Intestinal Obstruction Treatment: Intestinal obstruction is a serious medical condition where the intestines are blocked, preventing the normal passage of contents through the digestive tract. This condition can be life-threatening if not diagnosed and treated promptly.
In this article, we delve into the diagnosis and treatment of intestinal obstruction, providing comprehensive information to help medical professionals and patients understand this condition better.
Understanding Intestinal Obstruction
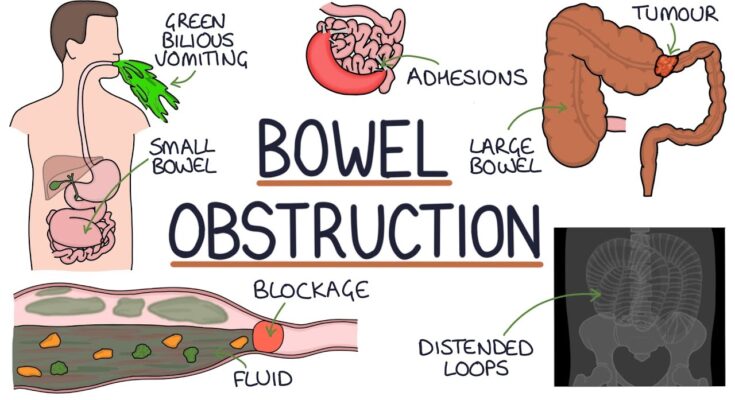
Intestinal obstruction is a serious medical condition where the intestines are partially or completely blocked, preventing the passage of food, fluids, and gas. This can lead to severe complications if not treated promptly. Understanding the types and causes of intestinal obstruction is crucial for early detection and effective management.
Types of Intestinal Obstruction
1. Mechanical Obstruction: This occurs when there is a physical blockage in the intestines.
- Adhesions: Bands of scar tissue that form after surgeries or infections.
- Hernias: When a part of the intestine pushes through a weak spot in the abdominal muscles.
- Tumors: Growths that can block the intestines.
- Volvulus: Twisting of the intestine.
- Intussusception: A condition where a part of the intestine slides into an adjacent part, like a telescope.
2. Functional Obstruction: Also known as paralytic ileus, this occurs when the intestines fail to move contents through due to a malfunction in the muscles or nerves.
- Post-surgical complications: Often seen after abdominal surgery.
- Infections: Such as gastroenteritis or appendicitis.
- Medications: Certain drugs can slow down intestinal movements.
Common Causes of Intestinal Obstruction by Age Group
Understanding the typical causes of intestinal obstruction in different age groups helps in timely diagnosis and treatment.
1. Infants and Children:
- Intussusception: The most common cause in children, often seen in those aged 6 months to 3 years.
- Congenital Malformations: Birth defects like atresia or stenosis of the intestines.
- Hirschsprung’s Disease: A condition where nerve cells are missing in parts of the intestine.
2. Adults:
- Adhesions: The most common cause in adults, especially those with a history of abdominal surgeries.
- Hernias: Particularly inguinal hernias that can trap parts of the intestine.
- Tumors: Both benign and malignant growths can obstruct the intestines.
3. Elderly:
- Diverticulitis: Inflammation of diverticula, which are small pouches that can form in the intestines.
- Colon Cancer: A significant cause of obstruction in older adults.
- Volvulus: More common in elderly due to weakened intestinal muscles.
However, early medical intervention can prevent complications and improve outcomes. If you suspect an intestinal obstruction, seek immediate medical attention.
Symptoms of Intestinal Obstruction
Recognizing the early signs and symptoms can be crucial for effective management. Below, we explore the early indications, critical symptoms, risk factors, and potential complications associated with intestinal obstruction.
Early Signs of Intestinal Obstruction
The initial symptoms of an intestinal obstruction may be mild but gradually worsen. Early detection is key to preventing severe complications. Here are common early signs that might indicate an obstruction:
- Abdominal Pain: Mild to severe cramping pain that comes and goes, usually starting suddenly and occurring around the belly button or lower abdomen.
- Bloating or Swelling: An early sign that is often overlooked, where the abdomen feels full and tight.
- Decreased Appetite: A sudden loss of appetite or feeling full after eating only a small amount.
- Nausea or Vomiting: Frequent vomiting, which can include vomiting after eating.
- Constipation: Inability to have a bowel movement or pass gas.
- Diarrhea: In cases where the obstruction is partial, liquid stool may bypass the blockage.
