Hypospadias Treatment: Hypospadias is a congenital condition affecting the urethra in males where the urethral opening is not located at the tip of the penis but along the underside.
This condition can vary in severity and has implications for both urinary function and reproductive health.
Understanding the diagnosis and treatment options is crucial for effective management and improved outcomes.
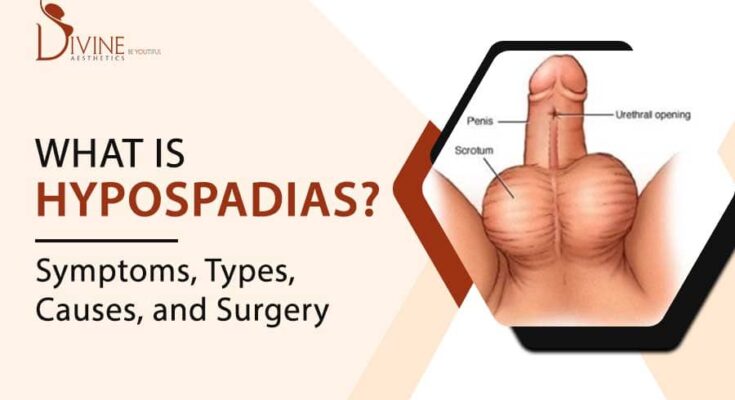
What is Hypospadias?
Hypospadias is a congenital condition in which the opening of the urethra is not located at the tip of the penis. Instead, the urethral opening is positioned anywhere along the underside of the penis, ranging from just below the tip to the scrotum. This abnormality can affect urination, sexual function, and the cosmetic appearance of the penis. The exact cause of hypospadias is not fully understood but is thought to involve a combination of genetic and environmental factors.
Statistics on Prevalence and Demographics Affected
Hypospadias is one of the most common congenital abnormalities in males, affecting approximately 1 in every 200 to 300 live male births. The prevalence of hypospadias can vary based on geographic and ethnic factors. For instance, higher rates have been observed in certain European countries and North America compared to Asia. The condition is more likely to occur in infants of mothers who experienced certain environmental exposures or used specific medications during pregnancy. It is also more prevalent in premature infants and those with a family history of hypospadias.
Discussion of Typical Anatomy vs. Hypospadias
In typical male anatomy, the urethra opens at the tip of the penis, facilitating straightforward urination and reproductive functions. In contrast, with hypospadias, the urethral opening is abnormally located along the underside of the penis. This can lead to several functional issues:
- Direction of Urine Stream: The abnormal location of the urethral opening can affect the direction and flow of urine, potentially causing difficulties with urination.
- Cosmetic Appearance: The physical appearance of the penis can be notably different, which may affect psychological and emotional well-being.
- Sexual Function: Depending on the severity of the condition, hypospadias can interfere with sexual functions in later life.
However, corrective surgery is typically recommended to improve the function and appearance of the penis, with most procedures being performed during early childhood to achieve optimal outcomes.
Causes and Risk Factors of Hypospadias
Understanding the causes and risk factors associated with hypospadias can help in early diagnosis and management. This condition is influenced by a combination of genetic and environmental factors, as well as potential prenatal influences.
Genetic and Environmental Factors
- Genetic Susceptibility: There is a significant genetic component to hypospadias. A family history of hypospadias increases the risk, suggesting the involvement of genetic mutations or hereditary traits that contribute to the condition.
- Hormonal Influences: The development of the male urethra is hormone-dependent, primarily relying on androgens (male hormones). Disruptions in androgen production or action can lead to the development of hypospadias.
- Environmental Chemicals: Exposure to certain environmental chemicals that disrupt endocrine function can increase the risk of hypospadias. These include pesticides, PCBs (polychlorinated biphenyls), and phthalates, which can interfere with hormonal balances during critical periods of fetal development.
Potential Prenatal Influences
- Maternal Diet and Nutrition: Poor maternal nutrition, especially a deficiency in certain nutrients like folic acid, has been linked to an increased risk of congenital abnormalities including hypospadias.
- Maternal Age: Advanced maternal age is associated with a slightly increased risk of having a child with hypospadias.
- Medications During Pregnancy: Use of certain medications during pregnancy, such as progesterone or other hormones, has been linked to a higher incidence of hypospadias in newborns.
