Hypertrophic Cardiomyopathy Symptoms: Hypertrophic Cardiomyopathy (HCM) is a condition characterized by the thickening of the heart muscle, which can lead to various health challenges.
This cardiac disorder is often inherited and is commonly undiagnosed because symptoms can be sporadic or non-existent.
Understanding both the symptoms and causes of HCM is crucial for early detection and management, potentially saving lives and improving the quality of life for those affected.
Understanding Hypertrophic Cardiomyopathy (HCM)
Hypertrophic cardiomyopathy (HCM) is a complex heart condition characterized by the thickening of the heart muscle, which can impede normal blood flow and lead to various cardiac issues. This section delves into the epidemiology of HCM and touches on its genetic basis, providing a clear and comprehensive overview.
Epidemiology: How Common is HCM?
Hypertrophic cardiomyopathy is relatively common in the general population, affecting approximately 1 in 500 people. It is one of the most frequent hereditary cardiac disorders and the most common cause of sudden cardiac death in young athletes. The prevalence of HCM is consistent across various ethnicities and demographics, making it a significant concern for a broad spectrum of individuals.
Genetic Nature of the Disease
HCM is primarily genetic in origin, caused by mutations in one or more genes responsible for the structure of the heart muscle. These mutations lead to the abnormal thickening of the myocardium—the heart’s muscular wall. The disease often runs in families, and individuals with a family history of HCM have a higher risk of developing the condition. Genetic testing can identify carriers of the mutations and help manage treatment options and preventive measures for affected families.
By understanding the prevalence and genetic factors associated with hypertrophic cardiomyopathy, individuals at risk can seek early diagnosis and appropriate management, potentially mitigating the severe outcomes associated with this condition.
Symptoms of Hypertrophic Cardiomyopathy (HCM)
Understanding these symptoms is crucial for early diagnosis and effective management. Here’s a detailed look at the common symptoms associated with HCM, their manifestations, and the underlying causes.
Common Symptoms of Hypertrophic Cardiomyopathy
- Shortness of Breath: Often experienced during exertion or sometimes at rest, this symptom occurs because the thickened heart muscle can make it harder for the heart to fill with blood, leading to increased pressure in the lungs.
- Chest Pain (Angina): Patients may experience pain or discomfort in the chest, typically during activities. This happens because the thickened heart muscle requires more oxygen than the narrowed coronary arteries can supply.
- Palpitations: These are sensations of a fast-beating, fluttering, or irregular heartbeat. They arise from abnormal electrical pathways or signals in the thickened heart muscle.
- Fatigue: This common symptom occurs as a result of the heart’s reduced capacity to pump blood efficiently, leading to lower oxygen delivery to the body.
- Dizziness or Lightheadedness: These symptoms can occur if the brain does not receive enough blood due to the impaired pumping ability of the heart.
- Fainting (Syncope): This can happen during or after physical activity or emotional stress. It is typically caused by a sudden drop in blood pressure or abnormal heart rhythms associated with HCM.
How These Symptoms Manifest and Their Causes
The primary cause of these symptoms is the thickening of the heart’s ventricular muscle (myocardium), which impairs the heart’s ability to pump blood effectively. As the condition progresses, the heart becomes stiffer, further restricting blood flow to and from the heart. The lack of adequate blood flow triggers the symptoms like dizziness, palpitations, and chest pain.
Moreover, the irregular structure of the heart muscle in HCM can disrupt the normal electrical signals that control the heartbeat, leading to arrhythmias, which are responsible for palpitations and, in some severe cases, sudden cardiac death.
Sidebar: Personal Stories of Individuals with HCM
Case Study 1: John, Age 34 – John first noticed his symptoms during a hiking trip when he experienced severe shortness of breath and fainting. A subsequent medical examination led to his HCM diagnosis. Managing his condition with medication and lifestyle adjustments, John continues to lead an active life with careful monitoring.
Case Study 2: Anita, Age 29 – Anita’s journey began with unexplained fatigue and palpitations. It took several visits to different healthcare providers before she was diagnosed with HCM. With the right treatment plan, including surgery to reduce the thickened muscle, Anita has seen significant improvement in her symptoms.
These personal stories highlight the varied ways HCM can present itself and the importance of awareness and early diagnosis in managing the disease effectively.
For those experiencing these symptoms, consulting with a healthcare provider is essential for a proper diagnosis and appropriate treatment plan.
Causes and Risk Factors of Hypertrophic Cardiomyopathy
Understanding the causes and risk factors associated with this condition is crucial for both patients and healthcare providers. Here’s a deeper look into the genetic basis, inheritance patterns, and other contributing factors of HCM.
