Intussusception Treatment: Intussusception is a serious and relatively rare medical condition where part of the intestine folds into an adjacent segment of the intestinal tract.
This potentially life-threatening situation causes a blockage in the bowel, leading to severe complications if not promptly diagnosed and treated.
Understanding the diagnosis and treatment options for intussusception is critical for ensuring patient safety and health outcomes.
Understanding Intussusception
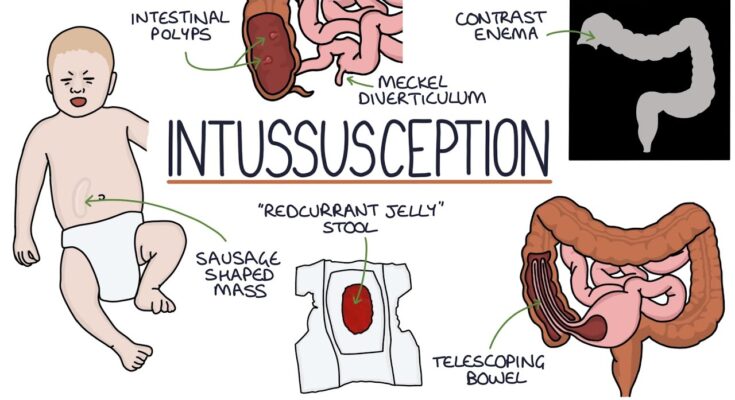
Intussusception is a serious medical condition in which a part of the intestine folds into an adjacent section. This “telescoping” effect can lead to blockages, disrupting the flow of food and potentially cutting off the blood supply. Recognizing the common causes and risk factors, as well as understanding the demographics most affected by intussusception, can enhance awareness and prompt timely medical intervention.
Common Causes and Risk Factors
- Viral Infections: Certain viruses can lead to lymphoid hyperplasia (swelling of lymphoid tissue) in the intestines, which may trigger intussusception.
- Structural Abnormalities: Conditions like Meckel’s diverticulum or polyps can predispose individuals to intussusception.
- Surgical Procedures: Previous abdominal surgery may increase the risk of developing intussusception due to the formation of adhesions.
- Hereditary Factors: In some cases, a genetic predisposition may be involved, although this is less common.
- Age: Infants and young children are particularly susceptible, especially those between 6 months and 2 years old.
Statistics on Incidence and Demographics Most Affected
- Age Group: The majority of intussusception cases occur in children, particularly infants and toddlers. Over 80% of cases are seen in children under the age of 3 years.
- Gender: Boys are slightly more likely than girls to develop intussusception, with a ratio of approximately 3:2.
- Geographical Variations: While intussusception can occur worldwide, the incidence rates can vary based on geographic location and the prevalence of certain viral infections.
- Seasonal Trends: Some regions report seasonal peaks in intussusception cases, which often correlate with the prevalence of viral gastroenteritis.
However, understanding the causes, risk factors, and demographics affected by intussusception helps in recognizing symptoms early, which is crucial for prompt and effective treatment.
Symptoms of Intussusception
Recognizing the symptoms early can be crucial for timely treatment. Here, we explore the early and progressive symptoms of intussusception and how these symptoms can vary among different age groups such as infants, children, and adults.
Early Symptoms of Intussusception
The initial signs of intussusception are often subtle and can be easily overlooked. Here are the common early symptoms:
- Abdominal Pain: Sudden, severe, and intermittent pain is typical. Infants may cry and draw their knees to their chest during episodes of pain.
- Bloating: The abdomen may appear swollen or distended.
- Vomiting: Early vomiting may occur, which is not necessarily bile-stained at this stage.
- Lethargy: There might be a noticeable decrease in energy and activity levels.
Progressive Symptoms of Intussusception
As the condition progresses, the symptoms become more severe and distinct:
- Bloody Stool: Often described as “currant jelly” stool due to its red and jelly-like appearance. This is a result of mucous and blood.
- Increased Vomiting: Vomiting becomes more frequent and may include bile.
- Worsening Abdominal Pain: The pain becomes more constant and severe.
- Signs of Shock: Pale skin, cold hands and feet, and a rapid but weak pulse may develop as the condition worsens.