Risk Assessment and Prevention Strategies
- Genetic Counseling: For families with a history of hypospadias, genetic counseling may be recommended. This can help prospective parents understand the risks and the genetic aspects of the condition.
- Avoiding Harmful Exposures: Pregnant women should avoid exposure to known endocrine disruptors and harmful chemicals. Adhering to safety guidelines regarding chemical exposure can help reduce the risk.
- Prenatal Care: Regular prenatal check-ups can help monitor fetal development and catch potential issues early. Adequate intake of essential nutrients, such as folic acid, during pregnancy is crucial.
Implementing effective risk assessment and preventive strategies can significantly contribute to the health outcomes of those affected.
Symptoms and Signs of Hypospadias
Hypospadias is a congenital condition in which the opening of the urethra is not located at the tip of the penis. Recognizing the symptoms early can lead to timely medical intervention and better outcomes.
List of Symptoms of Hypospadias
- Abnormal Urethral Opening: The urethral opening may be located along the shaft of the penis, at the base, or even within the scrotum.
- Downward Curvature of the Penis (Chordee): A noticeable downward curve of the penis, especially during an erection.
- Hooded Appearance of the Penis: The foreskin may form a hooded shape due to the abnormal location of the urethral opening.
- Spraying of Urine: Difficulty controlling the direction of urine flow.
- Incomplete Foreskin: Missing or incomplete foreskin on the underside of the penis.
Common Complications and Associated Conditions
Hypospadias can lead to several complications if not treated:
- Difficulty with Urination: Abnormal urine flow can make urination challenging.
- Sexual Dysfunction: If left untreated, the condition can cause problems with sexual function later in life.
- Fertility Issues: Severe cases can impact sperm delivery during ejaculation.
- Inguinal Hernia: Some children with hypospadias may also have a hernia in the groin area.
- Undescended Testicles: There is an increased likelihood of undescended testicles in children with hypospadias.
When to Seek Medical Advice
It’s crucial to seek medical advice if you notice any symptoms of hypospadias in your child. Early diagnosis and treatment, typically within the first year of life, can prevent complications. Consult a pediatric urologist if your child exhibits:
- A urethral opening in an abnormal location.
- Difficulty or abnormal spraying during urination.
- Noticeable downward curvature of the penis.
Early intervention can often correct the condition with surgical procedures, leading to normal urinary and sexual function.
By being aware of these symptoms and signs, you can ensure timely medical care for hypospadias, reducing the risk of complications and improving long-term outcomes.
Diagnosing Hypospadias
Diagnosing hypospadias involves a series of specific diagnostic procedures and medical exams to ensure accurate identification and proper treatment planning. Here’s a comprehensive look at the steps and considerations in diagnosing this condition:
List of Diagnostic Procedures and Medical Exams
- Physical Examination: The primary step in diagnosing hypospadias is a thorough physical examination by a healthcare professional. The doctor will examine the penis to assess the position and appearance of the urethral opening, the foreskin, and the curvature of the penis (chordee).
- Ultrasound: In some cases, an ultrasound may be recommended to evaluate the urinary tract and detect any associated abnormalities in the kidneys or bladder.
- Voiding Cystourethrogram (VCUG): This imaging test helps visualize the urinary tract and bladder during urination, checking for any abnormalities or obstructions.
- Genetic Testing: Genetic tests might be performed if there are concerns about underlying genetic conditions that could be associated with hypospadias.
Role of Pediatric Urologists in Diagnosis
Pediatric urologists play a crucial role in diagnosing hypospadias. These specialists are trained to identify and treat urinary and genital conditions in children. Their expertise is essential for several reasons:
- Expert Evaluation: Pediatric urologists have the skills and experience to accurately assess the severity and type of hypospadias.
- Tailored Treatment Plans: They can develop individualized treatment plans based on the specific needs of each child.
- Surgical Expertise: If surgery is necessary, pediatric urologists are proficient in performing the delicate procedures required to correct hypospadias.
Importance of Early Detection
Early detection of hypospadias is vital for several reasons:
- Better Outcomes: Early diagnosis allows for timely intervention, which can significantly improve surgical outcomes and overall health.
- Preventing Complications: Identifying hypospadias early helps prevent complications such as urinary difficulties, infections, and issues with sexual function later in life.
