Hyperhidrosis Treatment: Hyperhidrosis, commonly referred to as excessive sweating, is a medical condition characterized by abnormal perspiration levels.
This condition can significantly impact the quality of life, affecting both physical comfort and emotional well-being.
In this article, we will delve into the comprehensive details surrounding hyperhidrosis, including its diagnosis, underlying causes, and various treatment options.
What is Hyperhidrosis?
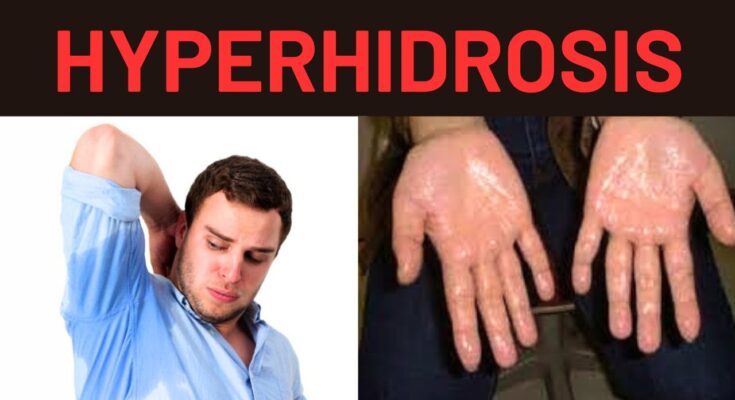
Hyperhidrosis is a medical condition characterized by excessive sweating beyond what is necessary to regulate body temperature. This condition can affect various parts of the body, including the hands, feet, underarms, and face. The excessive sweating can occur even in cool temperatures or without any apparent triggers such as physical activity or heat.
Primary and Secondary Causes
Hyperhidrosis is categorized into two main types: primary (idiopathic) hyperhidrosis and secondary hyperhidrosis.
- Primary (Idiopathic) Hyperhidrosis: This type is not caused by any other medical condition. It usually begins in childhood or adolescence and often affects specific areas like the palms, soles, underarms, or face. The exact cause of primary hyperhidrosis is unknown, but it is believed to be related to overactive sweat glands and possibly genetic factors.
- Secondary Hyperhidrosis: This type is caused by an underlying medical condition or as a side effect of certain medications. Conditions that can lead to secondary hyperhidrosis include diabetes, thyroid disorders, menopause, infections, and neurological conditions. Unlike primary hyperhidrosis, secondary hyperhidrosis typically starts in adulthood and can affect larger or generalized areas of the body.
Statistics on Prevalence and Demographics
Hyperhidrosis is more common than many might think. Studies indicate that approximately 2-3% of the global population suffers from this condition. Both men and women are affected equally, but the onset and severity can vary. Primary hyperhidrosis often begins in childhood or adolescence, while secondary hyperhidrosis typically appears in adulthood.
If you suspect you have hyperhidrosis, consult a healthcare professional for proper diagnosis and management strategies.
Symptoms of Hyperhidrosis
Understanding the symptoms can help in identifying and managing this condition effectively. Below is a list of common symptoms and the typical areas affected by hyperhidrosis.
Common Symptoms of Hyperhidrosis
- Excessive Sweating: The primary symptom of hyperhidrosis is excessive sweating that is beyond what is needed for regulating body temperature. This can occur even in cool environments or when at rest.
- Visible Sweating: Profuse sweating that can soak through clothing or drip from hands, face, or feet.
- Frequent Sweating Episodes: Episodes of intense sweating occurring multiple times a week, often without any clear trigger.
- Skin Issues: Prolonged exposure to moisture can lead to skin maceration, infections, and fungal growths.
- Emotional and Social Impact: Excessive sweating can lead to social embarrassment, anxiety, and withdrawal from social activities.
Typical Areas Affected by Hyperhidrosis
Hyperhidrosis can affect various parts of the body, but some areas are more commonly affected than others:
- Hands (Palmar Hyperhidrosis): Excessive sweating of the palms, making handshakes or handling objects difficult.
- Feet (Plantar Hyperhidrosis): Sweaty feet can lead to foot odor, infections, and discomfort in shoes.
- Armpits (Axillary Hyperhidrosis): Excessive sweating under the arms, leading to visible stains on clothing and potential odor issues.
- Face and Scalp: Sweating on the forehead, scalp, and face, which can be particularly noticeable and embarrassing.
- Generalized Areas: In some cases, hyperhidrosis can affect the entire body, though this is less common.
However, if you suspect you have hyperhidrosis, consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
Diagnosing Hyperhidrosis
Accurately diagnosing this condition is crucial for effective treatment. Here’s a comprehensive guide on the diagnostic process for hyperhidrosis, emphasizing the importance of medical history, physical examination, and specific tests.