Genetic Basis of HCM: Role of Mutations in Specific Genes
The primary cause of Hypertrophic Cardiomyopathy is genetic mutations in the genes that encode for the proteins making up the heart muscle. These mutations cause the heart muscle cells to grow larger and work less efficiently. Key genes involved include MYH7 and MYBPC3, which play significant roles in heart muscle structure and function. Mutations in these genes can disrupt the normal alignment and function of heart muscle fibers, leading to the thickening of the heart walls.
How HCM is Inherited: Autosomal Dominant Pattern
Hypertrophic Cardiomyopathy is typically inherited in an autosomal dominant pattern. This means that a single copy of the mutated gene, inherited from one parent, is sufficient to cause the condition. Children of a parent with HCM have a 50% chance of inheriting the gene mutation. This pattern of inheritance underscores the importance of genetic counseling and testing for families affected by HCM.
Other Contributing Factors
In addition to genetic predisposition, several other factors can contribute to the development or worsening of HCM. These include:
- High Blood Pressure: Elevated blood pressure can increase cardiac workload and myocardial thickness, exacerbating the condition in individuals predisposed to or already having HCM.
- Age-Related Changes in the Heart: As people age, natural changes in heart structure and function can aggravate or reveal underlying HCM, particularly in those with genetic predispositions.
The Role of Environmental Factors vs. Genetics in the Development of HCM
While genetics play a pivotal role in the development of Hypertrophic Cardiomyopathy, environmental factors also contribute to its manifestation and progression. Lifestyle factors such as diet, exercise, and stress management can influence the severity of HCM symptoms and the overall heart health. However, the primary driver of HCM is genetic mutations, with environmental factors playing a more secondary role in affecting the heart condition’s impact.
However, understanding the complex interplay between genetics and environmental factors is essential for managing and potentially mitigating the effects of HCM. Early detection through genetic screening and managing lifestyle factors can help manage or even improve the condition’s prognosis.
Complications Related to Hypertrophic Cardiomyopathy
Understanding these complications and how they relate to the symptoms of HCM is crucial for patients and healthcare providers alike. Here, we’ll explore the key complications associated with hypertrophic cardiomyopathy and discuss how the symptoms can indicate these serious issues.
Key Complications of Hypertrophic Cardiomyopathy
- Arrhythmias: HCM often leads to irregular heartbeats, or arrhythmias, which can be benign or life-threatening. The most common types include atrial fibrillation, which increases the risk of stroke, and ventricular tachycardia, which can lead to sudden cardiac arrest.
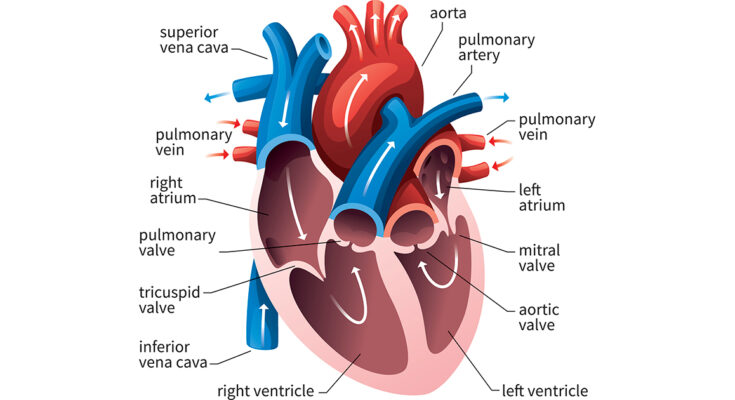
- Obstructive Symptoms: In many patients, the thickened heart muscle can block or reduce the flow of blood from the left ventricle to the aorta (known as obstructive hypertrophic cardiomyopathy). This can cause severe symptoms, including chest pain, fainting, and extreme fatigue during exertion.
- Heart Failure: Despite the heart muscle being thick and strong, its function can be impaired over time. HCM can lead to heart failure, where the heart is unable to pump blood efficiently, resulting in fluid buildup, swelling, and shortness of breath.
- Mitral Valve Problems: The abnormal structure of the heart muscle in HCM can affect the mitral valve, leading to mitral regurgitation. This condition allows blood to flow backward into the heart, causing further complications and symptoms.
- Sudden Cardiac Death: Although relatively rare, HCM is one of the most common causes of sudden cardiac death in young athletes. The risk is higher in those with severe symptoms or a family history of HCM.
