Intracranial Venous Malformations Treatment: Intracranial venous malformations, often classified under the broader category of vascular anomalies within the brain, present a unique challenge in neurology and neurosurgery.
Understanding the intricacies of their diagnosis and treatment is crucial for medical professionals and patients alike.
These malformations, although sometimes asymptomatic, can lead to serious neurological complications if undetected or improperly managed.
Understanding Intracranial Venous Malformations
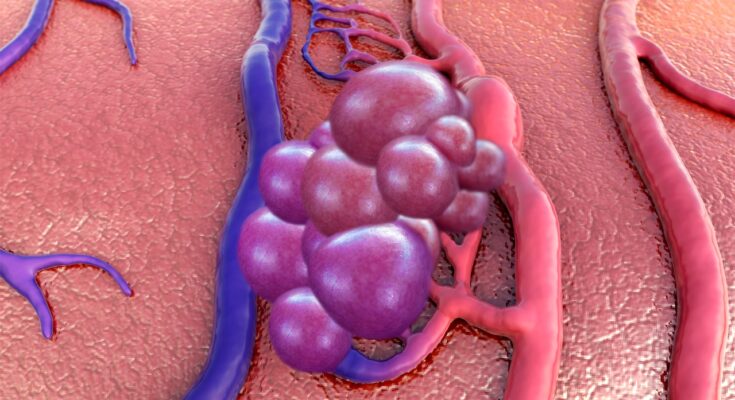
Intracranial venous malformations are abnormal formations of the veins within the brain, which can lead to a variety of health issues if not properly managed. This section explores the different types of these malformations, delves into who is most at risk, and examines the common causes and risk factors associated with them.
Types of Intracranial Venous Malformations
There are several types of intracranial venous malformations, each with unique characteristics and potential implications for brain health:
- Developmental Venous Anomalies (DVAs): These are the most common type of venous malformation and are usually considered benign. DVAs are often found incidentally during imaging for other reasons.
- Cavernous Malformations: These are clusters of abnormal, dilated blood vessels which can cause seizures and headaches. They may occur sporadically or be inherited.
- Venous Angiomas: Often considered a variant of DVAs, these are composed of dilated venous channels and are typically asymptomatic.
- Capillary Telangiectasias: These are small, dilated capillary spaces within the brain that are generally discovered incidentally and rarely cause symptoms.
- Sturge-Weber Syndrome: This is a neurological disorder that involves venous abnormalities along with other symptoms like facial port-wine stains and glaucoma.
Epidemiology: Who is Most at Risk?
Intracranial venous malformations can occur in individuals of any age, gender, or ethnicity. However, certain types may have a predilection towards specific groups:
- Developmental Venous Anomalies are often present at birth, suggesting a developmental origin.
- Cavernous Malformations may have a genetic component, particularly when multiple family members are affected.
- Sturge-Weber Syndrome is present from birth and usually becomes apparent in infancy or early childhood.
Causes and Risk Factors
The exact causes of intracranial venous malformations are not fully understood, but several factors are believed to contribute to their development:
- Genetic Factors: There is a hereditary component in some types, such as cavernous malformations, where specific genetic mutations are identified.
- Developmental Issues: Errors in the development of the vascular system during fetal growth may lead to venous malformations.
- Environmental Factors: While less well-defined, some studies suggest that environmental factors during pregnancy, such as exposure to certain chemicals or radiation, could play a role.
However, regular medical check-ups and imaging studies are often recommended for those known to be at risk, to ensure timely intervention and management.
Symptoms and Risks of Intracranial Venous Malformations
Recognizing the signs and understanding the potential risks associated with these malformations is crucial for timely diagnosis and treatment.
Common Symptoms Associated with Intracranial Venous Malformations
Individuals with intracranial venous malformations may experience a variety of symptoms, which can vary significantly in severity and frequency. Some of the most common symptoms include:
- Headaches: Often the primary symptom, these headaches can vary from mild to severe and may not respond well to typical pain relief methods.
- Seizures: Due to the abnormal vascular structure and potential pressure on the brain, seizures are a common complication of IVMs.
- Neurological deficits: Depending on the location of the malformation, patients might experience issues such as vision problems, muscle weakness, or difficulty with coordination and balance.
- Tinnitus: A ringing or buzzing in the ears can occur if the malformation affects certain veins in the brain.
Potential Complications if Left Untreated
Leaving intracranial venous malformations untreated can lead to serious health complications, including:
- Hemorrhage: One of the most severe risks is bleeding in the brain, which can occur if the malformation ruptures. This can lead to a stroke or other life-threatening conditions.