Symptoms by Age Group
The manifestation of intussusception symptoms can vary significantly by age, which is crucial for accurate diagnosis:
- Infants: The most common signs in infants include intermittent severe abdominal pain, vomiting, and the presence of bloody stools. Infants are less likely to verbalize their discomfort and may instead be inconsolably crying and appear excessively sleepy.
- Children: Older children might be able to communicate their symptoms more clearly. They may complain of abdominal pain, which can be localized to specific areas depending on the section of the bowel affected. They also experience vomiting, lethargy, and possibly bloody stools.
- Adults: While intussusception is rare in adults, the symptoms can include more specific signs like targeted abdominal pain, noticeable bloating, vomiting, and the possible presence of a palpable abdominal mass. Adults are more likely to experience subtle signs until the condition becomes severe.
If you or someone you know exhibits these symptoms, it is important to seek medical attention immediately.
Diagnosing Intussusception
Proper diagnosis is critical for effective treatment and recovery. Here’s how this condition is generally diagnosed, along with some challenges and considerations that may arise during the process.
Diagnostic Methods for Intussusception
- Ultrasound: This is the primary diagnostic tool for intussusception. It’s non-invasive and highly effective in identifying the presence of the “target sign” characteristic of this condition.
- X-ray: Abdominal x-rays can show signs of intestinal obstruction and are useful for ruling out other causes of abdominal pain.
- CT Scan: A computed tomography (CT) scan can provide detailed images and is useful if the diagnosis is uncertain or if complications are suspected.
- Air or Barium Enema: This is both a diagnostic and therapeutic tool. It can help confirm the presence of intussusception and in many cases, successfully reduce it.
- MRI: Although less commonly used, magnetic resonance imaging (MRI) can provide detailed images without radiation exposure, making it a safer option for repeated imaging.
The Role of Medical History and Physical Examination in Diagnosis
- Medical History: Gathering a detailed medical history helps identify previous episodes of intussusception or conditions that might increase the risk. It also helps differentiate intussusception from similar gastrointestinal disorders.
- Physical Examination: Physical signs such as abdominal swelling, palpable sausage-shaped mass in the abdomen, and signs of pain during palpation are key indicators. The examination might also reveal symptoms like lethargy or shock in severe cases.
Challenges and Considerations in Diagnosing Intussusception
- Age of Patient: Intussusception is most common in infants and young children, who may not be able to communicate their symptoms clearly.
- Symptom Overlap: The symptoms of intussusception, such as abdominal pain and vomiting, are common to many other disorders, which can lead to misdiagnosis.
- Timing: Rapid diagnosis is crucial as delayed treatment can lead to severe complications like bowel necrosis and perforation.
- Interpretation of Diagnostic Tests: Some diagnostic tests require expert interpretation; for instance, distinguishing intussusception from other causes of bowel obstruction on an x-ray or ultrasound can be challenging.
- Access to Imaging Technology: In some regions, immediate access to advanced imaging technology like CT scans or MRIs may be limited, delaying diagnosis and treatment.
However, effective diagnosis of intussusception involves a combination of advanced imaging techniques, careful medical history assessment, and thorough physical examination.
Treatment Options for Intussusception
Understanding the available treatments can help in managing the condition effectively. This guide details the non-surgical and surgical treatment options, as well as emerging therapies currently being explored in clinical trials.
Non-Surgical Treatments
Non-surgical treatments are typically the first line of intervention, especially in cases where the condition is diagnosed early and there are no signs of complications like perforation or infection. The following are the primary non-surgical treatment methods:
- Air or Barium Enema: This is both a diagnostic procedure and a treatment method. A mixture of air or barium is introduced into the colon using an enema. The pressure from this mixture can often cause the intestine to unfold back to its normal position. This procedure is usually performed under fluoroscopic guidance to monitor the progress.
- Intravenous (IV) Fluids: Patients with intussusception might be dehydrated; thus, IV fluids are administered to prevent dehydration and maintain adequate blood flow and electrolyte balance.
- Observation: In some instances, especially in mild cases, medical practitioners may recommend a period of close observation to see if the intussusception resolves on its own before proceeding with more invasive treatments.
Surgical Treatments
If non-surgical treatments fail or if the patient exhibits severe symptoms, surgical intervention may be necessary. Surgical treatments for intussusception include:
- Manual Reduction Surgery: This surgery involves the physical manipulation of the intestine to un-telescope it. This is often done via laparotomy (open surgery) or laparoscopy (minimally invasive).
