Ischemic Colitis Treatment: Ischemic colitis, a medical condition characterized by reduced blood flow to the colon, can lead to various gastrointestinal symptoms ranging from mild discomfort to severe, life-threatening complications.
However, understanding the diagnostic methods and treatment options is essential for effective management and recovery.
Understanding Ischemic Colitis
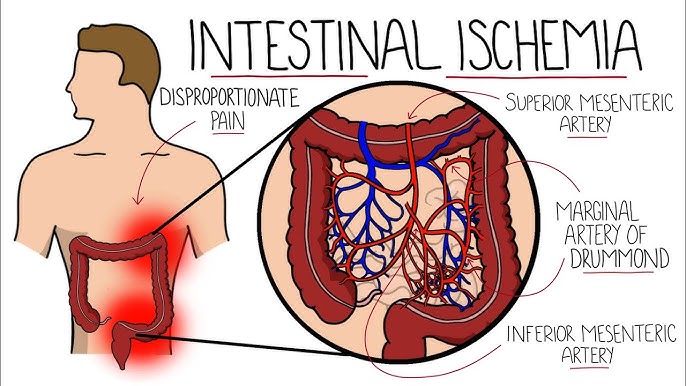
Ischemic colitis occurs when blood flow to part of the large intestine (colon) is reduced, usually due to narrowed or blocked blood vessels (arteries). The diminished blood flow provides insufficient oxygen for the cells in the digestive system. This condition can cause pain and can damage the colon. Understanding the causes and risk factors, along with awareness of its prevalence and demographics, can help individuals identify and manage this condition effectively.
Causes and Risk Factors
Ischemic colitis can stem from various situations that affect blood flow to the colon. Here are the primary causes and risk factors:
- Atherosclerosis: This is the most common cause, where plaque builds up and narrows the blood vessels leading to the intestines.
- Heart Conditions: Conditions like heart failure and arrhythmias, which reduce the heart’s ability to pump blood effectively, can lead to reduced blood flow to the colon.
- Low Blood Pressure: Severe drops in blood pressure, which can occur during surgery, from blood loss, or in other shock states, may decrease blood flow to the colon.
- Medications: Certain medications can constrict blood vessels or increase the risk of blood clotting, such as some types of diuretics, hormone medications, and nonsteroidal anti-inflammatory drugs (NSAIDs).
- Blood Clots: Blood clots in the arteries leading to the colon can block blood flow.
- Physical Strain: Heavy exertion or even activities like long-distance running can divert blood flow away from the colon to the muscles being used.
Risk factors include aging (being over the age of 60), chronic heart disease, diabetes, high cholesterol, and smoking, which all contribute to the likelihood of developing ischemic colitis.
Statistics on Prevalence and Demographics Affected
Ischemic colitis is more common in older adults, typically affecting people over 60 years old. However, younger adults may also be at risk under certain conditions, such as extreme physical exertion or dehydration.
- Gender: It slightly more frequently affects women than men.
- Incidence Rates: Approximately 16 to 22 cases of ischemic colitis occur per 100,000 person-years.
- Hospitalization: It accounts for about 1 in 2,000 hospital admissions annually.
- Outcomes: The majority of cases are mild and can be treated effectively; however, severe cases may require surgery and can lead to complications if not addressed promptly.
However, understanding these factors helps individuals and healthcare providers recognize symptoms early and seek appropriate treatment to prevent complications.
Signs and Symptoms of Ischemic Colitis
Here’s a detailed look at the common symptoms and how they differ from other gastrointestinal issues, along with guidelines on when to seek medical advice.
Common Symptoms of Ischemic Colitis
- Abdominal Pain: Often sudden and crampy, typically on the left side of the abdomen.
- Bloody Stools: Passage of bright red or maroon blood in the stool.
- Urgent Need to Defecate: A sudden and intense need to have a bowel movement.
- Diarrhea: Frequent, loose, or watery stools.
- Abdominal Tenderness: Pain when the abdomen is touched.
- Nausea and Vomiting: Feeling sick and sometimes vomiting.
- Fever: A mild to moderate increase in body temperature.