- Venous congestion: Increased pressure can lead to swelling and impaired blood flow, potentially damaging delicate brain tissue.
- Neurological damage: Over time, the constant pressure and irregular blood flow can cause progressive neurological deterioration, affecting cognitive and physical functions.
Case Studies and Anecdotal Examples
Case studies highlight the critical nature of early diagnosis and intervention. For instance, a study published in a leading neurology journal detailed the case of a 34-year-old patient who presented with unexplained seizures and was later found to have an intracranial venous malformation. After undergoing targeted treatment, the patient’s symptoms significantly improved, underscoring the importance of recognizing the signs early on.
Another anecdotal example involves a teenager who suffered from frequent, debilitating headaches that were initially thought to be migraines. Further investigation revealed an intracranial venous malformation. Treatment not only alleviated her headaches but also prevented potential long-term complications.
These examples demonstrate that while intracranial venous malformations can pose serious health risks, effective outcomes are possible with appropriate medical attention. Awareness of symptoms and timely medical consultation are key in managing the condition effectively, ensuring better health outcomes for those affected.
Diagnostic Techniques for Intracranial Venous Malformations
Effective diagnosis is crucial for managing these conditions. This section will explore the various diagnostic techniques, emphasizing the importance of initial assessments, imaging techniques, advanced diagnostic methods, and the role of differential diagnosis.
Initial Assessment and Medical History Importance
The first step in diagnosing intracranial venous malformations involves a thorough initial assessment and a detailed medical history. Healthcare providers evaluate symptoms such as headaches, seizures, or any neurological deficits that may suggest brain abnormalities. Gathering a comprehensive medical history helps to identify genetic predispositions or any past events that could contribute to venous malformations. This foundational information guides the choice of subsequent diagnostic tests and influences management strategies.
Imaging Techniques
Several imaging modalities are pivotal in diagnosing intracranial venous malformations:
- Magnetic Resonance Imaging (MRI): MRI is the most commonly used imaging technique due to its high sensitivity in detecting abnormal venous structures without exposure to radiation. It can provide detailed images of brain tissues and venous systems.
- Computed Tomography (CT) Scan: Though less detailed for venous structures, CT scans are faster and can be crucial in emergency settings where rapid diagnosis is needed.
- Digital Subtraction Angiography (DSA): DSA offers the most detailed visualization of blood vessels and is considered the gold standard for confirming the diagnosis of venous malformations. It involves injecting a contrast agent into the bloodstream and taking X-rays to trace the flow of blood through the brain’s veins.
- Ultrasonography: Particularly transcranial Doppler ultrasonography, which can be used to assess blood flow in cerebral vessels and detect abnormalities in real-time.
Advanced Diagnostic Methods
Advanced diagnostic methods provide further insights into the nature and extent of venous malformations:
- Functional MRI (fMRI): This technique measures brain activity by detecting changes associated with blood flow. It helps in understanding the impact of malformations on brain function.
- Venous Pressure Monitoring: Invasive but informative, this method measures pressure within the venous system and can help assess the risk of bleeding from malformations.
- Genetic Testing: Useful in cases where a hereditary pattern of venous malformations is suspected, helping to identify specific genetic abnormalities that may influence treatment options.
The Role of Differential Diagnosis
Differential diagnosis is critical in distinguishing intracranial venous malformations from other conditions that could cause similar symptoms, such as arteriovenous malformations, tumors, or cysts. By systematically ruling out these conditions, clinicians can focus on the most effective treatment strategies specific to venous malformations. This process relies heavily on imaging results and clinical presentation and may involve consultations with neurology, radiology, and neurosurgery specialists.
However, the diagnosis of intracranial venous malformations requires a combination of detailed patient history, various imaging techniques, and advanced diagnostic tests. A thorough and accurate diagnosis is essential for developing an effective treatment plan and improving patient outcomes.
Treatment Options for Intracranial Venous Malformations
Intracranial venous malformations, although rare, require carefully considered treatment strategies to manage effectively. These malformations can be treated using surgical methods, non-surgical approaches, and some promising emerging therapies currently under research in clinical trials. Here, we outline the various treatment options available for patients diagnosed with intracranial venous malformations.
Surgical Treatments
Surgical intervention is often considered for intracranial venous malformations that present significant symptoms or pose a high risk of complications. The primary surgical treatments include:
- Microsurgical Resection: This technique involves the removal of the malformation through microsurgical methods, which allows precise dissection and minimizes damage to surrounding brain tissues.
- Endoscopic Surgery: For malformations that are difficult to access, endoscopic surgery can be used. This less invasive approach uses small instruments and cameras to reach and remove the malformation through smaller incisions.