- Resection: If a segment of the intestine is severely damaged, it may need to be removed. Resection is performed to excise the damaged part and reconnect the healthy sections.
- Laparoscopy: For less severe cases, or when the bowel does not appear severely damaged, a minimally invasive approach using laparoscopy may be employed. This method reduces recovery time and the risk of infection.
Emerging Therapies and Interventions in Clinical Trials
Research into new treatment options for intussusception is ongoing, with several innovative therapies being tested in clinical trials. These include:
- New Imaging Techniques: Advanced imaging techniques that offer clearer, more detailed views of the intestine, potentially improving the diagnosis and the effectiveness of non-surgical treatments.
- Biological Therapies: These involve the use of medications that can relax the intestinal muscles, potentially reducing the need for surgical intervention.
- Custom Stents: The development of specialized stents that can be inserted endoscopically to hold the intestine open and prevent re-telescoping.
However, these emerging therapies aim to increase the effectiveness of treatments, reduce the need for surgery, and improve recovery times. As these treatments are still under investigation, they are generally available only through clinical trials.
Complications of Intussusception
Intussusception is a serious condition where part of the intestine slides into an adjacent part, similar to the pieces of a telescope folding into each other. This can cause a blockage in the bowel, leading to several complications if not promptly treated. Understanding these potential risks is crucial for effective management and early intervention.
Possible Complications if Untreated or Delayed Treatment
- Bowel Obstruction: The most immediate and dangerous complication is bowel obstruction, where the intestine becomes completely blocked, preventing the passage of food and fluids.
- Perforation: Continued pressure from the trapped section of the intestine can lead to perforation, or a tear in the bowel wall. This can result in a severe infection or peritonitis, which is a life-threatening condition requiring immediate surgical intervention.
- Infection and Sepsis: If the intestine is perforated, bacteria from the bowel can enter the abdominal cavity, leading to infection and possibly progressing to sepsis, a widespread and potentially fatal response to infection.
- Ischemia and Necrosis: Intussusception can cut off the blood supply to parts of the intestines, leading to ischemia (lack of blood flow) and necrosis (tissue death), which can complicate surgical procedures and recovery.
- Dehydration and Shock: As the intestine becomes blocked, fluid and electrolyte balance can be disrupted, leading to severe dehydration. If untreated, this can escalate into shock, further endangering the patient’s life.
Long-term Outlook for Patients after Treatment
The long-term outlook for patients who receive timely treatment for intussusception is generally positive. Here are key points regarding the prognosis post-treatment:
- Successful Reduction: Many cases of intussusception can be resolved with a non-surgical procedure called an enema, which is successful in reducing the telescoped segment of the intestine in about 70-90% of cases in children.
- Surgical Outcomes: If an enema is not successful, surgery is required to correct the intussusception. Post-surgery, most patients recover without further issues, provided there are no complications like infection or necrosis.
- Recurrence: Approximately 5-10% of cases may recur, typically within the first few months after treatment. Monitoring and follow-up are essential to manage and mitigate potential recurrences effectively.
- Long-term Health: Most children and adults recover completely and lead healthy lives with no lasting effects from the episode. However, the specific outcome can depend on how quickly the condition was diagnosed and treated and whether any complications arose during the course of the disease.
However, while intussusception can be a frightening condition, the prognosis is excellent with prompt diagnosis and appropriate treatment. Regular follow-ups are crucial to ensure the health and well-being of the patient post-recovery.
Prevention and Management of Intussusception
Preventing complications in cases of intussusception involves early detection and prompt treatment. Since intussusception is more common in infants and young children, parents and caregivers should be vigilant for symptoms such as acute abdominal pain, vomiting, bloody stools, or a palpable abdominal mass. Recognizing these signs early can lead to quicker diagnosis and treatment, which is crucial in preventing serious complications such as intestinal blockage or perforation.
Here are some practical tips for prevention:
- Regular Check-ups: Routine health examinations can help in identifying any unusual signs or symptoms that might suggest intussusception or other health issues.
- Educational Awareness: Understanding the signs and symptoms of intussusception can empower parents and caregivers to seek immediate medical attention for their child.
- Vaccination: Although research is ongoing, some studies suggest that certain rotavirus vaccines may slightly increase the risk of intussusception. However, the overall benefits of vaccination overwhelmingly outweigh the risks. Stay informed and discuss vaccination with your healthcare provider.
