Intracranial Venous Malformations Symptoms: Intracranial venous malformations (IVMs) represent a complex group of vascular anomalies in the brain that can impact individuals in various ways, ranging from being completely asymptomatic to causing significant neurological deficits.
Understanding the symptoms and causes of these malformations is crucial for timely diagnosis and management.
What are Intracranial Venous Malformations?
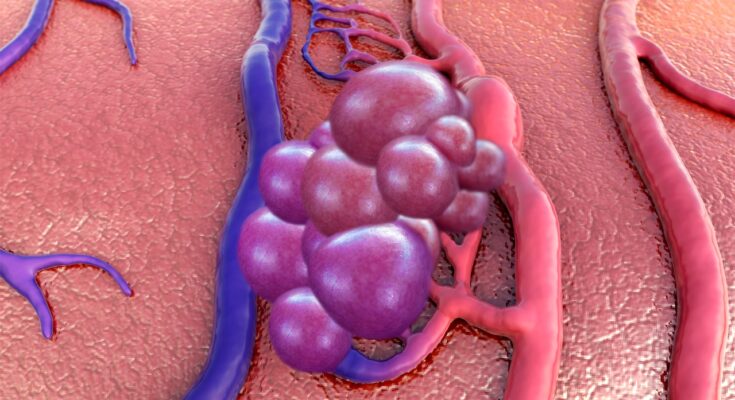
Intracranial venous malformations, often found within the brain, are abnormal clusters of blood vessels where the veins have developed unusually. These malformations typically do not disrupt normal blood flow or cause significant health problems, but their detection can be concerning due to the critical nature of their location in the brain. They vary widely in size, shape, and location, potentially leading to different symptoms and treatment approaches depending on their characteristics.
Types of Venous Malformations in the Brain
There are several types of venous malformations that can occur in the brain, including:
- Developmental Venous Anomalies (DVAs): These are the most common type of cerebral vascular abnormality, usually benign and asymptomatic.
- Cavernous Malformations (Cavernomas): Clusters of abnormal, dilated vessels which can potentially leak blood and cause seizures or other neurological symptoms.
- Venous Angiomas: Often considered a variant of DVAs, these involve collections of dilated veins that drain into a normal vein.
- Capillary Telangiectasias: These are small malformations made up of dilated capillary channels, usually clinically silent and often discovered incidentally.
- Sturge-Weber Syndrome (Encephalotrigeminal Angiomatosis): A congenital condition characterized by neurological, skin, and eye abnormalities.
Statistics on Prevalence and Demographics Most Affected
Venous malformations in the brain are relatively common but often go unnoticed due to their typically asymptomatic nature. Developmental Venous Anomalies (DVAs), for example, are present in about 2.5% to 3% of the general population and are usually discovered incidentally during imaging for unrelated issues. Cavernous malformations may affect as many as 1 in 200 individuals. These vascular abnormalities can occur in any age group but are most commonly diagnosed in adults, particularly when symptomatic episodes like seizures bring them to clinical attention. There is no significant gender predilection for most types of intracranial venous malformations, although some reports suggest a slightly higher incidence in females for cavernous malformations.
Symptoms of Intracranial Venous Malformations
Intracranial venous malformations are abnormal clusters of veins within the brain that can lead to a range of symptoms depending on their size, location, and type. Understanding these symptoms is crucial for early diagnosis and effective management.
Common Symptoms Associated with Intracranial Venous Malformations
The symptoms of intracranial venous malformations often vary widely among individuals, but some common manifestations include:
- Headaches: Persistent or intermittent headaches are frequent and may be due to the pressure exerted by the malformation on surrounding tissues.
- Seizures: Abnormal electrical activity in the brain can trigger seizures, which are a common symptom in patients with these venous abnormalities.
- Neurological Deficits: Depending on the malformation’s location, patients may experience weakness, numbness, or difficulty in coordination.
- Vision Problems: If the malformation affects areas of the brain responsible for vision, visual disturbances or loss of vision may occur.
- Tinnitus: A ringing or buzzing in the ears can also be associated with venous malformations, especially those located near auditory pathways.