Symptoms That Necessitate Immediate Medical Attention
Some symptoms of intestinal obstruction are particularly severe and warrant immediate medical intervention. If you experience any of the following, seek emergency care:
- Intense, Constant Abdominal Pain: Pain that does not subside and is sharp and severe.
- Vomiting Bile or Blood: Vomiting greenish-yellow fluid (bile) or blood is a critical sign.
- High Fever: A fever over 101°F (38°C) can indicate an infection or inflammation.
- Rapid Heart Rate: Feelings of faintness or a heart rate that’s much quicker than usual.
- Abdominal Tenderness or Rigidity: The abdomen may feel hard to the touch and be very sensitive to pressure.
- Altered Consciousness: Confusion or reduced alertness can occur in severe cases.
Risk Factors and Potential Complications
Several factors can increase the risk of developing an intestinal obstruction. These include previous abdominal or gastrointestinal surgery, which can lead to scar tissue (adhesions), certain intestinal diseases like Crohn’s disease or diverticulitis, and cancers that affect the abdominal organs.
If left untreated, intestinal obstruction can lead to severe, life-threatening complications such as:
- Strangulation: A part of the intestine becomes cut off from its blood supply, leading to tissue death.
- Perforation: A hole may form in the wall of the intestine, which is a medical emergency.
- Infection and Sepsis: Leakage from the intestine can cause infection in the abdominal cavity (peritonitis) and lead to sepsis, a severe and widespread infection.
If you suspect you or someone else is experiencing symptoms of intestinal obstruction, do not hesitate to seek medical attention immediately.
Diagnosing Intestinal Obstruction
Here’s a comprehensive guide to understanding how intestinal obstruction is diagnosed, incorporating common diagnostic tests and the importance of medical history and physical examinations.
Step-by-Step Approach to Diagnosis
- Initial Assessment: The first step in diagnosing intestinal obstruction involves a thorough assessment by your healthcare provider. This includes discussing your symptoms, which may range from severe abdominal pain and vomiting to constipation and inability to pass gas.
- Medical History Review: Your doctor will review your medical history, asking about any past abdominal surgeries, medications, and chronic health conditions. This helps to identify any potential causes or risk factors for intestinal obstruction.
- Physical Examination: During the physical exam, your doctor will check for signs of intestinal obstruction. This includes examining your abdomen for tenderness, swelling, and listening to sounds within the stomach using a stethoscope. The presence of high-pitched sounds when listening to the abdomen can often indicate an obstruction.
Common Diagnostic Tests and Imaging Techniques
- X-rays: This is often the first imaging test used to look for signs of obstruction in the intestines. An X-ray can show gas, fluid, or sometimes the actual site where the blockage occurs.
- Computed Tomography (CT) Scan: A CT scan provides a more detailed view and can help the doctor see the exact location and cause of the obstruction. It’s particularly useful in diagnosing complicated cases.
- Ultrasound: In some cases, an ultrasound may be performed to view the intestines and surrounding areas, especially in infants and young children.
- Blood Tests: Blood tests can check for signs of infection, inflammation, or electrolyte imbalances, which can occur with obstructions.
- Barium Enema: A special X-ray of the large intestine that involves filling the colon with a liquid called barium. This can help to outline any obstructions.
Role of Medical History and Physical Examinations
Understanding a patient’s medical history and conducting a physical examination are crucial components of diagnosing intestinal obstruction. These initial steps can provide essential clues and help differentiate between a mechanical obstruction (where something physically blocks the intestine) and a functional obstruction (where the intestine’s movement is impaired without a physical blockage). For instance, a history of abdominal surgeries might suggest the possibility of adhesions, which are a common cause of mechanical obstruction.
However, diagnosing intestinal obstruction requires a careful and methodical approach that starts with a detailed medical history and physical examination, followed by specific diagnostic tests. Early and accurate diagnosis can significantly enhance the effectiveness of treatment and improve patient outcomes. If you experience symptoms of intestinal obstruction, such as severe abdominal pain, vomiting, or inability to pass gas, it is important to contact your healthcare provider immediately.
Treatment Options for Intestinal Obstruction
Understanding the general treatment strategies, medications, surgical interventions, and nutritional support options can help in managing this medical emergency effectively.
General Treatment Strategies Based on Severity and Type
- Observation and Monitoring: In cases of partial and uncomplicated obstructions, doctors may recommend a wait-and-see approach, closely monitoring the patient’s condition to see if the obstruction resolves on its own.
- Decompression: For mechanical obstructions, a nasogastric tube may be inserted through the nose into the stomach to relieve pressure, drain contents, and decompress the bowel.