- Parental Support: Early detection provides parents with the necessary information and support to make informed decisions about their child’s care.
By understanding the diagnostic procedures, the critical role of pediatric urologists, and the importance of early detection, parents and caregivers can ensure the best possible care for children with hypospadias.
Treatment Options for Hypospadias
Treatment options vary depending on the severity and specific presentation of the condition. Below, we detail surgical interventions, non-surgical management, and recent innovations in hypospadias surgery.
Surgical Interventions for Hypospadias
Surgical treatment is the most common approach to correcting hypospadias. The primary goals are to create a functional and cosmetically normal penis. The key surgical procedures include:
- Urethroplasty: This procedure involves constructing a new urethral channel. Surgeons may use tissue grafts from the foreskin, mouth, or other parts of the body to create a new urethra.
- Chordee Repair: Chordee, or penile curvature, is often associated with hypospadias. Surgical correction of chordee involves straightening the penis by releasing fibrous tissue.
- Meatoplasty and Glanuloplasty: These procedures focus on reshaping the urethral opening (meatus) and the glans (head) of the penis to ensure a more natural appearance and function.
- Two-stage Repair: For more severe cases, a two-stage repair might be necessary. The first stage typically involves straightening the penis and the second stage focuses on creating the new urethral channel.
Non-surgical Management and Supportive Care
While surgery is the primary treatment for hypospadias, some cases may benefit from non-surgical management and supportive care. These options include:
- Hormonal Therapy: In certain cases, hormone therapy, such as topical or injectable testosterone, can stimulate penile growth, making subsequent surgical procedures easier.
- Psychological Support: Hypospadias can impact a child’s self-esteem and body image. Providing psychological support and counseling can help address these emotional challenges.
- Monitoring and Follow-up: Regular follow-up appointments with a pediatric urologist are essential to monitor the condition and ensure that any complications are promptly addressed.
Innovations in Hypospadias Surgery
Recent advancements in medical technology and surgical techniques have significantly improved the outcomes of hypospadias surgery. Notable innovations include:
- Tissue Engineering: Researchers are exploring the use of bioengineered tissues to create urethral substitutes, which may offer better integration and reduced complications.
- Minimally Invasive Techniques: Advances in minimally invasive surgical techniques, such as laparoscopic and robotic-assisted surgery, are reducing recovery times and improving precision.
- 3D Printing: The use of 3D printing technology to create customized surgical models helps surgeons plan and execute complex hypospadias repairs with greater accuracy.
- Enhanced Imaging: Improved imaging techniques, including high-resolution ultrasound and MRI, allow for more detailed preoperative planning and assessment of the condition.
However, ongoing innovations continue to enhance the effectiveness and safety of these treatments, offering hope for improved quality of life for those affected by this condition.
Preparing for Hypospadias Surgery
Pre-operative Considerations and Evaluations
Before hypospadias surgery, thorough pre-operative evaluations are essential to ensure the best outcomes. These evaluations typically include:
- Medical History Review: Your child’s complete medical history will be reviewed to identify any potential risks or complications.
- Physical Examination: A detailed physical exam will be conducted, focusing on the genital area to assess the severity of hypospadias.
- Imaging Tests: In some cases, imaging tests like an ultrasound may be required to get a clearer view of the urinary tract.
- Consultation with Specialists: Meeting with a pediatric urologist and anesthesiologist to discuss the procedure, anesthesia plan, and post-operative care.
What Parents Can Expect Before, During, and After Surgery
Before Surgery:
- Pre-operative Instructions: Follow specific instructions provided by the surgical team, including fasting guidelines and medication management.
- Emotional Preparation: Prepare your child for surgery by explaining the process in a calm and reassuring manner. Using age-appropriate language can help reduce anxiety.
- Packing Essentials: Bring necessary items for your child’s comfort, such as their favorite toy, blanket, or book, to the hospital.
During Surgery:
- Duration: Hypospadias surgery typically lasts 1-2 hours, but this can vary based on the complexity of the case.
- Anesthesia: Your child will be under general anesthesia to ensure they are comfortable and pain-free during the procedure.
- Surgical Team: A skilled team of pediatric urologists and nurses will perform the surgery, using specialized techniques to correct the condition.
