Hyperhidrosis Symptoms: Hyperhidrosis, commonly known as excessive sweating, is a medical condition that affects millions of people worldwide.
This condition can significantly impact an individual’s quality of life, leading to physical discomfort, social anxiety, and emotional distress.
In this comprehensive article, we delve into the symptoms and causes of hyperhidrosis, providing detailed information to help you understand this often misunderstood condition.
What is Hyperhidrosis?
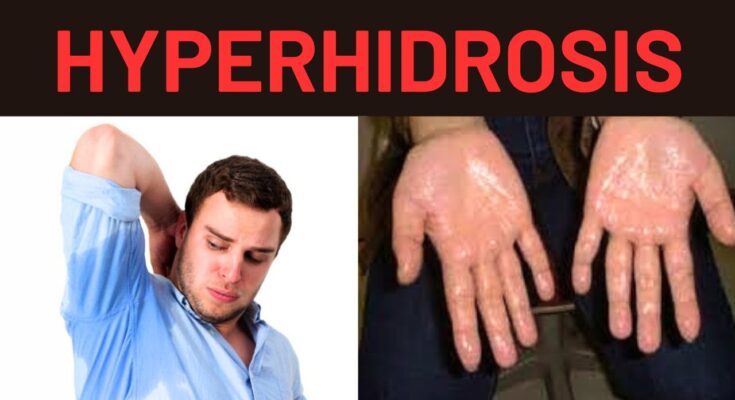
Hyperhidrosis is a medical condition characterized by excessive sweating that goes beyond what is necessary to regulate body temperature. This condition can significantly impact daily life, causing physical discomfort and emotional distress. Individuals with hyperhidrosis may experience sweating in specific areas such as the hands, feet, underarms, or face, or it can be generalized across the body.
Types of Hyperhidrosis
Hyperhidrosis is generally categorized into two main types:
- Primary (Focal) Hyperhidrosis: This type is the most common and usually begins in childhood or adolescence. It typically affects specific areas of the body such as the palms, soles, underarms, and face. The exact cause is unknown, but it is thought to be related to overactive sweat glands.
- Secondary (Generalized) Hyperhidrosis: This type is less common and usually occurs in adulthood. It is often caused by an underlying medical condition or as a side effect of certain medications. Unlike primary hyperhidrosis, secondary hyperhidrosis can cause sweating all over the body and tends to appear suddenly.
Prevalence and Demographic Information
Hyperhidrosis affects approximately 2-3% of the population. Primary hyperhidrosis typically starts during childhood or adolescence, with many individuals experiencing symptoms by the age of 25. It affects both men and women equally and can occur in people of all races and ethnicities.
Secondary hyperhidrosis, on the other hand, can develop at any age and is more likely to be associated with other medical conditions such as diabetes, thyroid disorders, menopause, or infections. Certain medications, including antidepressants and antipyretics, can also trigger excessive sweating.
However, understanding hyperhidrosis and its types is essential for seeking appropriate treatment and improving the quality of life for those affected by this condition.
Hyperhidrosis Symptoms
Here are some common symptoms and their impact on daily life:
Common Symptoms of Hyperhidrosis
- Excessive Sweating: Sweating that is disproportionate to the surrounding temperature or activity level, often occurring in specific areas such as the palms, soles, underarms, and face.
- Visible Moisture: Constant dampness or wetness in affected areas, leading to visibly soaked clothing and a need for frequent changes of attire.
- Skin Issues: Increased risk of skin infections, rashes, and irritation due to prolonged moisture exposure.
- Cold and Clammy Skin: The skin may feel cool and clammy, especially in the palms and soles.
- Unpleasant Odor: Persistent sweating can lead to a stronger body odor, which might be hard to manage even with regular hygiene practices.
Impact on Daily Life
- Emotional Distress: The constant worry about visible sweat stains and body odor can lead to anxiety, embarrassment, and decreased self-confidence.
- Social Interactions: Avoidance of social situations, handshakes, or close contact due to fear of judgment can affect relationships and social life.
- Work and Productivity: Difficulty handling paper documents, tools, or electronic devices due to sweaty hands can hinder job performance and productivity.
- Clothing Choices: The need to choose clothing that hides sweat stains can limit wardrobe options and lead to additional costs for extra laundry or dry cleaning.
- Daily Activities: Activities like exercising, cooking, or driving can become uncomfortable or challenging due to excessive sweating.
However, hyperhidrosis can significantly impact one’s quality of life. Recognizing these symptoms and their effects is crucial for seeking appropriate treatment and support.
Causes of Hyperhidrosis
Understanding its causes can help in managing and treating the condition. Hyperhidrosis is generally categorized into two types: primary and secondary.