- Fluids and Electrolytes: Rehydration through intravenous fluids is critical to prevent dehydration and electrolyte imbalances, which are common in patients with intestinal obstructions.
- Pain Management: Appropriate pain management is provided to alleviate discomfort caused by the obstruction.
Medications
- Anti-emetics: These are used to control nausea and vomiting, common symptoms of intestinal obstruction.
- Analgesics: Pain relief medications are administered to help alleviate abdominal pain.
- Antibiotics: If the obstruction has led to an infection or there’s a risk of infection, antibiotics are prescribed.
- Laxatives or Stool Softeners: In certain types of obstructions, these may be used to help resolve milder cases or functional obstructions without surgery.
Surgical Interventions
- Laparotomy: A surgical procedure where an incision is made in the abdomen to remove the obstruction directly.
- Laparoscopy: A less invasive form of surgery using small incisions and a camera to guide the surgery, suitable for certain types of blockages.
- Strictureplasty: In cases involving narrowed areas of the bowel, this procedure can widen the narrow sections without removing any part of the intestine.
- Colostomy or Ileostomy: These procedures involve creating an opening in the abdominal wall to divert waste into an external bag; these may be temporary or permanent, depending on the situation.
Nutritional Support and Management During Treatment
- Parenteral Nutrition: If the intestines need to rest and heal, nutrition may be provided intravenously to bypass the gastrointestinal tract.
- Enteral Nutrition: In some cases, a special diet or feeding via a tube may be introduced if part of the bowel is still functional.
- Dietary Adjustments: Once the obstruction is resolved or managed, dietary adjustments are often necessary to ease the transition back to normal eating and to support overall bowel health.
- Monitoring and Adjustment: Nutritional plans are closely monitored and adjusted based on the patient’s recovery progress, tolerance, and nutritional needs.
However, the treatment of intestinal obstructions involves a combination of medical management, surgical intervention, and meticulous nutritional support.
Recovery and Management Post-Treatment of Intestinal Obstruction
After undergoing treatment for an intestinal obstruction, managing your recovery effectively is crucial to ensure a smooth transition back to daily life. This phase involves understanding what to expect during the recovery period, adopting appropriate dietary and lifestyle changes, and recognizing the importance of follow-up appointments. Here’s a detailed breakdown:
What to Expect During the Recovery Period
- Rest and Gradual Activity Resumption: Initially, rest is vital. Over time, gradually increase your activity level as recommended by your healthcare provider.
- Symptom Monitoring: Pay close attention to symptoms such as abdominal pain, nausea, vomiting, or constipation. Immediate medical attention is required if these symptoms recur.
- Wound Care: If your treatment involved surgery, proper care of the incision site is essential to prevent infection.
- Hydration and Nutrition: Staying hydrated and following nutritional guidelines provided by your healthcare team is crucial during the recovery.
Dietary Management and Lifestyle Adjustments Post-Treatment
- Gradual Dietary Introduction: Start with clear liquids and gradually reintroduce solid foods as tolerated, following your doctor’s advice closely.
- Balanced Diet: Once you can tolerate regular foods, maintain a balanced diet rich in fiber to help regular bowel movement and reduce the chances of a recurring obstruction.
- Avoiding Certain Foods: Initially, you may need to avoid high-fiber foods, nuts, seeds, and raw vegetables until your intestine heals completely.
- Regular Exercise: Incorporating gentle exercise, such as walking, can improve digestion and overall health without straining your abdomen.
Importance of Follow-Up Appointments to Monitor Progress
- Monitoring Recovery: Regular check-ups allow your doctor to monitor your healing process, manage any complications, and adjust treatments as necessary.
- Adjusting Medications and Diet: These appointments are crucial for making necessary adjustments to medications and dietary recommendations based on your recovery progress.
- Early Detection of Potential Issues: Follow-up visits help in the early detection of signs that may indicate complications or a recurrence of the obstruction.
However, ensuring consistent follow-ups, adhering to dietary recommendations, and gradually increasing physical activity can help manage and mitigate potential risks post-treatment.
Prevention and Awareness of Intestinal Obstruction
- Maintain a Fiber-Rich Diet: Consuming a diet high in fiber can help keep your digestive system functioning smoothly. Incorporate whole grains, fruits, vegetables, and legumes into your meals to promote regular bowel movements and prevent constipation, a common cause of intestinal obstruction.
- Stay Hydrated: Drinking plenty of water aids in digestion and helps prevent the formation of hard stools that can lead to blockages. Aim for at least 8 glasses of water a day to keep your intestines healthy.
