Hypoplastic Left Heart Syndrome Treatment: Hypoplastic Left Heart Syndrome (HLHS) represents a significant challenge in pediatric cardiology, characterized by underdevelopment of the left side of the heart.
This condition affects various structures of the left heart including the mitral valve, left ventricle, aortic valve, and aorta.
Understanding the diagnosis and treatment options is crucial for managing this severe congenital defect effectively.
What is Hypoplastic Left Heart Syndrome?
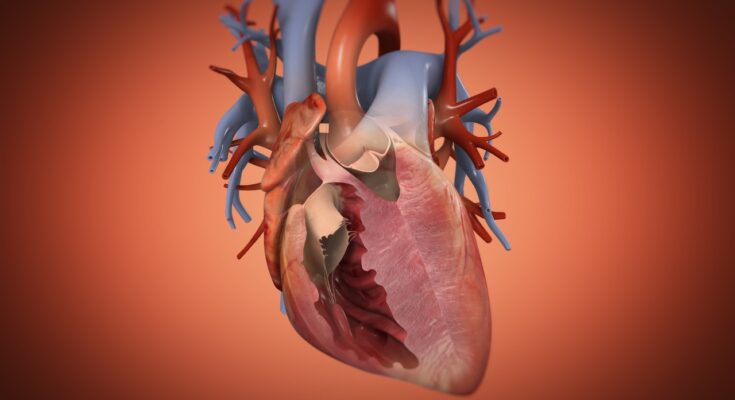
Hypoplastic Left Heart Syndrome (HLHS) is a rare congenital heart defect characterized by the underdevelopment of the left side of the heart. This includes the left ventricle, mitral valve, aortic valve, and parts of the aorta. The condition is critical and requires immediate intervention after birth. HLHS affects normal blood flow through the heart, as the structures on the left side are too small to function effectively, forcing the right side of the heart to compensate by pumping blood to both the lungs and the rest of the body.
Pathophysiology of HLHS
The pathophysiology of HLHS involves several key abnormalities:
- Underdeveloped Left Ventricle: The left ventricle is significantly smaller and less muscular, unable to pump oxygen-rich blood to the body efficiently.
- Mitral Valve Atresia or Stenosis: The mitral valve, which controls blood flow between the left atrium and left ventricle, is often closed or very narrow, further restricting blood flow.
- Aortic Valve Atresia or Stenosis: Similar to the mitral valve, the aortic valve is also critically narrowed or closed, preventing blood from flowing from the left ventricle to the aorta.
- Hypoplastic Aorta: The ascending aorta is underdeveloped, which limits blood flow to the body, compounding the challenges of oxygen delivery to the tissues.
Epidemiology and Risk Factors Associated with HLHS
Hypoplastic Left Heart Syndrome is considered one of the more severe heart defects and occurs in approximately 1 out of every 4,000 live births. The exact causes of HLHS are not fully understood, but several risk factors have been identified:
- Genetic Factors: A family history of congenital heart defects can increase the risk of HLHS.
- Environmental Exposures: Certain conditions during pregnancy, including the mother’s exposure to some medications, illnesses, or environmental toxins, may contribute to the development of HLHS.
- Maternal Health: Issues such as diabetes in the mother can also heighten the risk.
- Gender: HLHS is slightly more common in males than in females.
However, understanding these factors can help in managing and preventing potential cases of HLHS and guiding research into further treatment options.
Symptoms and Early Signs of Hypoplastic Left Heart Syndrome
Understanding the early signs and symptoms of HLHS is crucial for early intervention and improved outcomes. Here we discuss the common symptoms in newborns and infants, and emphasize the importance of detecting these symptoms early.
Common Symptoms in Newborns and Infants
- Cyanosis: A bluish tint to the skin, lips, and fingernails, known as cyanosis, is one of the most noticeable early signs of HLHS. This occurs because oxygenated blood does not circulate effectively through the body due to the underdeveloped heart.
