Hypoplastic Left Heart Syndrome Symptoms: Hypoplastic Left Heart Syndrome (HLHS) is a rare, yet severe congenital heart defect that impacts normal blood flow through the heart.
Understanding the symptoms and causes of HLHS is crucial for early detection and effective management of this condition.
This article delves into the intricate details of HLHS, shedding light on its symptoms and underlying causes.
What is Hypoplastic Left Heart Syndrome (HLHS)?
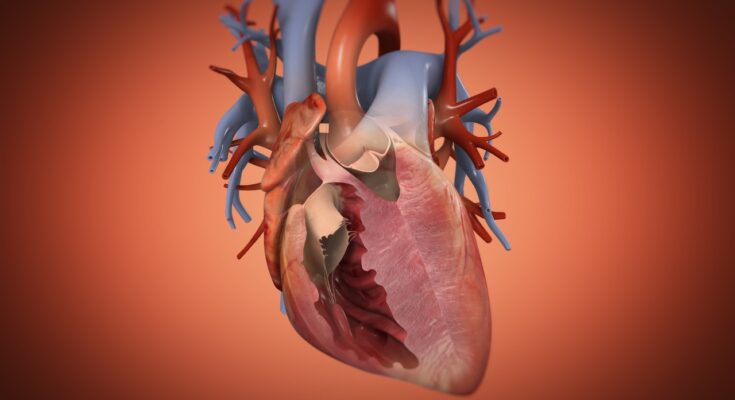
Hypoplastic Left Heart Syndrome (HLHS) is a rare and complex congenital heart defect present at birth. This condition involves underdevelopment of the left side of the heart, which includes the left ventricle, mitral valve, aortic valve, and the ascending portion of the aorta. As a result, the left side of the heart is unable to effectively pump blood to the body, forcing the right side of the heart to compensate by pumping blood both to the lungs and the rest of the body. This additional strain can lead to heart failure and other serious health issues.
How HLHS Affects the Heart’s Structure
HLHS leads to several structural changes in the heart, including:
- Underdeveloped Left Ventricle: The left ventricle is significantly smaller and weaker than normal, severely limiting its ability to pump blood.
- Stenotic or Atretic Mitral and Aortic Valves: These valves, which control blood flow from the left atrium to the left ventricle and from the left ventricle to the aorta, are either abnormally narrow, not fully formed, or completely closed.
- Small Ascending Aorta: The ascending aorta, which normally carries oxygen-rich blood from the left ventricle to the body, is smaller in diameter, reducing blood flow to the body’s vital organs.
Statistics on Prevalence and Diagnosis Rates
HLHS is a rare condition, affecting approximately 1 in every 4,000 newborns worldwide. This heart defect is typically diagnosed during a prenatal ultrasound or shortly after birth through clinical symptoms and echocardiography. Early diagnosis and intervention are crucial as HLHS is a life-threatening condition without surgical intervention. Despite its severity, advancements in surgical techniques and postoperative care have significantly improved the survival rate and quality of life for children born with this condition. In recent decades, the survival rate into adolescence and adulthood has increased substantially, though ongoing medical care and potential additional surgeries are often necessary.
Symptoms of Hypoplastic Left Heart Syndrome
Recognizing the symptoms early can significantly impact the management and outcomes of this condition. Here’s a detailed look at the symptoms across different stages of early life.
Early Signs in Newborns and Infants
In newborns and infants, the symptoms of HLHS are often noticeable shortly after birth. These signs include:
- Cyanosis: A blue tint to the skin, lips, and nails, indicating low oxygen levels in the blood.
- Difficulty Breathing: Rapid, labored, or heavy breathing is common as the heart struggles to supply oxygen-rich blood to the body.
- Poor Feeding: Infants with HLHS may have difficulty feeding and may tire very quickly during feeds.
- Lethargy: Newborns may show unusually low energy levels or seem excessively sleepy.
- Weak Pulse and Cold Extremities: The baby’s pulse may feel weak, and their hands and feet may be cool to the touch due to poor blood circulation.
Symptoms That Develop in Early Childhood
If HLHS is not diagnosed in infancy, symptoms may evolve as the child grows. These include:
- Failure to Thrive: Affected children may not gain weight or grow at a normal rate due to the heart’s inefficiency in nutrient and oxygen distribution.
- Developmental Delays: Delays in reaching milestones such as sitting up, walking, or talking may occur.
- Decreased Physical Stamina: Children might tire more easily during physical activity and may not be able to keep up with their peers.