How Symptoms Relate to These Complications
- Arrhythmias: Symptoms like palpitations, dizziness, or fainting can indicate the presence of arrhythmias in patients with HCM. These symptoms often require immediate medical attention to prevent more severe complications.
- Obstructive Symptoms: Shortness of breath, especially during exercise, chest pain, and episodes of fainting are direct manifestations of the obstructive nature of HCM. These symptoms often worsen with physical activity as the demand for blood flow increases.
- Heart Failure: Progressive shortness of breath, fatigue, and swelling in the legs and ankles can be signs of developing heart failure in HCM patients. These symptoms usually occur due to the heart’s decreasing efficiency in pumping blood.
- Mitral Valve Problems: Symptoms such as a heart murmur (detected by a healthcare provider), fatigue, and shortness of breath might suggest complications with the mitral valve due to the altered heart structure.
- Sudden Cardiac Death: While sudden cardiac death may occur without warning, some potential indicators include recurrent fainting spells, severe chest pain, or extreme fatigue, which could signal an increased risk in individuals with HCM.
Patients experiencing these symptoms should seek immediate medical evaluation to reduce the risk of severe outcomes and improve overall health management.
Diagnosis of Hypertrophic Cardiomyopathy
Accurate diagnosis is crucial for effective management and treatment of the condition. Here’s a detailed look at how hypertrophic cardiomyopathy is diagnosed, emphasizing the importance of early detection and the key diagnostic tests involved.
Physical Examination and Medical History
The initial steps in diagnosing hypertrophic cardiomyopathy involve a thorough physical examination and a comprehensive review of the patient’s medical history. During the physical exam, a healthcare provider listens for abnormal heart sounds or murmurs that may indicate HCM. Reviewing medical history helps identify any genetic patterns or symptoms consistent with the disease, such as chest pain, shortness of breath, or fainting spells, which are common in affected individuals.
Key Diagnostic Tests
Several key tests are essential in confirming a diagnosis of hypertrophic cardiomyopathy:
- Echocardiogram: This is the most critical test for diagnosing HCM. An echocardiogram uses ultrasound waves to create detailed images of the heart, allowing doctors to see the thickness of the heart muscle and how well the heart is pumping. It also helps in assessing whether the flow of blood is obstructed out of the heart.
- Magnetic Resonance Imaging (MRI): An MRI of the heart provides detailed images of the heart’s structure and function. It can show the extent of muscle thickening and detect minute changes in heart tissue, which can be vital for diagnosing HCM and planning treatment.
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart. It can detect abnormal rhythms, which are common in patients with hypertrophic cardiomyopathy, and provide clues about heart muscle thickness.
Importance of Early Detection
Early detection of hypertrophic cardiomyopathy is crucial. It allows for timely intervention, which can significantly improve the prognosis and quality of life for those affected. Early diagnosis can help prevent complications such as sudden cardiac death, heart failure, and stroke. Regular monitoring and appropriate management can also alleviate symptoms and reduce the risk of severe cardiac events.
By understanding and recognizing the signs and symptoms of HCM early, individuals can seek the necessary medical evaluation and intervention that can lead to a better outcome. Therefore, it is essential for individuals with a family history of HCM or related symptoms to undergo regular check-ups and diagnostic tests as recommended by a healthcare professional.
Treatment Options for Hypertrophic Cardiomyopathy
Managing this condition involves a multi-faceted approach that includes lifestyle adjustments, medical treatments, and innovative therapies on the horizon. Here’s a detailed look at the treatment options available for individuals diagnosed with HCM.
Lifestyle Adjustments and Managing Risk Factors
Lifestyle changes play a crucial role in managing hypertrophic cardiomyopathy. Patients are generally advised to:
- Modify Physical Activity: Vigorous exercise can be dangerous for people with HCM, so it’s essential to tailor exercise routines under medical guidance.
- Monitor Diet and Nutrition: Maintaining a healthy weight reduces stress on the heart. A balanced diet low in sodium and saturated fats is advisable.
- Avoid Dehydration: Staying hydrated helps maintain blood volume and pressure, facilitating easier heart function.
- Limit Alcohol and Tobacco Use: Alcohol can trigger arrhythmias in HCM patients, and smoking can exacerbate heart disease.
- Manage Stress: Chronic stress can negatively impact heart health, so employing stress management techniques like meditation or yoga can be beneficial.
Addressing these lifestyle factors can significantly reduce symptoms and improve quality of life.
Medical Treatments
Medications are often the first line of defense in managing hypertrophic cardiomyopathy. Common prescriptions include:
- Beta-blockers: Slow the heart rate and reduce the force of the heart’s contractions.
