Intussusception Symptoms: Intussusception is a serious medical condition where a part of the intestine folds into the section next to it, much like the pieces of a telescope sliding together.
This often results in a blockage in the bowel, cutting off the blood supply to the affected parts of the intestine.
It is a medical emergency that requires prompt diagnosis and treatment.
Understanding Intussusception
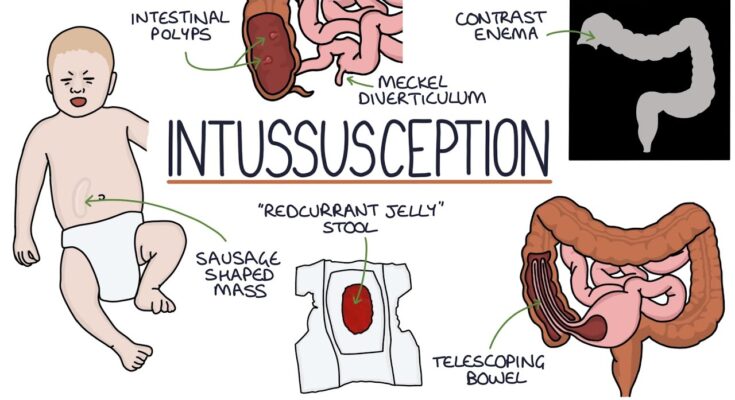
Intussusception is a serious condition where part of the intestine slides into an adjacent part of the intestine, much like the pieces of a telescope. This “telescoping” effect can lead to blockages, which disrupt the flow of food and can cut off the blood supply to the affected part of the intestine. Understanding the prevalence of intussusception in different age groups and the anatomy affected can help in recognizing the urgency of medical intervention.
How Common is Intussusception in Children and Adults?
Intussusception is primarily a pediatric condition. It is most common in young children and infants, particularly those between the ages of six months and three years. In this age group, it is one of the most frequent causes of bowel obstruction and typically requires urgent medical attention. The incidence in infants and young children is approximately 1 to 4 cases per 2,000 children, making it a relatively common emergency in pediatric medicine.
In contrast, intussusception in adults is rare and accounts for only about 5% of all cases. In adults, it is often linked to an underlying medical condition or a structural problem within the intestine, such as a polyp or tumor, which can act as a lead point for the telescoping.
The Anatomy Affected by Intussusception
Intussusception can occur in various parts of the intestine but most commonly affects the junction where the small intestine meets the large intestine, known as the ileocecal junction. Here’s a breakdown of the key anatomical areas involved:
- Ileum: The lower end of the small intestine that is most often involved in telescoping into the colon.
- Cecum: A pouch at the beginning of the large intestine that can be pulled into the ascending colon.
- Colon: The large intestine, which may also be part of the intussusception, especially in adult cases.
However, due to the nature of the condition and the potential for significant complications such as bowel necrosis, timely diagnosis and treatment are crucial.
Symptoms of Intussusception
Recognizing the symptoms early can lead to timely medical intervention and a better prognosis. Here’s what you need to know about the signs of intussusception across different age groups and when to seek medical help.
Early Signs of Intussusception
The early symptoms of intussusception can be subtle and sometimes difficult to distinguish from other common childhood illnesses. However, some key signs to watch for include:
- Sudden abdominal pain: Infants may cry loudly and suddenly, pulling their legs up toward their abdomen in response to waves of pain.
- Bowel habits: Changes such as passing a stool that looks like red currant jelly, which contains blood and mucus, is a classic symptom.
- Vomiting: This can range from mild to severe and may include bile.
- Lethargy: The child may seem unusually tired or weak.
How Symptoms Vary Between Infants, Children, and Adults
Infants:
- Intermittent crying that comes in intense waves
- Drawing knees to chest during episodes of pain
- A palpable mass in the abdomen (in some cases)
- Episodes of lethargy between cries
Children:
- Persistent abdominal pain
- Swelling of the abdomen
- Dehydration symptoms, such as dry mouth and decreased urination
- Fever and a general sense of being unwell
Adults:
- Although less common, adults can also suffer from intussusception. Symptoms in adults often include:
- Acute abdominal pain and bloating
- Vomiting
- Constipation or feeling unable to pass a bowel movement
- Noticeable abdominal swelling
When to Seek Medical Attention
Intussusception is a medical emergency. If you notice any of the symptoms mentioned above, it’s crucial to seek medical attention immediately. This is particularly urgent if the person exhibits:
- Severe abdominal pain
- Blood in the stool (which may appear as red jelly-like substance)
- High fever
- Signs of shock, such as pale skin, cold hands and feet, and rapid breathing
However, medical care typically involves imaging tests to confirm the diagnosis and a procedure to correct the intussusception, which may include an enema or surgery depending on the severity and response to initial treatment measures.
Causes of Intussusception
Understanding the causes and risk factors of intussusception is essential for early diagnosis and prevention. Here, we explore the primary and secondary causes of this condition, along with the associated risk factors and preventive measures.
