overview of ischemic colitis, including symptoms, necessary lifestyle changes, and potential complications. It’s an excellent source for patient-friendly information and advice. Learn more at WebMD.
- Cleveland Clinic: Known for its patient-centered approach, Cleveland Clinic offers insights into the prevention and management of ischemic colitis. Their resource is beneficial for understanding long-term management strategies. Check out the Cleveland Clinic’s resource.
- Healthline: With easy-to-understand articles, Healthline breaks down the symptoms and treatments for ischemic colitis. They provide practical health advice and tips for managing the condition. Explore Healthline’s coverage on ischemic colitis.
These resources will provide you with a solid foundation for understanding ischemic colitis better and equip you with the knowledge to discuss symptoms and treatment options with healthcare providers.