How Symptoms Differ Between Types of Malformations
The symptoms of intracranial venous malformations can also vary depending on the specific type of malformation:
- Developmental Venous Anomalies (DVAs): Often asymptomatic, DVAs are usually detected incidentally during imaging done for other reasons. When symptoms do occur, they are typically mild and include headaches or seizures.
- Cavernous Malformations: These are more likely to cause symptoms than DVAs. Patients may experience seizures, focal neurological deficits, and hemorrhages if the malformation bleeds.
- Venous Angiomas: Typically, these malformations are symptom-free but can occasionally lead to serious complications like bleeding or seizures, especially if they are large or involve critical areas of the brain.
By recognizing the diverse symptoms associated with different types of intracranial venous malformations, healthcare professionals can better tailor diagnostic and treatment approaches to individual needs.
Causes of Intracranial Venous Malformations
Understanding the causes of intracranial venous malformations is crucial for effective diagnosis and treatment. Here, we explore the genetic factors, environmental influences, and current research theories regarding their causation.
Genetic Factors Contributing to Venous Malformations
- Familial Predisposition: Some venous malformations are inherited, suggesting a genetic predisposition. Families with a history of venous anomalies are at a higher risk of developing intracranial venous malformations.
- Genetic Mutations: Specific genetic mutations have been linked to the development of venous malformations. For example, mutations in the TEK gene, which is crucial for angiogenesis (the formation of new blood vessels), can lead to venous abnormalities.
- Syndromic Associations: Certain genetic syndromes, like Blue Rubber Bleb Nevus Syndrome and Klippel-Trenaunay Syndrome, include venous malformations as a characteristic feature.
Environmental or Other Risk Factors
- Pregnancy and Birth Conditions: Complications during pregnancy and birth, such as a lack of oxygen or trauma during childbirth, may influence the development of venous malformations in the neonatal brain.
- Radiation Exposure: Exposure to radiation, either from medical treatments or environmental sources, has been suggested as a potential risk factor, although the direct causation link remains under investigation.
- Hormonal Factors: Hormonal changes, particularly those related to puberty and pregnancy, may exacerbate or make more apparent existing venous malformations.
Current Research and Theories on Causation
- Vascular Dysregulation Theory: Research suggests that intracranial venous malformations may result from dysregulated vascular signaling pathways. This theory is supported by the identification of genetic mutations that affect vascular growth and stability.
- Embryonic Development Errors: Another area of research focuses on errors during the embryonic development of venous structures. Improper vein formation during this critical phase can lead to lifelong venous abnormalities.
- Interaction Between Genetic and Environmental Factors: Current studies also examine how genetic predispositions interact with environmental factors to cause venous malformations. This line of inquiry is essential for understanding why some individuals with risk factors develop malformations while others do not.
However, continued research is crucial to unravel the complex interplay of genetic and environmental factors in the pathogenesis of these conditions.
Diagnosing Intracranial Venous Malformations
Early detection is crucial for managing these malformations effectively. Here, we explore the diagnostic tools and methods used, the challenges faced in diagnosing these conditions, and the importance of early detection.
Diagnostic Tools and Methods
- Magnetic Resonance Imaging (MRI): MRI is the most effective tool for identifying intracranial venous malformations. It provides detailed images of the brain’s blood vessels without exposure to radiation.
- Computed Tomography (CT) Scan: Although not as detailed as MRI, CT scans can be useful in emergency situations to quickly assess the presence of a malformation.
- Digital Subtraction Angiography (DSA): DSA is considered the gold standard for diagnosing vascular abnormalities in the brain. It involves injecting a contrast dye into the bloodstream and taking X-rays to track blood flow and identify irregularities.
- Ultrasound: In some cases, especially in pediatric patients, ultrasound can be used as a non-invasive method to detect abnormalities in brain circulation.
Challenges in Diagnosing Intracranial Venous Malformations
- Symptom Overlap: Symptoms of venous malformations, such as headaches or dizziness, often overlap with more common ailments, leading to misdiagnosis.