How Symptoms May Progress Without Treatment
Without proper treatment, HLHS can lead to progressively severe complications. The ongoing strain on the heart can lead to:
- Heart Failure: The underdeveloped heart may not function properly, leading to heart failure.
- Arrhythmias: Irregular heartbeats can develop, further complicating the child’s condition.
- Edema: Fluid buildup in various parts of the body, such as the lungs and limbs, may occur due to poor heart function.
- Pulmonary Hypertension: Increased blood pressure in the lungs can arise from the heart’s inability to effectively pump blood.
If any of these symptoms are noticed, it is essential to consult a pediatric cardiologist immediately. Early intervention can lead to better management strategies and improved outcomes for children suffering from HLHS.
Causes and Risk Factors of Hypoplastic Left Heart Syndrome
Understanding the causes and risk factors is crucial for early diagnosis and management. This condition is influenced by genetic, environmental, and familial factors.
Genetic Factors Associated with HLHS
Genetic influences play a significant role in the development of HLHS. Several genetic abnormalities have been linked to the syndrome:
- Chromosomal Anomalies: Conditions such as Turner syndrome (45,X0) and other chromosomal disorders are sometimes associated with HLHS.
- Gene Mutations: Specific gene mutations can predispose an individual to HLHS. Researchers have identified mutations in genes like NKX2-5, GJA1, and MYH6 as potential contributors.
- Genetic Syndromes: HLHS can occur as part of broader genetic syndromes that affect multiple organs and systems, further complicating the condition.
Possible Environmental Contributors
While the exact environmental causes of HLHS remain under investigation, several factors are believed to contribute to its development:
- Maternal Health: Conditions during pregnancy, such as diabetes or a viral infection, can increase the risk of giving birth to a child with HLHS.
- Medication Exposure: Exposure to certain medications during pregnancy, like some anti-seizure drugs or prostaglandin synthesis inhibitors, has been linked to a higher risk of congenital heart defects, including HLHS.
- Lifestyle Factors: Maternal lifestyle factors such as smoking or severe nutritional deficiencies during pregnancy might also elevate the risk.
The Role of Family History in HLHS
Family history is a significant risk factor in the occurrence of HLHS:
- Genetic Predisposition: Families with a history of congenital heart defects, especially HLHS, are at increased risk of recurrence in subsequent generations.
- Sibling Risk: If a family already has one child with HLHS, the risk of having another child with the same condition is increased, though the exact percentage varies.
However, understanding these risk factors helps in assessing the likelihood of HLHS and can guide genetic counseling and prenatal care to manage and mitigate risks associated with the condition.
Diagnosis of Hypoplastic Left Heart Syndrome
Detecting Hypoplastic Left Heart Syndrome (HLHS) early in newborns is crucial for managing this serious condition. Below, we explore the primary methods for diagnosing HLHS, emphasizing the importance of prenatal and postnatal screenings and follow-up procedures.
Screening Methods for HLHS in Newborns
Early detection of HLHS significantly improves the management and outcomes of the condition. The screening process for HLHS involves several non-invasive tests that can identify the condition shortly after birth:
- Pulse Oximetry Screening:
Pulse oximetry is a simple, painless test that measures the oxygen saturation level in a baby’s blood. It involves placing a sensor on a baby’s skin, typically on the foot or hand. Low oxygen levels can indicate a heart problem or other conditions, prompting further investigation. - Echocardiogram Details:
An echocardiogram is critical for diagnosing HLHS and assessing its severity. This ultrasound of the heart provides detailed images of the heart’s structure and function, helping doctors see the underdeveloped left side of the heart characteristic of HLHS. It also evaluates how well the right side of the heart is functioning and checks for other complications.
Importance of Prenatal Ultrasound in Identifying HLHS
Prenatal ultrasounds play a pivotal role in the early diagnosis of HLHS. During routine pregnancy check-ups, an ultrasound can detect structural abnormalities in the fetus’s heart as early as the second trimester. Early detection allows expectant parents to plan with healthcare providers for necessary interventions and care immediately after birth.
Stages of Diagnosis and Follow-ups
The diagnosis of HLHS occurs in stages, starting from prenatal ultrasounds, followed by postnatal pulse oximetry, and confirmed through an echocardiogram. After the initial diagnosis:
- Immediate Postnatal Care: Newborns diagnosed with HLHS typically receive care in a neonatal intensive care unit (NICU), where they are closely monitored and stabilized.