- Stereotactic Radiosurgery (SRS): Although not a traditional surgery, SRS is a non-invasive therapeutic option that uses focused radiation to treat the malformation. It is often used when the malformation is small and surgery is deemed too risky.
Non-surgical Treatments
For patients who are not suitable candidates for surgery or prefer less invasive options, non-surgical treatments can be effective:
- Embolization: This procedure involves the injection of a substance through a catheter into the veins to block blood flow to the malformation, reducing its size and symptomatology.
- Medication: While there are no specific medications to cure venous malformations, certain drugs can be used to manage symptoms such as pain, swelling, and inflammation associated with the condition.
- Observation: In cases where malformations do not cause symptoms or their growth is slow, regular monitoring might be recommended. This approach avoids the risks associated with more invasive treatments.
Emerging Therapies and Clinical Trials
Emerging therapies for intracranial venous malformations include innovative surgical techniques and novel pharmacological treatments. Ongoing clinical trials are crucial for the development of these new options. Current areas of research include:
- Gene Therapy: Exploring the genetic basis of venous malformations to develop targeted treatments that can correct the underlying genetic errors.
- Advanced Imaging Techniques: Developing better imaging technologies to improve the precision of malformation detection, which can enhance treatment planning and outcomes.
- Regenerative Medicine: Using stem cells and other regenerative techniques to repair and replace damaged tissues caused by the malformations.
However, as research continues, the prospects for more effective and less invasive treatments look promising. Patients should consult with a specialist in neurology or neurosurgery to discuss the most appropriate treatment plan based on their specific condition.
Challenges in Treating Intracranial Venous Malformations
Intracranial venous malformations present a complex challenge in medical treatment, stemming from their location in the brain and their variable clinical presentations. The treatment of these vascular anomalies is complicated by several factors, each affecting the approach and potential success of medical interventions.
Complex Decision-Making in Treatment
Deciding on the appropriate treatment for intracranial venous malformations requires careful consideration of numerous patient-specific factors. The age and overall health of the patient, the size and location of the malformation, and the presence of symptoms are critical in shaping the treatment strategy. For instance, asymptomatic malformations discovered incidentally might not require immediate intervention, whereas symptomatic malformations causing seizures or headaches may necessitate more aggressive treatment.
Medical professionals must also weigh the risks of treatment against the potential benefits. Surgical interventions, for example, carry risks of neurological damage and complications from brain surgery. Radiosurgery and pharmacological treatments offer non-invasive alternatives but may not be effective for all types of malformations.
Outcomes and Prognosis
The prognosis for patients with intracranial venous malformations varies widely and is heavily influenced by the characteristics of the malformation and the success of the chosen treatment approach. Generally, patients with smaller, asymptomatic malformations that do not require intervention have a favorable prognosis. In contrast, those requiring surgical or invasive treatments may face a more complicated recovery and a higher risk of post-treatment complications.
Long-term outcomes also depend on the ability to completely remove or stabilize the malformation and manage any associated symptoms. Regular follow-up is essential to monitor for any changes in the malformation’s behavior and to address any new symptoms promptly.
Overall, treating intracranial venous malformations is a delicate balancing act that requires a multidisciplinary approach. Neurosurgeons, radiologists, and neurologists must collaborate to tailor the treatment plan to the individual patient’s needs, optimizing the chances for a successful outcome while minimizing risks.
Case Management and Follow-up of Intracranial Venous Malformations
Intracranial venous malformations (IVMs) require precise and coordinated care due to their complexity and potential impact on brain function. Effective management and long-term follow-up of these conditions are essential for optimizing patient outcomes and enhancing quality of life. Below, we discuss the key strategies for handling IVMs.
Importance of a Multidisciplinary Approach
A multidisciplinary approach is crucial for the successful management of intracranial venous malformations. This involves collaboration among various specialists, including:
- Neurologists: to monitor neurological health and manage any brain function impairments.
- Neurosurgeons: to evaluate surgical options when necessary.
- Radiologists: to assist in detailed imaging that helps in precise diagnosis and monitoring of the malformation.
- Rehabilitation Specialists: to aid in recovery and maintain or improve functional capabilities.
This team works together to devise a personalized treatment plan that addresses both the immediate needs and long-term health of the patient.
Long-term Management and Follow-up Strategies
Long-term management of IVMs includes regular monitoring and various intervention strategies to prevent complications. Key aspects include:
- Routine Imaging Studies: MRI or CT scans are performed periodically to monitor the status of the malformation.
- Medication Management: to address symptoms such as headaches or seizures.
- Regular Clinical Evaluations: to assess neurological status and adjust treatments as needed.