Primary Hyperhidrosis Causes
Primary hyperhidrosis, also known as focal hyperhidrosis, typically affects specific areas of the body such as the palms, soles, underarms, and face. The exact cause of primary hyperhidrosis is not fully understood, but it is believed to be related to overactive sweat glands. Genetics play a crucial role, as this condition often runs in families.
- Genetic Factors: A significant number of primary hyperhidrosis cases have a family history of excessive sweating, indicating a hereditary component.
- Overactive Sweat Glands: The sympathetic nervous system, which controls sweating, may be overly active, leading to excessive sweat production.
Secondary Hyperhidrosis Causes
Secondary hyperhidrosis, unlike primary hyperhidrosis, is usually caused by an underlying medical condition or is a side effect of certain medications. It tends to affect larger areas of the body and can occur during sleep.
- Medical Conditions: Various medical conditions can lead to secondary hyperhidrosis, including diabetes, hyperthyroidism, menopause, obesity, and infections.
- Medications: Certain medications, such as antidepressants, antipyretics, and antipsychotics, can cause excessive sweating as a side effect.
- Hormonal Changes: Hormonal imbalances, such as those occurring during menopause or due to endocrine disorders, can trigger hyperhidrosis.
- Neurological Disorders: Conditions like Parkinson’s disease, spinal cord injuries, and stroke can lead to secondary hyperhidrosis.
However, consulting a healthcare professional can provide a proper diagnosis and treatment plan tailored to the specific cause of excessive sweating.
Diagnosis of Hyperhidrosis
Diagnosing hyperhidrosis is essential for managing excessive sweating that can disrupt daily activities and decrease quality of life. An accurate diagnosis helps in identifying the underlying causes and determining the most effective treatment options.
Medical Evaluation Process
The process of diagnosing hyperhidrosis typically begins with a thorough medical evaluation:
- Patient History: Doctors start by gathering a detailed history of the patient’s sweating patterns. This includes when and where the excessive sweating occurs, any triggering factors, and family history of similar issues.
- Physical Examination: A physical exam is conducted to assess the areas affected by excessive sweating and to look for any related skin changes or signs of other health conditions.
- Symptom Assessment: Patients may be asked about the impact of sweating on their daily life, including social, professional, and emotional aspects.
Diagnostic Tests
Several tests can help in the diagnosis of hyperhidrosis, including:
- Starch-Iodine Test: This involves applying an iodine solution to the sweaty area. Once dry, starch is sprinkled over the iodine. When the starch mixes with the sweat, it turns dark, highlighting the affected areas.
- Paper Test: Special paper is placed on the affected areas to absorb sweat, and the weight of the paper is measured after a certain time to determine the amount of sweat produced.
- Thermoregulatory Sweat Test: A powder that changes color when exposed to sweat is applied to the body. The patient then enters a chamber that heats up, triggering sweating. This test maps the areas of excessive sweating and helps in understanding the pattern.
Importance of Early Diagnosis
Early diagnosis of hyperhidrosis is crucial:
- Improves Treatment Outcomes: Early diagnosis allows for the timely implementation of treatment strategies, which can be more effective at managing symptoms before they worsen.
- Reduces Psychological Impact: Addressing hyperhidrosis early can help prevent the psychological distress associated with the condition, such as anxiety and social withdrawal.
- Prevents Complications: Early treatment helps prevent skin infections and other complications related to excessive moisture, such as dermatitis.
By understanding the diagnosis process of hyperhidrosis, patients and healthcare providers can better navigate the options for managing this challenging condition. Early and accurate diagnosis is the first step towards effective treatment and improved quality of life.
Treatment Options for Hyperhidrosis
Fortunately, there are several treatment options available, ranging from non-invasive methods to surgical interventions. Here’s a comprehensive look at the treatment options for hyperhidrosis:
Non-Invasive Treatments
- Antiperspirants: Over-the-counter antiperspirants containing aluminum chloride can be effective for mild cases of hyperhidrosis. Prescription-strength antiperspirants are also available for more severe cases.
- Lifestyle Changes: Wearing breathable clothing, maintaining good hygiene, and managing stress through relaxation techniques can help reduce sweating.
- Iontophoresis: This involves using a device that passes a mild electrical current through water and into the skin’s surface, which can reduce sweating in the hands and feet.
- Botox Injections: Botulinum toxin injections can temporarily block the nerves that cause sweating, providing relief for several months.
Medical Treatments
- Prescription Antiperspirants: Stronger than over-the-counter options, these require a doctor’s prescription and are typically used for underarm sweating.
- Oral Medications: Anticholinergic drugs can reduce sweating by blocking the chemical messengers that stimulate sweat glands. However, they may have side effects like dry mouth and blurred vision.