- Rapid Breathing or Difficulty Breathing: Infants with HLHS may exhibit rapid breathing or struggle to breathe due to the heart’s inability to deliver adequate oxygen to the body.
- Poor Feeding: Difficulty feeding or a lack of appetite is common among newborns with HLHS. This may be accompanied by fatigue during feeding, as the baby may tire easily due to low oxygen levels.
- Lethargy: Newborns with this condition often appear unusually sleepy or lethargic. They may show less interest in their surroundings due to decreased energy levels.
- Cold Extremities: The hands and feet may feel cool to the touch, indicating that blood circulation is compromised.
- Weak Pulse or Heart Murmurs: A weak pulse in the groin, wrist, or another area can be a sign of HLHS. Additionally, a heart murmur, often described as an extra or unusual sound during the heartbeat, is typically detected by a healthcare provider during a physical examination.
The Critical Nature of Early Symptom Detection
Early detection of these symptoms is vital. HLHS can lead to serious complications, such as heart failure or life-threatening infections, if not treated promptly. Newborns showing signs of heart distress should undergo detailed cardiac evaluation to confirm the diagnosis and begin the necessary interventions.
Early diagnosis typically involves echocardiography, a safe and effective imaging technique that allows doctors to view the heart’s structure and function in detail. With timely and appropriate treatment, which may include medications, surgery, or in some cases, heart transplantation, children with HLHS can lead longer and more quality-filled lives.
Parents and caregivers should seek immediate medical attention if they notice any of the above symptoms in their newborns. Early intervention is key to managing HLHS effectively, and regular follow-ups with a pediatric cardiologist are crucial to monitor the child’s health and heart function.
By recognizing the early signs of Hypoplastic Left Heart Syndrome, parents and healthcare providers can act swiftly to ensure that infants receive the care they need, potentially saving lives and enhancing the quality of life for those affected.
Diagnostic Procedures for Hypoplastic Left Heart Syndrome
Early diagnosis is crucial for the management and treatment of HLHS. Here we explore the various diagnostic procedures and the importance of prenatal screening for this condition.
List of Diagnostic Imaging and Tests
- Fetal Echocardiography: This is the most effective test for detecting HLHS and other congenital heart defects before birth. It uses ultrasound waves to create images of the baby’s heart, typically performed between 18 to 22 weeks of gestation.
- Echocardiogram: After birth, an echocardiogram can assess the structure and function of the heart. This test is essential for confirming the diagnosis of HLHS by detailing the heart’s size, structure, and blood flow.
- Electrocardiogram (ECG): This test records the electrical activity of the heart and helps in identifying any rhythm abnormalities, which are common in children with HLHS.
- Chest X-ray: This imaging test can show the size and shape of the heart and whether there is an enlargement of organs or abnormal fluid accumulation.
- Cardiac MRI: A cardiac MRI provides detailed images of the heart’s structures and can be used to plan surgeries or assess ongoing heart function.
- Cardiac Catheterization: Although not always necessary, this invasive test can measure the pressure and oxygen levels in different parts of the heart and can be used to assess the need for intervention or surgery.
Role of Prenatal Screening in Early Detection
Prenatal screening plays a vital role in the early detection of HLHS. Early diagnosis via fetal echocardiography allows for optimal planning and management, improving the overall prognosis. With prenatal screening, parents can be prepared for the necessary interventions and surgeries immediately after birth. Furthermore, it provides an opportunity for healthcare providers to plan the delivery around facilities equipped to handle the complexities of HLHS, ensuring immediate and specialized care.
Prenatal screening not only helps in early detection but also assists in making informed decisions about the pregnancy and the care plan post-birth. Regular follow-up and monitoring through prenatal visits enhance the ability to assess and adjust care for the fetus and mother as needed.
However, timely and accurate diagnostic imaging and tests are essential for the detection and management of Hypoplastic Left Heart Syndrome. Coupled with comprehensive prenatal screening, these procedures can significantly influence the outcomes for infants affected by this challenging condition.