After Surgery:
- Recovery Room: Your child will be monitored in a recovery room until the effects of anesthesia wear off.
- Pain Management: Pain relief medications will be administered as needed. The surgical team will provide guidance on managing pain at home.
- Follow-up Care: Scheduled follow-up appointments are crucial to monitor healing and address any concerns. The first follow-up is usually within a week of surgery.
Psychological Preparation for the Child and Family
Preparing psychologically for hypospadias surgery is vital for both the child and the family:
- Educate and Reassure: Explain the procedure to your child using simple and reassuring words. Books or videos designed for children about medical procedures can be helpful.
- Open Communication: Encourage your child to express their feelings and ask questions. Address their fears and reassure them that it’s okay to feel anxious.
- Support System: Lean on family and friends for emotional support. Consider speaking with a child psychologist if your child exhibits significant anxiety.
- Parental Self-care: Take care of your own emotional health. Children often take cues from their parents, so staying calm and positive can help your child feel more secure.
By understanding these pre-operative considerations, managing expectations, and preparing psychologically, parents can help their child navigate hypospadias surgery with confidence and ease.
Post-Surgical Care and Outcomes of Hypospadias
Immediate Postoperative Care Requirements
After hypospadias surgery, meticulous postoperative care is essential to ensure optimal healing and prevent complications. The primary focus during the immediate postoperative period includes pain management, infection prevention, and monitoring the surgical site for any signs of complications.
- Pain Management: Administer prescribed pain medications as needed to keep your child comfortable. Follow the dosage instructions carefully to avoid any adverse effects.
- Hygiene and Wound Care: Keep the surgical area clean and dry. Follow your healthcare provider’s instructions on how to clean the area and change dressings, if necessary.
- Catheter Care: If a catheter is in place, ensure it remains unobstructed and follow instructions for its care to prevent urinary tract infections.
- Activity Restrictions: Limit your child’s physical activities to avoid putting stress on the surgical site. Encourage quiet activities and prevent any rough play that could disrupt healing.
Long-Term Follow-Up and Monitoring
Long-term follow-up care is crucial to monitor the healing process and identify any potential complications early. Regular check-ups with your healthcare provider will ensure that your child’s recovery is progressing well and that the surgical outcomes are satisfactory.
- Scheduled Visits: Attend all scheduled postoperative appointments. These visits allow the surgeon to assess the healing process and make any necessary adjustments to the care plan.
- Monitoring Urination: Observe your child’s urination pattern. Report any difficulties, pain, or unusual symptoms to your healthcare provider immediately.
- Growth and Development: As your child grows, ongoing monitoring of the surgical site is important to ensure that there are no issues with the function or appearance of the penis.
Success Rates and Potential Complications
Hypospadias surgery has a high success rate, with most children experiencing positive outcomes and normal urinary and sexual function. However, as with any surgical procedure, there are potential complications to be aware of.
1. Success Rates: The majority of hypospadias surgeries are successful, resulting in a normally functioning and aesthetically pleasing penis. Success rates vary depending on the severity of the condition and the type of surgical technique used.
2. Potential Complications: While uncommon, some potential complications include:
- Fistula Formation: An abnormal connection between the urethra and the skin can develop, requiring additional surgery.
- Urethral Stricture: Narrowing of the urethra can occur, leading to difficulty urinating and necessitating further intervention.
- Cosmetic Issues: Occasionally, additional procedures may be needed to achieve the desired cosmetic outcome.
By following medical advice and maintaining regular follow-up appointments, most children can achieve excellent results and lead healthy, normal lives.
Challenges in Hypospadias Treatment
Common Surgical Challenges and Their Solutions
Hypospadias, a congenital condition where the urethral opening is not located at the tip of the penis, presents several surgical challenges. Surgeons frequently encounter issues such as:
- Meatal Stenosis: Narrowing of the urethral opening is a common problem. This is typically addressed through careful surgical technique and postoperative monitoring to ensure proper healing and function.
- Urethrocutaneous Fistula: This occurs when there is an abnormal connection between the urethra and the skin. Surgeons often use tissue grafts and flaps to repair these fistulas, followed by meticulous suturing to prevent recurrence.
- Curvature (Chordee): Correcting penile curvature requires precise dissection and sometimes the use of grafts to straighten the penis. Techniques like dorsal plication or ventral lengthening are employed based on the severity of the curvature.