Differentiating Symptoms from Other Gastrointestinal Issues
Ischemic colitis symptoms can overlap with other gastrointestinal conditions, making diagnosis challenging. Here’s how to distinguish it:
- Irritable Bowel Syndrome (IBS): IBS also causes abdominal pain and changes in bowel habits but rarely involves bloody stools or fever.
- Ulcerative Colitis and Crohn’s Disease: These inflammatory bowel diseases often present with chronic symptoms and may include weight loss and severe fatigue, unlike the more sudden onset of ischemic colitis.
- Gastroenteritis: Typically caused by infections, it involves vomiting and diarrhea but usually does not cause bloody stools or the severe abdominal pain seen in ischemic colitis.
When to Seek Medical Advice
Immediate medical attention is necessary if you experience:
- Severe abdominal pain
- Bloody stools
- A sudden and intense need to defecate
- High fever
- Persistent nausea and vomiting
Early intervention can prevent complications and improve outcomes. If you suspect ischemic colitis, do not delay in contacting a healthcare professional.
Diagnosis of Ischemic Colitis
Accurate diagnosis is essential for effective treatment and management. Below is a comprehensive overview of the diagnostic procedures, challenges, and the importance of differential diagnosis in ischemic colitis.
List of Diagnostic Procedures
1. Medical History and Physical Examination: Initial assessment involves detailed patient history and physical examination to identify risk factors and symptoms such as abdominal pain, blood in stool, and changes in bowel habits.
2. Laboratory Tests: Blood tests to check for markers of inflammation, infection, and anemia. Common tests include complete blood count (CBC), C-reactive protein (CRP), and lactate levels.
3. Imaging Studies:
- CT Scan: The most commonly used imaging modality to visualize the colon and identify signs of ischemia, such as thickening of the bowel wall.
- MRI: Provides detailed images and can be useful in certain cases where CT scan results are inconclusive.
- Doppler Ultrasound: Assesses blood flow in the mesenteric arteries and can help identify vascular insufficiency.
4. Colonoscopy: Direct visualization of the colon allows for assessment of the mucosa and identification of ischemic changes, such as pale or bluish discoloration and ulcerations. Biopsies can be taken for histopathological examination.
5. Angiography: Used in some cases to directly visualize blood vessels and identify any blockages or narrowing that could be causing reduced blood flow to the colon.
Challenges in Diagnosing Ischemic Colitis
Diagnosing ischemic colitis can be challenging due to several factors:
- Non-Specific Symptoms: Symptoms of ischemic colitis often overlap with other gastrointestinal conditions such as inflammatory bowel disease (IBD), infections, and irritable bowel syndrome (IBS), making it difficult to distinguish between them based on symptoms alone.
- Variable Presentation: The severity and presentation of ischemic colitis can vary widely among patients, ranging from mild, self-limiting cases to severe, life-threatening conditions.
- Timing of Diagnosis: Early symptoms can be subtle, and delays in seeking medical attention can lead to advanced disease, complicating diagnosis and treatment.
Importance of Differential Diagnosis
Differential diagnosis is crucial in the evaluation of ischemic colitis to ensure accurate identification and appropriate management of the condition. Misdiagnosis can lead to inappropriate treatment and potentially serious complications. By considering and ruling out other potential causes of the patient’s symptoms, healthcare providers can:
- Avoid Mismanagement: Ensure that the patient receives the correct treatment and avoids unnecessary interventions that may worsen their condition.
- Tailor Treatment Plans: Develop targeted treatment strategies that address the specific underlying cause of the patient’s symptoms, improving outcomes and reducing complications.
- Improve Prognosis: Early and accurate diagnosis can significantly improve the patient’s prognosis, reducing the risk of severe complications and improving overall quality of life.
However, the diagnosis of ischemic colitis requires a combination of thorough clinical evaluation, appropriate diagnostic procedures, and careful consideration of differential diagnoses.
Treatment Options for Ischemic Colitis
Effective management of this condition is crucial to prevent complications and ensure recovery. Here are the primary approaches to treating ischemic colitis:
Medical Treatments
- Medications: Doctors may prescribe antibiotics to prevent infection, pain relievers to manage discomfort, and anti-inflammatory drugs to reduce inflammation in the colon.
- Intravenous (IV) Fluids: To prevent dehydration and provide essential nutrients, IV fluids are often administered, especially if the patient is unable to eat or drink.