Treatment Options for Hypoplastic Left Heart Syndrome
Managing HLHS effectively requires a combination of immediate stabilization procedures and a series of surgeries spread over several years. Below, we detail the treatment protocol, focusing on both surgical and non-surgical interventions.
Initial Management and Stabilization of Infants with HLHS
Immediate postnatal management of infants diagnosed with HLHS is crucial to ensure the baby’s survival and stability before any surgical procedure. Initial stabilization typically involves:
- Prostaglandin E1 Therapy: This medication is used to keep the ductus arteriosus open, ensuring blood flow bypasses the underdeveloped left heart and continues to the aorta.
- Mechanical Ventilation: Supports breathing and oxygenation, which is vital due to the compromised heart function.
- Inotropic Support: Medications that help strengthen the heart’s pumping capability may be administered to support cardiac output.
Detailed Exploration of Surgical Treatment Stages
The surgical treatment for HLHS involves three stages performed at different times in the infant’s early life, each designed to reconstruct the heart’s functionality progressively.
Stage I: Norwood Procedure
Performed shortly after birth, the Norwood Procedure is the first critical surgery. It involves:
- Reconstruction of the Aorta and Right Ventricle: The main pulmonary artery and the aorta are connected, and the right ventricle is reconstructed to pump blood to both the lungs and the body.
- Placement of a Shunt: A shunt is placed between the pulmonary artery and the aorta to assist pulmonary blood flow, which is crucial until the second stage of surgery.
Stage II: Glenn Procedure
At around 4 to 6 months of age, the Glenn Procedure is the second stage. This surgery involves:
- Connecting the Superior Vena Cava to the Pulmonary Arteries: This procedure reduces the workload on the right ventricle by allowing blood from the upper body to flow directly into the lungs, bypassing the heart.
Stage III: Fontan Procedure
The final stage, usually performed between 2 and 4 years of age, is the Fontan Procedure. It involves:
- Directing Blood from the Lower Body to the Lungs: This is achieved by connecting the inferior vena cava to the pulmonary arteries, completing the separation of oxygen-rich and oxygen-poor blood.
Non-Surgical Interventions
In addition to surgical treatments, non-surgical interventions may include:
- Heart Transplantation: In some cases, a heart transplant may be considered if the staged surgeries are not viable or if the heart function deteriorates significantly.
- Medications: Continuous medication may be required to help control heart rhythm, prevent blood clots, and improve heart function.
However, with the advancements in medical science and surgical techniques, the outlook for infants with HLHS has significantly improved, offering them a better chance at a prolonged and improved quality of life.
Advances in Hypoplastic Left Heart Syndrome Treatment
Advances in treatment techniques and ongoing research are crucial in improving outcomes for patients with HLHS. This section will explore the latest research and developments in surgical techniques, as well as potential future treatments and ongoing clinical trials.
Latest Research and Developments in Surgical Techniques
Recent advancements in the surgical management of HLHS have significantly improved survival rates and quality of life for affected infants. Key developments include:
- Hybrid Procedures: Combining surgical and catheter-based techniques, hybrid procedures allow for less invasive interventions that can be crucial in the initial stabilization of newborns with HLHS.
- The Norwood Procedure Enhancements: Innovations in the Norwood procedure, the first of three surgeries typically performed in stages, have led to better outcomes. These enhancements include refined surgical techniques and improved post-operative care protocols.
- Regenerative Medicine Applications: Researchers are exploring the use of stem cells to regenerate heart tissue, potentially improving heart function in children who have undergone surgeries for HLHS.
- 3D Printing Technology: Surgeons use 3D printing to create exact replicas of a patient’s heart. This technology aids in planning and practicing complex surgeries, leading to more precise interventions.
Potential Future Treatments and Ongoing Clinical Trials
The future of HLHS treatment is promising, with several innovative approaches being investigated:
- Genetic Therapies: As researchers better understand the genetic factors contributing to HLHS, gene therapy emerges as a potential treatment to correct underlying genetic defects before birth.
- Biodegradable Heart Conduits: Development of biodegradable grafts that grow with the patient and reduce the need for multiple surgeries is an exciting area of research.