Primary Causes of Intussusception
The primary causes of intussusception often relate directly to the inherent conditions within the bowel itself, including:
- Idiopathic Factors: In many cases, particularly in infants and young children, the exact cause of intussusception is not known. This idiopathic nature accounts for the majority of occurrences in children.
- Anatomical Variations: Certain anatomical differences, such as Meckel’s diverticulum or congenital bowel length discrepancies, can predispose individuals to intussusception.
- Motility Disorders: Disorders that affect the normal motility of the gastrointestinal tract can lead to abnormal movements, potentially causing one part of the intestine to slip into another.
Secondary Causes of Intussusception
Secondary causes are generally associated with underlying conditions that may trigger intussusception, including:
- Infections: Viral or bacterial infections that lead to inflammation and swelling of the intestinal walls can precipitate intussusception.
- Tumors: Both benign and malignant tumors can act as a lead point for intussusception. These may include polyps, lymphomas, or other neoplasms within the intestine.
- Surgical Scars: Post-surgical scar tissue can create a focal point around which intussusception can occur.
Risk Factors and Preventive Measures
While intussusception can occur without clear predisposing factors, several risk factors increase the likelihood of this condition:
- Age: The most common age group affected is infants and young children, especially those between six months and three years old.
- Previous Intussusception: Individuals who have experienced intussusception previously are at a higher risk of recurrence.
- Certain Medical Conditions: Conditions such as cystic fibrosis or celiac disease that affect the structure or function of the intestines may increase the risk.
Preventive Measures:
While preventing intussusception entirely may not always be possible, especially in idiopathic cases, awareness and early recognition of symptoms are crucial. Parents and caregivers should seek prompt medical attention if they notice signs such as sudden abdominal pain, vomiting, bloody stools, or a palpable mass in the abdomen of a child. In cases where specific risk factors are identified, regular medical check-ups and appropriate management of underlying conditions can help reduce the likelihood of intussusception.
By understanding the causes and risk factors associated with intussusception, individuals can better seek timely medical intervention, potentially mitigating the severity of the condition.
Diagnosis of Intussusception
Diagnosing intussusception involves a combination of medical history evaluation, physical examinations, and imaging tests. Early detection is crucial to manage this condition effectively and to prevent serious complications.
Medical History and Physical Examination
The first step in diagnosing intussusception is collecting a thorough medical history and conducting a physical examination. Healthcare providers will ask about symptoms such as abdominal pain, vomiting, bloody stools, and episodes of crying or distress in children. During the physical examination, doctors will look for signs of abdominal swelling or a palpable mass, which may indicate the presence of intussusception.
Imaging and Tests Used to Diagnose Intussusception
Advanced imaging techniques play a vital role in confirming the diagnosis of intussusception. These tests help visualize the intestines and determine the location and severity of the telescoping bowel.
Ultrasound: The First-line Imaging Technique
Ultrasound is the preferred first-line imaging method for suspected intussusception. It is a safe, non-invasive, and effective tool that provides real-time images of the intestines. Ultrasound can help identify the characteristic “target” or “doughnut” sign, indicative of intussusception. This method is particularly valuable as it avoids radiation exposure, making it ideal for children.
Additional Diagnostic Tools (X-ray, CT Scan, etc.)
While ultrasound is highly effective, additional diagnostic tools may be used if the ultrasound results are inconclusive or if complications are suspected:
- X-rays: These can be helpful in identifying signs of intestinal obstruction or perforation. An X-ray may show a pattern of air distribution that suggests intussusception or other complications like trapped gas.
- CT Scans: In adults or when other imaging modalities are inconclusive, a computed tomography (CT) scan can provide detailed images of the abdominal organs. CT scans are particularly useful in identifying the presence of intussusception in older patients, where the condition might be caused by a tumor.
- Air or Barium Enema: This is both a diagnostic and therapeutic procedure. It involves inserting air or barium into the colon via the rectum to help push the telescoped part of the bowel back into place. This procedure can also provide excellent diagnostic images and is sometimes successful in treating the condition.
By combining these diagnostic methods, healthcare providers can accurately diagnose intussusception, allowing for timely and appropriate treatment interventions.
Treatment Options for Intussusception
Effective treatment is crucial to prevent complications such as tissue death and perforation of the intestine. Here, we explore the various treatment options for intussusception, including non-surgical management, surgical interventions, and post-treatment care and monitoring.
Non-Surgical Management
- Air or Barium Enema: The first line of treatment for intussusception, particularly in children, is a therapeutic enema. This can be either an air or a barium enema, which is not only diagnostic but also therapeutic. The pressure from the enema may help to unfold the intestine and resolve the intussusception without the need for surgery. This procedure has a high success rate and is often attempted under fluoroscopic guidance by a radiologist.
- IV Fluids and Electrolytes: Patients with intussusception often need supportive care, which includes hydration and electrolyte management. Intravenous (IV) fluids are administered to maintain hydration and correct electrolyte imbalances.