- Graft Rejection: In cases where tissue grafts are used, there is a risk of rejection. Surgeons mitigate this by using autologous tissue (from the patient’s own body) whenever possible and ensuring proper vascularization of the graft.
Dealing with Complications and Revision Surgeries
Complications in hypospadias surgery can necessitate revision procedures. Some common complications include:
- Urethral Stricture: This narrowing of the urethra can be managed through dilation, endoscopic procedures, or, in severe cases, additional surgery to reconstruct the urethra.
- Infection: Postoperative infections are managed with antibiotics and proper wound care. Preventive measures during surgery, such as maintaining a sterile field, are crucial.
- Aesthetic Concerns: Ensuring a natural appearance can be challenging. Surgeons aim to achieve optimal cosmetic outcomes through careful planning and advanced techniques.
Revision surgeries are sometimes required to address these complications. Each revision is tailored to the specific issue, whether it’s a fistula repair, stricture management, or aesthetic enhancement.
The Impact of Recent Research on Treatment Approaches
Recent research has significantly influenced the approaches to hypospadias treatment. Innovations in surgical techniques and postoperative care have improved outcomes. Key advancements include:
- Tissue Engineering: Development of bioengineered grafts has shown promise in reducing complications and improving functional outcomes.
- Genetic Research: Understanding the genetic factors contributing to hypospadias can help in early diagnosis and potentially in the development of preventive strategies.
- Minimally Invasive Techniques: Advancements in laparoscopic and robotic-assisted surgeries are being explored to reduce recovery times and enhance precision in complex cases.
By integrating these research findings into clinical practice, surgeons can offer more effective and less invasive treatment options, ultimately improving the quality of life for patients with hypospadias.
FAQs about Hypospadias Treatment
What is Hypospadias?
Hypospadias is a congenital condition where the opening of the urethra is located on the underside of the penis instead of at the tip. This can affect urination and, in some cases, sexual function.
How is Hypospadias Diagnosed?
Hypospadias is typically diagnosed at birth during a physical examination. In some cases, further tests such as ultrasounds may be required to assess the condition’s severity and associated abnormalities.
What are the Treatment Options for Hypospadias?
The primary treatment for hypospadias is surgical correction. This surgery, usually performed between 6 to 18 months of age, aims to reposition the urethral opening and straighten the penis if necessary. The specific surgical techniques can vary depending on the severity of the condition.
Is Surgery Always Necessary?
In most cases, surgery is recommended to correct hypospadias and prevent future complications. However, for mild cases where the urethral opening is only slightly mislocated, surgery may not be immediately necessary.
What is the Recovery Process Like?
Post-surgery, children typically recover quickly. They may need to avoid strenuous activities for a few weeks and follow specific care instructions provided by their surgeon. Follow-up appointments are crucial to monitor healing and ensure successful results.
Are There Any Risks or Complications?
As with any surgery, there are potential risks, including infection, bleeding, or complications with the repair. However, hypospadias surgery is generally safe and successful, especially when performed by an experienced pediatric urologist.
Can Hypospadias Affect Fertility?
Most individuals who undergo successful hypospadias repair can expect normal fertility. However, severe cases of hypospadias, especially if left untreated, could potentially impact reproductive function.
Where Can I Find More Information?
For more detailed information, consulting a pediatric urologist or referring to reputable medical websites like the American Urological Association can be very helpful.
Conclusion
Recognizing and treating hypospadias is crucial for ensuring the health and well-being of affected individuals. Early diagnosis and proper management can prevent complications and improve quality of life.
Consulting with specialists is essential, as they provide expert guidance and personalized treatment plans. The future of hypospadias treatment is promising, with advancements in surgical techniques and ongoing research aimed at improving outcomes.
By staying informed and seeking professional advice, patients and caregivers can make informed decisions and contribute to better health outcomes.
References
For further reading and validation of the information provided in this article on Hypospadias Treatment, we recommend the following reputable sources:
- Mayo Clinic – Hypospadias: Diagnosis and Treatment
- Cleveland Clinic – Hypospadias
- American Urological Association – Hypospadias Guidelines
These references provide comprehensive information and further details about the diagnosis, treatment options, and management of hypospadias.