- Blood Thinners: In cases where blood clots are a contributing factor, blood thinners may be prescribed to improve blood flow.
Surgical Treatments
- Bowel Resection: In severe cases where a part of the colon is damaged, surgery may be required to remove the affected section.
- Stent Placement: For patients with narrowed blood vessels, stents can be placed to keep the vessels open and improve blood flow.
Lifestyle and Dietary Adjustments
Adopting healthy lifestyle habits and making dietary changes can significantly improve the management and recovery of ischemic colitis. Here are some key adjustments:
- Hydration: Drinking plenty of water helps maintain adequate blood flow and prevents dehydration, which can worsen symptoms.
- Balanced Diet: Eating a diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and improve digestion.
- Low-Fiber Diet: During flare-ups, a low-fiber diet can reduce bowel irritation and promote healing. Gradually reintroduce fiber as symptoms improve.
- Avoiding Alcohol and Caffeine: These substances can irritate the digestive system and should be limited or avoided.
- Regular Exercise: Engaging in regular physical activity can improve circulation and overall digestive health.
- Smoking Cessation: Smoking can exacerbate ischemic colitis and impede healing, so quitting is strongly advised.
Implementing these treatment options and lifestyle adjustments can help manage ischemic colitis effectively, reduce symptoms, and prevent complications. Always consult with a healthcare professional to tailor a treatment plan that meets individual needs.
Recovery and Management of Ischemic Colitis
Recovery from ischemic colitis typically varies based on the severity of the condition and the patient’s overall health. Most patients start to feel better within a few days to a week after initial treatment. Full recovery can take several weeks, with severe cases potentially requiring months. Hospitalization may be necessary for those with severe symptoms or complications.
Monitoring and Long-term Management Strategies
- Regular Medical Check-ups: Frequent visits to your healthcare provider are crucial to monitor progress and detect any potential complications early.
- Imaging and Endoscopy: Periodic imaging studies and colonoscopy may be recommended to assess the healing process and ensure no underlying issues persist.
- Medication Adherence: Strict adherence to prescribed medications, such as antibiotics or anti-inflammatory drugs, is essential to prevent recurrence.
- Managing Comorbid Conditions: Effective management of conditions like hypertension, diabetes, and heart disease is vital to reduce the risk of further ischemic episodes.
Role of Diet and Lifestyle in Recovery
- Balanced Diet: Consuming a well-balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports overall digestive health and recovery.
- Hydration: Staying well-hydrated helps maintain optimal blood flow and prevents constipation, which can exacerbate symptoms.
- Avoiding Triggers: Identifying and avoiding foods or beverages that trigger symptoms can prevent flare-ups.
- Regular Exercise: Engaging in moderate physical activity promotes good circulation and overall health, aiding in recovery.
- Stress Management: Techniques such as yoga, meditation, or counseling can help manage stress, which may otherwise impact recovery negatively.
Importance of Follow-up Visits
Follow-up visits are critical to ensure the successful management of ischemic colitis. During these visits, healthcare providers can:
- Assess Healing Progress: Check for signs of improvement or complications.
- Adjust Treatment Plans: Modify medications or dietary recommendations based on the patient’s current condition.
- Early Detection of Recurrence: Identify any signs of recurrence early and take necessary preventive measures.
- Provide Ongoing Support: Offer guidance on lifestyle changes and answer any questions or concerns about the recovery process.
By adhering to a comprehensive management plan that includes medical, dietary, and lifestyle strategies, patients can achieve a successful recovery from ischemic colitis and maintain long-term health.
Prevention of Ischemic Colitis
Fortunately, there are several preventative measures and lifestyle changes that can significantly reduce the risk of developing this condition.
Preventative Measures and Lifestyle Changes
- Maintain a Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can improve overall vascular health and reduce the risk of ischemic colitis. Avoid high-fat and high-cholesterol foods, which can contribute to arterial blockage.
- Stay Hydrated: Adequate fluid intake is essential for maintaining blood flow and preventing dehydration, which can exacerbate ischemic conditions.
- Exercise Regularly: Regular physical activity improves cardiovascular health and enhances blood circulation. Aim for at least 30 minutes of moderate exercise most days of the week.