- Regular Exercise: Physical activity stimulates intestinal contractions, which helps move food through your digestive system. Aim for at least 30 minutes of moderate exercise most days of the week, such as walking, jogging, or swimming.
- Avoid Heavy or Indigestible Foods: Be cautious with foods that are difficult to digest, such as large quantities of nuts, seeds, and certain fibrous vegetables. Chew your food thoroughly and eat smaller, more frequent meals to reduce the risk of obstruction.
- Manage Underlying Conditions: Conditions like Crohn’s disease, diverticulitis, and hernias can increase the risk of intestinal obstructions. Work with your healthcare provider to manage these conditions effectively.
Role of Diet, Physical Activity, and Regular Medical Check-Ups
- Diet: A balanced diet rich in fiber, fluids, and essential nutrients plays a crucial role in maintaining intestinal health. Avoiding foods that are known to cause blockages and eating a variety of fruits and vegetables can keep your digestive system in optimal condition.
- Physical Activity: Regular exercise not only promotes overall health but also enhances intestinal motility, reducing the likelihood of obstructions. Activities such as yoga, cycling, and brisk walking can be particularly beneficial.
- Regular Medical Check-Ups: Routine check-ups with your healthcare provider can help detect and manage potential issues before they develop into serious problems. Regular screenings and diagnostic tests can identify early signs of conditions that may lead to obstructions.
Educating the Public on Recognizing Early Signs of Obstruction
Public awareness is key to preventing severe complications from intestinal obstructions. Educate people on the following early signs:
- Abdominal Pain and Cramping: Persistent or severe abdominal pain can indicate a blockage. If the pain is accompanied by bloating, it’s essential to seek medical attention.
- Constipation and Inability to Pass Gas: A sudden change in bowel habits, especially if you cannot pass gas or have a bowel movement, can signal an obstruction.
- Nausea and Vomiting: Persistent nausea and vomiting, particularly if they occur without an obvious cause like food poisoning, can be a warning sign.
- Abdominal Swelling: Noticeable swelling or distention of the abdomen can be a symptom of a blockage.
By promoting awareness and educating the public on these early signs, we can ensure timely medical intervention and reduce the risk of severe complications associated with intestinal obstructions.
FAQs about Intestinal Obstruction Treatment
What is an intestinal obstruction?
An intestinal obstruction is a blockage that prevents food or liquid from passing through your small or large intestine. It can be caused by various factors such as scar tissue, tumors, or hernias.
What are the symptoms of an intestinal obstruction?
Common symptoms include severe abdominal pain, vomiting, bloating, and an inability to pass gas or stool. If you experience these symptoms, seek medical attention immediately.
How is an intestinal obstruction diagnosed?
Doctors use a combination of physical exams, imaging tests like X-rays or CT scans, and blood tests to diagnose an intestinal obstruction.
What treatments are available for an intestinal obstruction?
Treatment depends on the severity and cause of the obstruction. Mild cases may be managed with medication and a special diet. Severe cases might require hospitalization, where treatments could include intravenous fluids, nasogastric tubes, or surgery.
Can intestinal obstructions be prevented?
While not all obstructions can be prevented, maintaining a healthy diet, staying hydrated, and managing underlying conditions like Crohn’s disease can reduce your risk.
When should I seek emergency care for an intestinal obstruction?
Seek emergency care if you experience sudden, severe abdominal pain, persistent vomiting, or signs of dehydration, such as dizziness and low urine output. These symptoms could indicate a life-threatening condition requiring immediate treatment.
Conclusion
Recognizing and treating intestinal obstruction promptly is crucial for preventing severe complications and ensuring a swift recovery. Early detection can significantly improve outcomes and reduce the risk of long-term health issues.
If you suspect you or a loved one may have an intestinal obstruction, seek medical advice immediately. Timely intervention can make all the difference in your health and well-being.
Don’t hesitate to consult a healthcare professional if you experience symptoms like severe abdominal pain, vomiting, or inability to pass stool. Your health is too important to wait.
References
To ensure the accuracy and reliability of the information provided in our guide on Intestinal Obstruction Treatment, we have cited reputable sources. For further reading and validation, please refer to the following links:
- Mayo Clinic: Intestinal Obstruction
- Johns Hopkins Medicine: Intestinal Obstruction
- National Institute of Diabetes and Digestive and Kidney Diseases: Treatment for Intestinal Obstruction
These sources provide comprehensive insights into the causes, symptoms, and treatments of intestinal obstruction, ensuring you have access to trustworthy and detailed information.