- Follow-Up Assessments: Regular follow-up appointments are essential. These include frequent echocardiograms to monitor the heart’s function and development, as well as other assessments to manage the overall health and wellbeing of the child.
- Long-Term Care Planning: As children with HLHS grow, their condition requires ongoing assessment and management. This involves a team of pediatric cardiologists, cardiac surgeons, and specialized nurses dedicated to providing continuous care tailored to each child’s needs.
However, through early and accurate diagnosis, appropriate treatments can be planned and administered, significantly improving the quality of life and outcomes for affected children.
Management and Treatment Options for Hypoplastic Left Heart Syndrome (HLHS)
Managing and treating HLHS requires a combination of intricate surgical interventions and ongoing non-surgical care. Here, we will explore the stages and goals of these treatments to provide a comprehensive understanding for families and caregivers.
Surgical Interventions: Stages and Goals
1. Norwood Procedure: Typically performed within the first few weeks of life, the Norwood procedure is the initial surgery for children with HLHS. The goal of this operation is to reconstruct the heart so that the right ventricle can effectively pump blood to both the lungs and the rest of the body. This involves building a new aorta and connecting it directly to the right ventricle.
2. Glenn Procedure: Performed when the child is between 4 and 6 months old, the Glenn procedure is the second stage of surgical treatment. This surgery reduces the workload on the right ventricle by redirecting the oxygen-poor blood from the upper body directly to the lungs, bypassing the heart. This is achieved by connecting the superior vena cava to the pulmonary artery.
3. Fontan Procedure: The final stage in the surgical management of HLHS, the Fontan procedure is usually carried out between 2 and 4 years of age. It completes the separation of oxygen-rich and oxygen-poor blood. The procedure involves directing blood from the lower body to the lungs by connecting the inferior vena cava to the pulmonary artery. This allows the right ventricle to pump oxygen-rich blood more efficiently to the body.
Non-surgical Treatments
Medications: Several medications may be used to help the heart work more efficiently and to improve blood flow. Common medications include diuretics, which help reduce fluid accumulation in the body, and inotropes, which strengthen the heart’s pumping capacity.
Lifestyle Adjustments for Children with HLHS: While lifestyle adjustments cannot cure HLHS, they can significantly improve quality of life. Nutritional support is crucial, as children with HLHS often have difficulty gaining weight. Activities may need to be moderated to balance energy expenditure and heart function. Emotional and psychological support is also vital for the child and family.
Role of Ongoing Medical Care and Monitoring
Regular follow-ups with a pediatric cardiologist are essential. These appointments allow doctors to monitor the heart’s function, assess the effectiveness of treatments, and make adjustments as necessary. Advanced imaging techniques, such as echocardiograms and MRIs, play a critical role in ongoing care. Additionally, vaccinations and routine health check-ups are vital to prevent complications such as infections.
However, effective management of Hypoplastic Left Heart Syndrome involves a coordinated approach that includes sophisticated surgeries and comprehensive non-surgical care. Through these interventions and careful monitoring, children with HLHS can lead more stable and healthier lives.
Living with Hypoplastic Left Heart Syndrome (HLHS)
Living with Hypoplastic Left Heart Syndrome (HLHS) presents unique challenges for both patients and their families. Understanding these challenges and knowing where to find resources and support can significantly ease the journey.
Challenges for Families and Patients
- Medical Complexity: HLHS is a complex congenital heart defect where the left side of the heart is underdeveloped. It requires multiple surgeries and ongoing medical care, which can be overwhelming for families.
- Emotional Stress: The diagnosis of HLHS brings a significant emotional toll on families. Parents may experience stress, anxiety, and depression as they navigate their child’s health issues and the uncertainties of the future.
- Financial Burden: The cost of surgeries, hospital stays, medications, and follow-up care can be substantial. Families often face financial strain and may need to seek financial assistance or adjust their work lives to manage care.
- Social Impact: Families may also experience social isolation as their lifestyle becomes centered around their child’s medical needs. This can affect relationships and reduce opportunities for normal family activities.
- Educational and Developmental Challenges: Children with HLHS may face developmental delays and educational challenges. Families need to advocate for their child’s educational needs and seek appropriate support services.
Resources and Support for Coping with HLHS
- Specialized Medical Care: It’s crucial to have a healthcare team that specializes in congenital heart defects. Major children’s hospitals often have dedicated cardiac units that provide tailored care for HLHS patients.