Ongoing Management and Follow-up Care Recommendations
Once an episode of intussusception is resolved, ongoing management is crucial to ensure the health and well-being of the patient. Here are some recommended strategies for follow-up care:
- Post-Treatment Monitoring: After treatment, especially if surgical intervention was involved, regular monitoring is essential. This includes scheduled visits to a pediatrician or gastroenterologist to check for any recurrence of symptoms.
- Diet and Nutrition: Depending on the severity of the condition and the treatment approach, dietary adjustments might be necessary. A healthcare provider might recommend a specific diet to promote healing and adequate nutrition.
- Emotional Support: Experiencing a serious health event like intussusception can be stressful for both the child and the family. Psychological support or counseling might be beneficial to address any emotional distress and to help cope with the experience.
By adhering to these preventative measures and following thorough management and follow-up care, complications from intussusception can be minimized, promoting a smoother recovery and better long-term health outcomes.
FAQs about Intussusception Treatment
What is intussusception?
Intussusception is a medical condition where a part of the intestine folds into an adjacent segment, causing a blockage. This condition is most common in infants and young children but can also occur in adults.
How is intussusception diagnosed?
Intussusception is typically diagnosed through a combination of physical exams, symptoms review, and imaging tests such as an ultrasound or an X-ray. In some cases, an air or barium enema, which also can be therapeutic, is used for both diagnosis and treatment.
What are the treatment options for intussusception?
Treatment for intussusception usually involves a non-surgical approach initially, such as an air or barium enema under image guidance, which can often reduce the intussusception. If this is unsuccessful, or the condition recurs, surgical intervention may be necessary to correct the intestine and remove any damaged sections.
Is intussusception a medical emergency?
Yes, intussusception is considered a medical emergency because it can lead to severe complications like infection, perforation of the intestine, and decreased blood supply to the affected parts of the intestine, which can be life-threatening if not treated promptly.
Can intussusception be prevented?
There are no guaranteed ways to prevent intussusception. However, maintaining a healthy diet and regular medical check-ups can help manage and mitigate potential complications associated with intestinal issues.
What is the recovery time after treatment for intussusception?
Recovery time can vary depending on the severity of the condition and the type of treatment administered. After a successful non-surgical reduction, most children can return to normal activities within a few days, although close monitoring for recurrence is necessary. Surgical recovery may take longer, requiring hospital stays and a period of rest at home.
Conclusion:
Intussusception is a serious medical condition where a part of the intestine slides into an adjacent part, causing a blockage. This can lead to severe symptoms, including pain, swelling, and in severe cases, loss of blood supply to the affected parts of the intestine. Treatment is critical and typically involves procedures such as air or barium enemas, which can often reduce the intussusception non-surgically. In more severe cases, surgical intervention may be necessary to correct the issue and prevent further complications.
If you suspect that you or someone you know might be suffering from intussusception, it is crucial to seek medical consultation immediately. Early diagnosis and treatment are key to a good outcome and can prevent more serious complications, including potential damage to the intestines. Remember, prompt action can make a significant difference in health outcomes for individuals experiencing this condition.
References
For a deeper understanding and further validation of the information provided on intussusception treatment, consider exploring these reputable sources. Each link leads to a well-regarded medical website or journal, offering extensive knowledge and additional details:
- Mayo Clinic – Provides comprehensive insights into the symptoms, diagnosis, and treatments for intussusception. A trusted resource for patient and practitioner information. Read more about intussusception at the Mayo Clinic.
- MedlinePlus – A resource from the U.S. National Library of Medicine, offering detailed descriptions of intussusception, including causes, risk factors, and treatment options. Explore MedlinePlus for more information on intussusception.
- National Institutes of Health (NIH) – Features research articles and clinical updates on intussusception, making it a valuable resource for the latest treatment modalities and outcomes. Visit NIH for recent studies on intussusception treatment.
- Pediatric Emergency Care – An academic journal that includes peer-reviewed articles focused on pediatric emergency medicine, including case studies on intussusception. Ideal for healthcare professionals seeking in-depth analysis. Access Pediatric Emergency Care for scholarly articles on intussusception.
These links are intended to help readers verify facts, gather more data, and pursue a greater understanding of intussusception treatment.