- Avoid Smoking: Smoking damages blood vessels and reduces blood flow. Quitting smoking is one of the most effective ways to prevent vascular diseases, including ischemic colitis.
- Limit Alcohol Intake: Excessive alcohol consumption can lead to dehydration and negatively affect cardiovascular health. Drink alcohol in moderation, if at all.
- Manage Stress: Chronic stress can negatively impact cardiovascular health. Engage in stress-reducing activities such as yoga, meditation, and deep-breathing exercises.
Risk Factor Management
- Cardiovascular Health: Regular check-ups with your healthcare provider are essential for monitoring and managing blood pressure, cholesterol levels, and other cardiovascular risk factors. Medications may be prescribed to control these conditions.
- Diabetes Control: Proper management of diabetes is crucial. This includes maintaining blood sugar levels within the target range, adhering to prescribed medications, and following a diabetes-friendly diet.
- Weight Management: Maintaining a healthy weight reduces the strain on your heart and blood vessels. A balanced diet combined with regular exercise can help achieve and maintain a healthy weight.
- Monitor Medication Use: Certain medications, such as NSAIDs and hormone replacement therapies, can increase the risk of ischemic colitis. Consult with your doctor to understand the risks and explore alternative treatments if necessary.
- Regular Screenings: Regular medical screenings and tests can help detect early signs of vascular problems. Early detection and intervention can prevent the progression to ischemic colitis.
By incorporating these preventative measures and managing risk factors, individuals can significantly reduce their chances of developing ischemic colitis. Maintaining a healthy lifestyle and working closely with healthcare providers are key steps in prevention.
FAQs about Ischemic Colitis Treatment
What is ischemic colitis?
Ischemic colitis occurs when blood flow to the colon is reduced, causing inflammation and injury. It can lead to abdominal pain, cramping, and bloody stools.
What are the symptoms of ischemic colitis?
Common symptoms include sudden abdominal pain, an urgent need to have a bowel movement, blood in the stool, and diarrhea. In severe cases, fever and low blood pressure may occur.
How is ischemic colitis diagnosed?
Diagnosis typically involves a combination of medical history review, physical examination, blood tests, and imaging studies like a CT scan or colonoscopy to assess the extent of colon damage.
What treatments are available for ischemic colitis?
Treatment depends on the severity. Mild cases may resolve with supportive care, including rest, hydration, and a temporary liquid diet. Severe cases might require antibiotics, intravenous fluids, or surgery to remove damaged tissue.
Can lifestyle changes help manage ischemic colitis?
Yes, maintaining a healthy diet, staying hydrated, avoiding smoking, and managing underlying health conditions like high blood pressure and cholesterol can help reduce the risk of ischemic colitis.
Is ischemic colitis a chronic condition?
Ischemic colitis is usually not chronic. Most people recover completely with appropriate treatment, although some may experience recurrent episodes, particularly if underlying risk factors are not addressed.
When should I see a doctor?
Seek medical attention if you experience severe abdominal pain, bloody stools, persistent diarrhea, or any symptoms of ischemic colitis. Early diagnosis and treatment are crucial for a good outcome.
Conclusion
Recognizing and treating ischemic colitis promptly is crucial for maintaining good health. This condition can lead to severe complications if not addressed early.
By understanding the symptoms and seeking immediate medical attention, patients can prevent further damage and promote recovery.
It is essential to adhere to professional medical advice and follow prescribed treatments diligently. Regular check-ups and a healthy lifestyle can also contribute to preventing future episodes.
Always prioritize your health by consulting healthcare professionals when symptoms arise and following their guidance for effective management and recovery.
References
For further reading and to validate the information provided in this guide on ischemic colitis treatment, consider exploring these reputable sources:
- Mayo Clinic – Detailed overview of ischemic colitis symptoms, causes, and treatment options. Read more
- WebMD – Comprehensive guide on ischemic colitis, including diagnosis and management. Read more
- Johns Hopkins Medicine – Insights into the latest research and treatment advancements for ischemic colitis. Read more
- Cleveland Clinic – Information on the symptoms, diagnosis, and treatment of ischemic colitis. Read more
These sources offer extensive information and are trusted in the medical community for their accuracy and reliability.