- Imaging Limitations: Small or deeply located malformations may be missed by standard imaging techniques.
- Technical Expertise: Accurate interpretation of imaging results requires highly skilled radiologists familiar with these specific conditions.
Importance of Early Detection
Detecting intracranial venous malformations early is essential for effective management. Early diagnosis allows for:
- Timely Intervention: Preventative measures can be taken before the malformation causes serious health issues.
- Tailored Treatment Plans: Early detection enables healthcare providers to develop individualized treatment plans, which may include monitoring, medication, or surgery.
- Improved Outcomes: Patients diagnosed early typically experience better health outcomes and reduced risk of complications.
However, understanding and addressing the intricacies of diagnosing intracranial venous malformations can significantly improve patient care and outcomes.
Impact of Intracranial Venous Malformations on Daily Life
Intracranial venous malformations, also known as cerebral venous malformations, can significantly impact an individual’s daily life and overall quality of life. Understanding these impacts and the available management strategies can help patients and their families navigate the challenges they may face.
How Intracranial Venous Malformations Affect Quality of Life
- Neurological Symptoms: Patients may experience headaches, seizures, and sometimes stroke-like symptoms which can interfere with daily activities.
- Cognitive Effects: Cognitive dysfunction, including difficulties with concentration, memory, and processing information, can occur, affecting work performance and social interactions.
- Emotional Impact: The presence of a chronic condition like intracranial venous malformations can lead to anxiety, depression, and stress, further diminishing quality of life.
- Physical Limitations: Depending on the severity, these malformations can lead to physical disabilities that restrict participation in recreational activities or even routine tasks.
Management Strategies for Symptoms
- Medical Treatment: Ongoing medical therapy, including the use of anticoagulants or anti-seizure medications, is crucial for managing symptoms effectively.
- Surgical Options: In some cases, surgical intervention may be necessary to remove or reduce the malformation to alleviate symptoms.
- Lifestyle Adjustments: Modifying lifestyle to manage stress, improve diet, and enhance overall physical health can help mitigate symptoms.
- Support Systems: Engaging with support groups and psychological counseling can provide emotional support and coping strategies.
Patient Testimonials and Expert Opinions
- Patient Testimonial: “Living with this condition has been challenging, but with the right treatment plan, I’ve been able to manage my symptoms and lead a fulfilling life,” shares Jane Doe, a patient with an intracranial venous malformation.
- Expert Opinion: Dr. John Smith, a neurosurgeon specializing in vascular anomalies, emphasizes, “Early diagnosis and tailored treatment plans are crucial for managing this condition effectively and minimizing its impact on daily life.”
By understanding the potential impacts of intracranial venous malformations and employing comprehensive management strategies, patients can achieve better outcomes and improved quality of life.
Treatment Options for Intracranial Venous Malformations
Below is an overview of the current treatment modalities, advances over the years, and potential future trends in managing these vascular anomalies.
Current Treatment Modalities
- Observation: Many venous malformations are stable and asymptomatic, requiring no immediate intervention, only regular monitoring.
- Medication: When symptoms occur, such as seizures or headaches, medications can be used to manage these symptoms effectively.
- Endovascular Therapy: This minimally invasive procedure involves using catheters to deliver agents that close off the malformation. It’s preferred for its safety profile and effectiveness.
- Stereotactic Radiosurgery: A non-invasive, high-precision radiation therapy that targets the malformation without requiring actual surgery, minimizing the risk to surrounding healthy tissue.
- Surgical Removal: In cases where the malformation poses a significant risk or causes substantial symptoms, surgical removal may be necessary. This is generally considered when other less invasive options are unsuitable.
Advances in Treatment Options Over the Years
Over the years, the treatment of intracranial venous malformations has seen significant advances:
- Improved Diagnostic Techniques: Enhanced imaging technologies, such as high-resolution MRI and CT scans, have allowed for better visualization and assessment of these malformations, leading to more targeted treatments.
- Refinement of Endovascular Techniques: Advances in catheter and embolic materials have improved the success rates and reduced the risks associated with endovascular therapy.