- Topical Medications: Glycopyrrolate and other medicated creams can be applied to areas prone to excessive sweating, such as the face and scalp.
Surgical Treatments
- Endoscopic Thoracic Sympathectomy (ETS): This surgical procedure involves cutting or clamping the nerves that trigger sweating in specific areas of the body, such as the hands. It is usually considered when other treatments have failed.
- Sweat Gland Removal: In severe cases, surgery to remove sweat glands can be performed, particularly in the underarm area. Techniques include excision, curettage, and laser treatments.
- Microwave Therapy: A newer surgical option, microwave therapy uses electromagnetic energy to destroy sweat glands, offering a long-term solution with minimal downtime.
By understanding and exploring these various treatment options, individuals with hyperhidrosis can find relief and improve their quality of life. Always consult a healthcare professional to determine the best treatment plan tailored to your specific needs.
Lifestyle and Home Remedies for Hyperhidrosis
Hyperhidrosis, or excessive sweating, can be a challenging condition to manage. However, there are effective lifestyle changes and home remedies that can help you control your symptoms and improve your quality of life.
Tips for Managing Symptoms at Home
- Antiperspirants: Use over-the-counter or prescription-strength antiperspirants. Apply them at night to allow the active ingredients to work overnight. Look for products containing aluminum chloride, which is effective in reducing sweating.
- Stay Cool: Keep your environment cool and well-ventilated. Use fans, air conditioning, and wear breathable, loose-fitting clothing made of natural fibers like cotton. Avoid synthetic fabrics that can trap heat and moisture.
- Hygiene: Maintain good hygiene by showering daily with antibacterial soap. This helps to reduce bacteria on the skin, which can cause odor when mixed with sweat.
- Diet: Watch your diet. Spicy foods, caffeine, and alcohol can trigger excessive sweating. Opt for a balanced diet rich in fruits, vegetables, and lean proteins. Staying hydrated is also crucial to regulate body temperature.
- Absorbent Pads: Use absorbent pads or sweat shields. These can be placed inside clothing to absorb excess sweat and prevent visible stains.
- Foot Care: For those experiencing hyperhidrosis in the feet, change socks frequently and opt for moisture-wicking materials. Use antifungal powders to keep feet dry and reduce the risk of infections.
- Stress Reduction: Since stress and anxiety can exacerbate sweating, incorporating stress management techniques into your routine is essential.
Stress Management Techniques
- Mindfulness and Meditation: Practice mindfulness meditation to help reduce anxiety and stress. Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can be particularly effective.
- Regular Exercise: Engage in regular physical activity to help manage stress. Exercise releases endorphins, which are natural stress relievers. Activities like yoga, tai chi, or even a brisk walk can make a significant difference.
- Adequate Sleep: Ensure you get enough sleep each night. Quality sleep is crucial for stress management and overall well-being. Aim for 7-9 hours of uninterrupted sleep per night.
- Healthy Social Connections: Maintain strong social connections. Talking with friends and family or participating in social activities can provide emotional support and reduce stress levels.
- Hobbies and Relaxation: Engage in hobbies and activities that you enjoy. Whether it’s reading, gardening, or playing a musical instrument, taking time for yourself can be a great way to relax and de-stress.
By incorporating these lifestyle and home remedies, you can better manage the symptoms of hyperhidrosis and improve your overall quality of life. If symptoms persist, consult a healthcare professional for further advice and treatment options.
Living with Hyperhidrosis
Hyperhidrosis, a condition characterized by excessive sweating, can significantly impact daily life. Whether it’s constant perspiration or damp palms, the condition can be challenging. However, there are effective coping strategies, support groups, and personal stories that offer hope and guidance.
Coping Strategies
- Antiperspirants: Clinical-strength antiperspirants are more effective than regular ones and can be applied to various parts of the body, not just underarms.
- Lifestyle Adjustments: Wearing breathable fabrics, avoiding spicy foods, and managing stress can help reduce sweating episodes.
- Medical Treatments: Options include prescription medications, Botox injections, iontophoresis (a treatment involving electrical currents), and, in severe cases, surgery.
- Hygiene Practices: Regular showers, using antibacterial soaps, and keeping affected areas dry can help manage symptoms and prevent infections.
- Absorbent Products: Items such as sweat pads, absorbent shoe inserts, and moisture-wicking clothing can provide comfort and confidence.
Support Groups and Resources
Connecting with others who understand the challenges of hyperhidrosis can be incredibly beneficial. Consider joining these support groups and exploring resources:
- International Hyperhidrosis Society: This organization offers a wealth of information, support forums, and updates on the latest treatments.
- Online Forums: Websites like Reddit and HealthUnlocked have communities where individuals share experiences, tips, and support.