- Observation and Monitoring: Close monitoring is crucial after a non-surgical attempt to treat intussusception. This includes regular abdominal examinations and possibly further imaging studies to ensure that the intussusception has been successfully reduced.
Surgical Interventions
- Manual Reduction: If non-surgical methods fail, surgical intervention may be required. During surgery, the surgeon manually reduces the intussusception, which involves gently squeezing the telescoped section of the intestine back into its proper position.
- Resection of Non-Viable Intestine: In cases where the intestine has become necrotic (tissue death due to lack of blood supply), the affected segment may need to be removed. This procedure is called resection.
- Laparoscopy: For less severe cases or when the exact condition of the intestine is unclear, a laparoscopic approach may be used. This minimally invasive surgery involves making small incisions and using a camera to guide the procedure, allowing for quicker recovery times and less post-operative pain.
Post-Treatment Care and Monitoring
- Follow-Up Imaging: After treatment, whether non-surgical or surgical, follow-up imaging studies are often necessary to confirm that the intussusception has not recurred and that the intestines are functioning properly.
- Diet and Activity Recommendations: Post-treatment guidelines typically include dietary modifications to ease the digestive process. Gradual reintroduction of normal diet and careful monitoring of bowel movements are important.
- Regular Medical Check-Ups: Regular check-ups are vital to monitor the overall health of the patient and to promptly address any complications or signs of recurrence.
By understanding these treatment options and the importance of comprehensive post-treatment care, patients and caregivers can be better prepared to manage intussusception effectively. Prompt medical attention and following the doctor’s recommendations are key to a successful recovery.
FAQs about Intussusception Symptoms
What is intussusception?
Intussusception is a serious condition where part of the intestine slides into an adjacent part of the intestine. This “telescoping” effect can block food or fluid from passing through and disrupt blood flow to the affected part of the intestine.
What are the common symptoms of intussusception?
The most common symptoms of intussusception include severe abdominal pain that comes in waves, vomiting, bloody stools that may resemble red currant jelly, and a swollen abdomen. Infants may also cry and draw their knees to their chest as a reaction to the pain.
At what age is intussusception most likely to occur?
Intussusception is most commonly seen in children between six months and three years of age, but it can occasionally occur in older children and adults.
How quickly do symptoms of intussusception develop?
Symptoms of intussusception can develop rapidly, often within hours. The onset is usually sudden, and the symptoms can be intense and frightening.
Is intussusception a medical emergency?
Yes, intussusception is a medical emergency. If you suspect someone has intussusception, it’s crucial to seek immediate medical attention. Delaying treatment can lead to serious complications, including infection, perforation of the intestine, and potentially life-threatening shock.
Can intussusception resolve on its own?
In very rare cases, intussusception may resolve itself. However, medical evaluation and treatment are necessary because it is difficult to confirm resolution without a medical assessment, and the risks of complications are high.
What should I do if I suspect intussusception?
If you suspect intussusception, especially in a child, it is essential to go to the nearest emergency department immediately. Quick action can lead to a better outcome and prevent serious health complications.
Conclusion
In conclusion, recognizing the symptoms and understanding the causes of intussusception is crucial for timely and effective treatment. Common symptoms include abdominal pain, vomiting, and the presence of blood in the stool, which should prompt immediate medical evaluation. Understanding that intussusception can arise from various conditions helps in identifying potential risks and underlying health issues.
We strongly encourage anyone observing these symptoms, particularly in infants and young children, to seek prompt medical care. Early intervention is key to preventing complications and ensuring a smooth recovery.
The prognosis for intussusception is generally favorable with timely treatment. Most patients recover fully after the necessary medical procedures, such as air or liquid enema, which are successful in most cases. Surgery may be required if these treatments are not effective, but it too typically results in a complete recovery.
By staying informed and vigilant, you can help ensure a swift response to the signs of intussusception, leading to a positive outcome and quick recovery.
References
For those seeking more information on intussusception symptoms and the validation of the data presented, the following reputable sources are recommended. These references have been carefully selected to provide a deeper understanding and further reading opportunities.
- Mayo Clinic – Explore detailed explanations of intussusception symptoms, causes, and treatments on the Mayo Clinic’s official website. Access their comprehensive resource here.
- WebMD – WebMD offers an in-depth look at intussusception, including symptoms and emergency treatment procedures. Learn more by visiting their page on intussusception here.
- MedlinePlus – A service of the U.S. National Library of Medicine, MedlinePlus provides a user-friendly article covering all you need to know about intussusception. Check out their article here.
- Healthline – Healthline’s guide to intussusception includes symptoms, risk factors, and diagnosis. This resource can be found here.
- PubMed – For academic research articles and clinical studies related to intussusception, PubMed is a reliable source. You can search for peer-reviewed articles here.
These sources are invaluable for patients, caregivers, and medical professionals interested in the specifics of intussusception symptoms and related healthcare information.