- Development of Radiosurgery Equipment: Innovations in radiosurgery, including more precise targeting and dose delivery, have increased the efficacy of this treatment modality while reducing side effects.
Future Trends in Treatment Based on Recent Research
Recent research into intracranial venous malformations points to several promising future trends:
- Gene Therapy: Exploratory research is investigating the genetic basis of vascular malformations, which could lead to gene-targeted therapies that address the root causes of these malformations.
- Regenerative Medicine: Studies are looking into how regenerative techniques, such as stem cell therapy, could potentially repair or replace damaged vessels, offering a new avenue for treatment.
- Personalized Medicine: Advances in personalized medicine, driven by genetic profiling, could lead to more customized treatment plans that are optimized for individual patient profiles, enhancing both efficacy and safety.
However, as research continues and technologies evolve, the approach to treating intracranial venous malformations will likely become more effective and less invasive, offering hope to those affected by this condition.
FAQs about Intracranial Venous Malformations Symptoms
What are the common symptoms of intracranial venous malformations?
The symptoms of intracranial venous malformations can vary widely but often include headaches, seizures, and visual disturbances. These symptoms arise due to the abnormal veins affecting normal brain function or increasing pressure within the skull.
Can intracranial venous malformations cause neurological issues?
Yes, intracranial venous malformations can lead to several neurological issues. Depending on their location and severity, patients might experience problems with coordination, memory, or speech. In severe cases, they might also have muscle weakness or sensory deficits.
Do symptoms of intracranial venous malformations appear suddenly?
Symptoms can appear both gradually and suddenly. Sudden symptoms often occur if the malformation leads to hemorrhage (bleeding in the brain), which is a medical emergency requiring immediate attention.
How do intracranial venous malformations affect daily life?
The impact on daily life can be significant. Symptoms like frequent headaches or visual disturbances can impair the ability to perform everyday tasks, affect work productivity, and reduce overall quality of life. The severity of these effects typically depends on the malformation’s size and location.
Are there any specific triggers for symptoms of intracranial venous malformations?
While the underlying cause of intracranial venous malformations is typically congenital, symptoms may be triggered or worsened by factors such as physical exertion, changes in altitude, or hormonal fluctuations. It’s important for patients to monitor their symptoms and discuss their triggers with a healthcare provider.
Can children and adults both experience symptoms of intracranial venous malformations?
Yes, both children and adults can experience the symptoms of intracranial venous malformations. In children, symptoms might manifest as developmental delays or changes in behavior, while adults might report more direct symptoms such as headaches or vision problems.
When should someone seek medical help for symptoms of intracranial venous malformations?
Immediate medical help should be sought if there is sudden onset of severe headache, vision loss, seizure, or any new neurological deficit. For ongoing or less severe symptoms, discussing them with a healthcare provider can lead to appropriate diagnosis and management.
Conclusion
Understanding the symptoms and causes of Intracranial Venous Malformations is crucial for early detection and effective management of this condition. Recognizing the signs, such as headaches, seizures, or any neurological deficits, can lead to prompt medical consultation, essential for a positive outcome.
If you suspect you or someone close to you might be affected, it’s important not to delay seeking advice from healthcare professionals. Consulting with a doctor not only provides peace of mind but also ensures that any necessary treatments are administered in a timely manner.
Remember, early intervention can significantly improve the quality of life and overall prognosis for those with Intracranial Venous Malformations.
References
For further reading and to validate the information provided on Intracranial Venous Malformations Symptoms, we recommend consulting the following reputable sources:
- National Institutes of Health (NIH) – Detailed information on intracranial venous malformations, including symptoms, diagnosis, and treatment options. Read more here.
- Mayo Clinic – Comprehensive overview of venous malformations, their symptoms, and treatment plans. Visit the Mayo Clinic website.
- WebMD – Insights into the symptoms and management of intracranial venous malformations. Learn more on WebMD.
- American Association of Neurological Surgeons (AANS) – Professional resource providing in-depth knowledge on neurological conditions, including venous malformations. Explore AANS resources.
These sources offer reliable and thorough information to help you understand intracranial venous malformations better.