- Local Support Groups: Check if there are any local meetups or support groups in your area. Sometimes hospitals or dermatology clinics can provide information about these.
- Social Media Groups: Facebook and other social media platforms have groups dedicated to hyperhidrosis support, where members exchange advice and encouragement.
- Educational Resources: Books, podcasts, and YouTube channels focused on hyperhidrosis can provide additional insights and coping mechanisms.
Personal Stories and Testimonials
Hearing from others who live with hyperhidrosis can be both inspiring and reassuring. Here are a few personal stories that highlight resilience and offer practical advice:
- Sarah’s Story: “I’ve dealt with hyperhidrosis since my teenage years. Discovering clinical-strength antiperspirants and practicing mindfulness techniques has been a game-changer for me.”
- Michael’s Journey: “Botox injections helped me manage my excessive sweating. It’s a relief to shake hands confidently during business meetings now.”
- Emily’s Experience: “Joining an online support group made a huge difference. Knowing I’m not alone and having a safe space to share my struggles has been incredibly empowering.”
- John’s Advice: “I underwent iontophoresis, and it drastically reduced the sweating in my hands. It took a few sessions, but the results were worth it.”
- Rachel’s Testimonial: “Simple changes like wearing loose, cotton clothing and avoiding spicy foods have helped me manage my symptoms better.”
However, living with hyperhidrosis can be challenging, but with the right strategies, support, and inspiration from others, it’s possible to lead a comfortable and fulfilling life.
FAQs about Hyperhidrosis Symptoms
What is hyperhidrosis?
Hyperhidrosis is a medical condition characterized by excessive sweating beyond what is necessary for body temperature regulation. It can affect various body parts, including the underarms, hands, feet, and face.
What are the common symptoms of hyperhidrosis?
The primary symptom of hyperhidrosis is excessive sweating. This can occur in specific areas like the palms, soles, underarms, or face. The sweating often occurs without any physical activity or external heat.
How can I tell if I have hyperhidrosis?
If you experience frequent, uncontrollable sweating that interferes with your daily activities, you might have hyperhidrosis. Common indicators include constantly wet palms, noticeable sweat stains on clothes, and persistent dampness.
Is hyperhidrosis a serious condition?
While hyperhidrosis is not life-threatening, it can significantly impact the quality of life. It can cause emotional distress, social embarrassment, and discomfort. It’s important to seek medical advice if you suspect you have this condition.
What causes hyperhidrosis?
Hyperhidrosis can be primary or secondary. Primary hyperhidrosis often has no identifiable cause and may be hereditary. Secondary hyperhidrosis results from other medical conditions or medications.
Can hyperhidrosis be treated?
Yes, several treatments are available for hyperhidrosis. These include antiperspirants, prescription medications, iontophoresis, Botox injections, and in severe cases, surgical options. Consulting a healthcare provider can help determine the best treatment plan for you.
Are there lifestyle changes that can help manage hyperhidrosis?
Yes, lifestyle changes can help manage symptoms. Wearing breathable fabrics, using clinical-strength antiperspirants, staying hydrated, and avoiding triggers like spicy foods and caffeine can reduce sweating.
When should I see a doctor about my sweating?
You should see a doctor if your sweating is excessive, causing emotional or physical discomfort, or affecting your daily activities. A healthcare provider can diagnose hyperhidrosis and recommend appropriate treatments.
Conclusion
Hyperhidrosis is characterized by excessive sweating, which can affect various parts of the body such as the hands, feet, underarms, and face. This condition often disrupts daily activities, causing discomfort and embarrassment. Key symptoms include noticeable and frequent sweating that soaks through clothing or leads to clammy hands and feet, even in cool or non-stressful environments.
If you are experiencing these symptoms, it’s important to seek medical advice. Consulting a healthcare professional can help you identify the underlying cause and explore effective treatments. Don’t let hyperhidrosis control your life—take the first step towards managing your symptoms and improving your quality of life by reaching out for medical support.
References
For further reading and validation of the information provided in this article on hyperhidrosis symptoms, please refer to the reputable sources listed below:
- International Hyperhidrosis Society – Comprehensive information on hyperhidrosis, including symptoms, causes, and treatment options.
- Mayo Clinic – Detailed overview of hyperhidrosis symptoms, diagnosis, and management.
- WebMD – In-depth articles on the symptoms and treatments of hyperhidrosis.
- National Institutes of Health (NIH) – Scientific studies and research articles related to hyperhidrosis and its impact on patients.
- American Academy of Dermatology (AAD) – Expert insights and guidelines on diagnosing and treating hyperhidrosis.
These sources provide valuable insights and further validation of the information discussed in this article.