- Clinical Trials: Ongoing clinical trials are testing the efficacy of using a patient’s own stem cells to repair heart tissues, which could revolutionize treatment paradigms in congenital heart diseases. The Pediatric Heart Network, among others, regularly updates lists of active clinical trials focused on HLHS.
However, these advances represent a combination of surgical innovation, genetic research, and regenerative medicine, highlighting a hopeful trajectory towards more effective treatments for Hypoplastic Left Heart Syndrome. As these technologies and methods continue to evolve, they hold the potential to significantly improve the lives of patients with HLHS.
Challenges in Managing Hypoplastic Left Heart Syndrome (HLHS)
Managing Hypoplastic Left Heart Syndrome (HLHS), a severe congenital heart defect where the left side of the heart is underdeveloped, presents significant challenges for healthcare providers, patients, and their families. The complexity of HLHS requires a multidisciplinary approach to care, spanning various stages from diagnosis through to adulthood.
Long-Term Management Complexities
The long-term management of HLHS involves multiple surgeries and medical interventions, starting from the first few days of a newborn’s life. These surgeries are critical and are typically performed in stages to reconstruct the heart and improve its function. However, each stage carries risks and can lead to complications such as heart failure, arrhythmias, and organ dysfunction. Beyond surgical intervention, patients often require lifelong cardiac care, including medications to support heart function and regular follow-up appointments with cardiac specialists.
Patients with HLHS are also at a higher risk for developmental delays and neurological issues, necessitating ongoing therapy and support. This comprehensive care approach highlights the complexity of treating HLHS and underscores the importance of specialized healthcare teams.
Impact on Quality of Life
HLHS significantly impacts the quality of life not only for the patient but also for their family. For patients, the physical limitations and frequent medical visits can lead to social isolation and emotional distress. The psychological burden of living with a chronic, life-threatening condition can affect a patient’s mental health, leading to anxiety or depression.
For families, the diagnosis of HLHS in a child brings about profound emotional, financial, and social challenges. The need for ongoing care and the possibility of medical emergencies can cause significant stress and uncertainty. Families often face financial strain due to medical costs and the need for a parent to reduce work hours or even stop working to care for the child.
Supporting the patient and family, enhancing communication among care providers, and providing access to resources such as counseling and support groups are crucial for improving the overall quality of life for those affected by HLHS.
However, addressing these challenges effectively improves not only the survival and health of the patient but also enhances the quality of life for both the patient and their family. With advances in medical treatments and supportive care, the outlook for patients with HLHS continues to improve, bringing hope to those affected by this challenging condition.
Support and Resources for Families Dealing with Hypoplastic Left Heart Syndrome (HLHS)
Families facing the challenges of Hypoplastic Left Heart Syndrome (HLHS) in a loved one often find that accessing robust support and resources is crucial for managing the emotional, physical, and financial stresses associated with this serious condition. HLHS is a rare congenital heart defect where the left side of the heart is underdeveloped, requiring specialized care and often multiple surgeries starting in infancy.
Importance of Support Systems and Resources
Having a strong support system is essential for families navigating the complexities of HLHS. Support systems can include healthcare professionals, counseling services, and community groups. These networks provide not only emotional reassurance and a sense of community but also practical advice and firsthand experiences from other families facing similar challenges. They can significantly improve the quality of life and outcomes for the child and family members by reducing feelings of isolation and providing essential information and coping strategies.
Organizations and Communities Focused on Congenital Heart Defects
Several organizations and communities offer support, education, and advocacy for families affected by congenital heart defects like HLHS. Here are some prominent ones:
- The Children’s Heart Foundation – This organization is dedicated to funding research and providing information to improve the lives of those with congenital heart defects. They offer resources for families, connect them with research updates, and provide community support networks.
- Mended Little Hearts – An initiative that provides resources, communities, and hope for children with congenital heart defects and their families. They offer a national network of support groups, educational resources, and advocacy opportunities.