Patients with IVMs require continuous follow-up to adapt to changes in their condition and to promptly address any new symptoms.
Lifestyle Adjustments and Patient Education
Lifestyle adjustments and thorough patient education play a significant role in managing IVMs. Patients are advised to:
- Avoid certain activities: such as those that might excessively increase intracranial pressure.
- Monitor symptoms: learning to recognize new or worsening symptoms is crucial for early intervention.
- Stress Management: engaging in relaxation techniques to help manage stress, which can exacerbate symptoms.
Educating patients about their condition empowers them to take an active role in their health management, helps reduce fear and anxiety, and promotes adherence to treatment plans.
Implementing these comprehensive strategies ensures a proactive approach to the management and follow-up of intracranial venous malformations, aiming to maintain patient health and prevent potential complications.
FAQs about Intracranial Venous Malformations Treatment
What are intracranial venous malformations?
Intracranial venous malformations are abnormal clusters of veins within the brain. These malformations can vary in size and location, and while they are typically benign, they can cause symptoms depending on their position and the effect they have on surrounding brain structures.
How are intracranial venous malformations diagnosed?
These conditions are often diagnosed through imaging studies. Magnetic Resonance Imaging (MRI) is commonly used because it provides detailed images of the brain’s blood vessels and soft tissues. In some cases, a cerebral angiogram may also be recommended to gain a clearer view of the blood flow in the brain’s veins and arteries.
What are the symptoms of intracranial venous malformations?
Many individuals with intracranial venous malformations experience no symptoms at all. However, if symptoms occur, they might include headaches, seizures, hearing or vision changes, and neurological deficits. The specific symptoms largely depend on the location of the malformation.
What treatment options are available for intracranial venous malformations?
Treatment options vary based on the severity and symptoms of the malformation. Options may include monitoring through regular imaging tests, medication to manage symptoms, or surgery. Surgical procedures could involve traditional surgery, endovascular treatment, or radiosurgery, depending on the malformation’s characteristics.
Is surgery always necessary for treating these malformations?
Surgery is not always necessary. Many intracranial venous malformations are discovered incidentally and do not cause any symptoms. In such cases, a conservative approach involving regular monitoring might be recommended. Surgical intervention is typically considered if there is a risk of complications or if the patient is experiencing significant symptoms.
What are the risks associated with treatment?
The risks depend on the type of treatment. Surgical treatments carry risks such as infection, bleeding, or damage to surrounding brain tissue. Non-surgical treatments, such as medication, have their own side effects, which can include allergic reactions or side effects specific to the medication used.
How effective is the treatment for intracranial venous malformations?
The effectiveness of treatment can vary. Many patients experience significant improvement in symptoms and quality of life following treatment. However, as with any medical treatment, outcomes can differ based on individual patient factors and the specific nature of the malformation.
Conclusion
Looking to the future, continuous research is essential to uncover more innovative treatment options and to refine current methodologies. There is a promising path ahead with the potential for breakthroughs in genetic research and minimally invasive surgery that could further revolutionize the management of venous malformations.
For patients and families dealing with these conditions, it’s crucial to seek timely medical advice. Early diagnosis and treatment are key to managing symptoms and preventing complications. Patients are encouraged to maintain regular consultations with their healthcare providers and to stay informed about the latest developments in the field.
By staying proactive about health and supporting ongoing research, we can look forward to improved treatments and a deeper understanding of intracranial venous malformations.
References
For further reading and to validate the information provided on intracranial venous malformations treatment, here are several reputable sources:
- Mayo Clinic – This renowned medical site offers a comprehensive overview of the symptoms, causes, and treatment options for various types of vascular malformations, including those that affect the brain. Read more about vascular malformations at Mayo Clinic.
- National Institutes of Health (NIH) – NIH provides detailed medical information on intracranial venous malformations, including recent research studies and clinical trials. Explore NIH resources on intracranial venous malformations.
- Johns Hopkins Medicine – Known for its pioneering work in medical research, Johns Hopkins offers insights into the diagnosis and treatment of venous malformations, with a focus on innovative treatment methods. Learn more from Johns Hopkins Medicine.
- American Stroke Association – This site provides information about the complications and risks associated with cerebral venous malformations, part of their broader coverage on stroke and cerebrovascular disease prevention. Visit the American Stroke Association.
- Radiopaedia – As a resource for radiologists and other healthcare professionals, Radiopaedia features case studies and detailed imaging examples of intracranial venous malformations, offering a visual understanding of the condition. See case studies on Radiopaedia.
These sources are essential for anyone looking to deepen their understanding of intracranial venous malformations and stay updated on the latest treatment protocols.