- Calcium channel blockers: Help relax the heart muscle and reduce the heart’s workload.
- Antiarrhythmic drugs: Used to control heart rhythm disturbances.
In some cases, medications alone aren’t sufficient to manage HCM symptoms or risks.
Surgical Options
When symptoms are severe or there is a significant risk of sudden cardiac death, surgical interventions may be necessary:
- Myectomy: Removal of a portion of the thickened heart muscle wall to improve blood flow.
- Septal ablation: A minimally invasive procedure where a small portion of the thickened heart muscle is destroyed using alcohol introduced through a catheter.
These procedures are typically recommended when symptoms persist despite medical management.
Implanted Devices
For patients at high risk of sudden cardiac death, implanted devices such as defibrillators may be recommended. These devices monitor heart rhythms and can deliver electric shocks to restore a normal heartbeat when necessary.
Advances in Treatment and Potential Future Therapies
Research into hypertrophic cardiomyopathy is ongoing, and recent advances offer hope for even more effective treatments in the future. Potential new therapies include:
- Genetic therapies: Targeting the genetic mutations that cause HCM could revolutionize treatment.
- Advanced imaging techniques: Improving the diagnosis and ongoing monitoring of HCM.
- Novel pharmaceuticals: Drugs that can more precisely target the cellular mechanisms of HCM are under development.
These emerging therapies highlight the importance of ongoing research and clinical trials in the quest to better understand and treat hypertrophic cardiomyopathy.
However, with advancements in medical science, the outlook for managing HCM continues to improve, offering patients a better quality of life and longer life expectancy.
FAQs about Hypertrophic Cardiomyopathy Symptoms
What are the common symptoms of hypertrophic cardiomyopathy?
Hypertrophic cardiomyopathy (HCM) symptoms often include shortness of breath, chest pain, and fainting, especially during physical activity. Some individuals might experience palpitations or heart murmurs. However, many people with HCM may not exhibit any symptoms.
Can hypertrophic cardiomyopathy be asymptomatic?
Yes, hypertrophic cardiomyopathy can be asymptomatic. Some individuals with HCM might not show any symptoms and may only discover their condition during routine medical exams or screenings.
How is chest pain associated with hypertrophic cardiomyopathy?
Chest pain in HCM is usually caused by reduced blood flow to the heart muscle. This can occur during physical exertion when the heart’s demand for oxygen increases.
Are palpitations a common symptom of hypertrophic cardiomyopathy?
Yes, palpitations are a common symptom of HCM. They are often due to abnormal heart rhythms, which can occur because the heart muscle is thickened and can affect the heart’s electrical system.
When should I seek medical attention for hypertrophic cardiomyopathy symptoms?
Seek medical attention if you experience unexplained chest pain, shortness of breath, fainting, or palpitations, especially if these symptoms occur during physical activity. Early diagnosis and treatment are crucial for managing HCM effectively.
Conclusion:
Understanding and recognizing the symptoms of Hypertrophic Cardiomyopathy (HCM) is crucial for early diagnosis and management. HCM, characterized by the thickening of the heart muscle, can lead to serious health complications if left unaddressed. Symptoms such as shortness of breath, chest pain, palpitations, and fainting should not be overlooked, as they are key indicators of this condition.
Awareness of the causes and risk factors associated with HCM, including genetic predispositions and lifestyle factors, empowers individuals to take proactive steps towards their heart health. If you or someone you know is experiencing any symptoms suggestive of HCM, it is essential to consult a healthcare provider. Early screening and diagnosis can lead to effective management strategies and significantly improve the quality of life.
Take action today: Don’t ignore potential symptoms. Reach out to your healthcare provider for a comprehensive evaluation and ensure your heart’s health for the future.
References
For further reading and to validate the information provided about Hypertrophic Cardiomyopathy Symptoms, we recommend consulting the following reputable sources:
- Mayo Clinic: Hypertrophic Cardiomyopathy
An in-depth guide on the symptoms, causes, and treatments of Hypertrophic Cardiomyopathy.
Read more on Mayo Clinic - American Heart Association: What is Hypertrophic Cardiomyopathy?
Comprehensive information on the diagnosis, management, and support resources available for those with Hypertrophic Cardiomyopathy.
Learn more on the American Heart Association - Johns Hopkins Medicine: Hypertrophic Cardiomyopathy
Detailed overview of the condition, including its genetic aspects and the latest research findings.
Explore Johns Hopkins Medicine
These resources provide valuable insights and are excellent starting points for anyone looking to understand Hypertrophic Cardiomyopathy better.