- Adult Congenital Heart Association (ACHA) – While primarily focused on adults, ACHA also offers valuable resources for families transitioning pediatric patients into adult care. Their services include patient education, advocacy, and connection to specialized care.
- Little Hearts, Inc. – A nonprofit organization that offers support, education, and advocacy for families affected by congenital heart defects. They provide a supportive community and practical resources to help families navigate their journey.
These organizations provide critical resources ranging from emotional support groups to practical advice on handling medical procedures and financial assistance. Engaging with these communities can provide families with the necessary tools to face the challenges of HLHS with resilience and informed confidence.
By utilizing these resources, families can find much-needed support and information to help manage the journey through HLHS treatment and care. It’s important for family members to reach out and connect with these communities to not only receive support but also to enhance the collective knowledge and advocacy for congenital heart defects.
FAQs about Hypoplastic Left Heart Syndrome Treatment
What is Hypoplastic Left Heart Syndrome?
Hypoplastic Left Heart Syndrome (HLHS) is a congenital heart defect where the left side of the heart is underdeveloped. It affects several structures on the left side of the heart that are crucial for normal blood flow.
How is HLHS treated?
Treatment for HLHS typically involves multiple surgeries performed in stages. The first stage, often done within the first few weeks of life, is called the Norwood procedure. Subsequent surgeries — the Glenn procedure and the Fontan procedure — follow at several months and a few years of age, respectively.
Can HLHS be cured?
While HLHS can be managed with surgery, it is not considered curable. Treatments focus on improving heart function and quality of life.
What are the long-term prospects for a child with HLHS?
With advances in medical treatment and surgery, children with HLHS are living longer and healthier lives than in the past. Long-term outcomes vary, with ongoing medical follow-up required to address any complications or additional health issues.
Is there support available for families affected by HLHS?
Yes, many hospitals offer resources for families, including counseling and support groups. National organizations and online communities also provide valuable support and information for families dealing with HLHS.
Conclusion
In summary, the diagnosis and treatment of Hypoplastic Left Heart Syndrome (HLHS) remain pivotal in enhancing the survival and quality of life for affected infants. Recent advancements in medical procedures and technologies have shown promising results, yet the complexity of HLHS calls for ongoing innovation and improvement in treatment methodologies.
It is crucial that research in this area continues to receive support. Funding for new studies, development of advanced medical technologies, and improved surgical techniques are essential for forging pathways towards better outcomes. The role of community support cannot be overstated; it provides not only emotional and social backing for families but also helps in advocating for essential research and healthcare services.
Together, through sustained research efforts and community engagement, we can hope to see further improvements in the management and prognosis of Hypoplastic Left Heart Syndrome, offering a brighter future for those affected by this challenging condition.
References
For those seeking more in-depth information or verification of the details discussed regarding the treatment of Hypoplastic Left Heart Syndrome (HLHS), the following sources are highly recommended. These references are from reputable medical journals and organizations, ensuring reliable and up-to-date information:
- American Heart Association (AHA) – Provides comprehensive guidelines and articles on the management and treatment options available for HLHS. Visit their official website for detailed resources: American Heart Association – HLHS.
- Mayo Clinic – Offers a detailed overview of Hypoplastic Left Heart Syndrome, including symptoms, diagnosis, treatment plans, and long-term outlook. Access their extensive articles at Mayo Clinic – HLHS.
- National Organization for Rare Disorders (NORD) – Contains valuable data on rare diseases, including HLHS, with resources for treatment and patient support. For more information, check out NORD – HLHS.
- PubMed Central – An invaluable resource for accessing scientific studies and clinical trial outcomes regarding HLHS treatments. Browse related articles at PubMed Central.
- Children’s Heart Foundation – Focuses on research and education specific to congenital heart defects like HLHS. They provide resources for families and practitioners alike. Learn more by visiting Children’s Heart Foundation.
These sources are essential for anyone looking to understand the complex nature of HLHS and the advancements in its treatment. They provide a solid foundation for academic study or personal knowledge, ensuring that the information you obtain is accurate and trustworthy.