- Support Groups: Connecting with other families who are dealing with HLHS can provide emotional support and valuable insights. Organizations such as the Children’s Heart Foundation and Mended Little Hearts offer support groups and resources.
- Financial Assistance Programs: Many organizations and charities provide financial aid specifically for families dealing with significant medical expenses. The National Organization for Rare Disorders (NORD) offers a financial assistance program for medical treatments.
- Educational and Developmental Support: Early intervention programs can be critical. These programs offer therapies that help children develop motor skills, cognitive skills, and other abilities. Schools and educational systems may also provide special accommodations and support.
- Mental Health Resources: Access to mental health professionals who specialize in chronic illness can help families and patients cope with emotional stress. Counseling and therapy can be vital in managing the psychological aspects of living with a chronic condition.
By understanding the challenges and accessing the available resources and support systems, families dealing with HLHS can find the necessary help to manage this condition effectively. This knowledge not only helps in providing the best care for the child but also supports the overall well-being of the entire family.
FAQs about Hypoplastic Left Heart Syndrome Symptoms
What is Hypoplastic Left Heart Syndrome (HLHS)?
Hypoplastic Left Heart Syndrome (HLHS) is a severe congenital heart defect in which the left side of the heart is underdeveloped. This condition affects the heart’s ability to pump blood effectively to the body, necessitating specialized care and treatment.
What are the first signs of HLHS in newborns?
The first signs of HLHS in newborns typically appear within the first few hours or days of life. These can include rapid breathing, difficulty feeding, lethargy, and a blue tint to the skin, lips, and nail beds, known as cyanosis. These symptoms result from insufficient oxygenated blood reaching the body.
How is HLHS detected?
HLHS is often detected during a prenatal ultrasound, but if not, symptoms soon after birth will lead to further cardiac evaluation. This includes echocardiograms (heart ultrasounds) and other diagnostic tests to assess the structure and function of the heart.
Can a baby with HLHS appear healthy at birth?
Yes, some babies with HLHS might initially appear healthy at birth and develop symptoms within the first few days of life as the ductus arteriosus (a fetal blood vessel) begins to close, which is a normal process after birth that can exacerbate the condition in HLHS.
What symptoms might older children with HLHS experience?
Older children with HLHS who have undergone initial surgeries may experience varied symptoms based on their individual condition and surgeries. These can include decreased exercise tolerance, difficulty breathing, fatigue, and signs of heart failure or complications related to their heart condition.
Is there a cure for HLHS?
While there is no cure for HLHS, several surgical procedures performed in stages can help create a functional circulation that compensates for the underdeveloped left heart. The treatment involves a series of surgeries—typically three—carried out over the first few years of life.
What should parents watch for in children with HLHS?
Parents should monitor for any signs of decreased energy, difficulty breathing, decreased appetite, or any other changes that might indicate heart failure or complications. Regular follow-ups with a pediatric cardiologist are essential for managing and monitoring the child’s condition.
Conclusion
Understanding the symptoms of Hypoplastic Left Heart Syndrome (HLHS) is crucial for early diagnosis and intervention, which can significantly improve outcomes for affected infants.
Recent advances in medical treatments and surgical techniques have dramatically enhanced the prognosis for HLHS, offering hope to families and extending the lives of those affected.
If you suspect that your child may be showing signs of HLHS, or if you have any concerns about their heart health, it is vital to consult with healthcare providers promptly. These professionals can provide the necessary screenings and evaluations to ensure that any heart issues are properly addressed.
Early medical engagement is key to leveraging the advancements in HLHS treatment and ensuring the best possible outcomes for your child.
References
For those seeking more detailed information and further reading on Hypoplastic Left Heart Syndrome (HLHS), including its symptoms and management, the following resources are highly recommended. Each source has been chosen for its reliability and depth of information to ensure readers have access to credible and comprehensive data:
- American Heart Association (AHA) – Provides a thorough overview of Hypoplastic Left Heart Syndrome, including symptoms, treatment options, and long-term outlook. Explore their detailed guide here.
- Mayo Clinic – Offers an expert-written, in-depth description of HLHS, symptoms to watch for, and the various stages of treatment. Visit their page on the condition here.
- National Organization for Rare Disorders (NORD) – Provides a comprehensive article on Hypoplastic Left Heart Syndrome, including detailed sections on symptoms, diagnosis, and therapeutic strategies. Read more at NORD’s website.
These sources are excellent starting points for understanding HLHS, and they offer resources for both patients and healthcare providers.