Step-by-Step Diagnostic Process
1. Medical History
The first step in diagnosing hyperhidrosis involves a detailed medical history. Your healthcare provider will ask about:
- Sweating Patterns: When and where you experience excessive sweating.
- Triggers: Factors that seem to exacerbate sweating, such as stress or heat.
- Family History: Whether hyperhidrosis runs in your family.
- Associated Symptoms: Any additional symptoms, like weight loss or fever, that might indicate other conditions.
A thorough medical history helps identify the type of hyperhidrosis (primary or secondary) and potential underlying causes.
2. Physical Examination
A physical examination is essential to observe and document the extent of sweating. Your doctor will:
- Inspect Affected Areas: Look at the areas where sweating is most severe.
- Assess General Health: Check for signs of other conditions that could cause excessive sweating.
- Evaluate Skin Health: Ensure there are no skin infections or irritations resulting from excessive moisture.
3. Diagnostic Tests
Several tests and procedures can help confirm a hyperhidrosis diagnosis:
- Starch-Iodine Test: A simple test where iodine is applied to the sweaty area, followed by starch. The combination turns dark blue in the presence of excessive sweat, highlighting the problem areas.
- Paper Test: Special paper is placed on the skin to absorb sweat. The paper is then weighed to measure the amount of sweat produced.
- Thermoregulatory Sweat Test: This test involves coating the body with a powder that changes color in response to moisture. The patient is then exposed to a controlled environment to induce sweating, and the results are analyzed to pinpoint areas of excessive sweating.
Importance of Accurate Diagnosis
Diagnosing hyperhidrosis accurately is vital for developing an effective treatment plan. Understanding your specific condition allows healthcare providers to recommend targeted therapies, improving your quality of life and helping manage symptoms effectively.
By following this step-by-step guide, you and your healthcare provider can work together to diagnose hyperhidrosis accurately and start the journey toward effective management and relief.
Conventional Treatments for Hyperhidrosis
Hyperhidrosis, or excessive sweating, can be challenging to manage. Fortunately, there are several conventional treatments available that can help. Here are some of the most effective options:
Topical Treatments
Antiperspirants containing aluminum chloride: One of the most common treatments for hyperhidrosis is using antiperspirants that contain aluminum chloride. These products work by blocking the sweat glands, thereby reducing the amount of sweat produced. They are typically applied at night to dry skin and can be very effective for mild to moderate cases of hyperhidrosis.
Oral Medications
Oral medications can also be used to manage hyperhidrosis. Here are some of the commonly prescribed drugs:
- Anticholinergics: These medications, such as glycopyrrolate and oxybutynin, work by blocking the neurotransmitters that stimulate sweat glands. While effective, they can have side effects like dry mouth, blurred vision, and urinary retention.
- Beta-blockers and Benzodiazepines: These are sometimes prescribed for situational hyperhidrosis triggered by stress or anxiety. Beta-blockers (e.g., propranolol) and benzodiazepines (e.g., diazepam) can help reduce symptoms but may cause drowsiness and other side effects.
Advanced Treatments
For more severe cases of hyperhidrosis, advanced treatments may be necessary:
- Iontophoresis: This treatment involves using a device that passes a mild electrical current through water and into the skin’s surface. It is particularly effective for excessive sweating of the hands and feet. Regular sessions are required to maintain results, and some patients might experience mild skin irritation.
- Botox Injections: Botox (botulinum toxin) injections are another advanced treatment option. Botox works by blocking the nerves that trigger sweat glands, significantly reducing sweating in the treated areas. The effects can last for several months, but repeat treatments are necessary. Possible side effects include pain at the injection site and temporary muscle weakness.
By exploring these conventional treatments, individuals with hyperhidrosis can find relief and improve their quality of life. Always consult a healthcare provider to determine the best treatment plan for your specific condition.
Surgical Options and Innovative Therapies for Hyperhidrosis
Hyperhidrosis, characterized by excessive sweating, can significantly impact quality of life. While many treatments exist, surgical options and emerging therapies are providing new hope for those seeking relief. Below, we explore the most common surgical procedures, innovative therapies, and the benefits and risks associated with these treatments.
Surgical Procedures for Hyperhidrosis
1. Sympathectomy:
- Explanation: Sympathectomy involves cutting or clamping the sympathetic nerves responsible for triggering excessive sweating. This procedure is typically performed using minimally invasive techniques, such as endoscopic thoracic sympathectomy (ETS).
- Benefits: It can provide permanent relief from excessive sweating, particularly in the hands and underarms.
- Risks: Potential side effects include compensatory sweating (increased sweating in other body areas), nerve damage, and, in rare cases, Horner’s syndrome (drooping eyelid and constricted pupil).
2. Local Sweat Gland Removal:
- Explanation: This involves the surgical removal of sweat glands from affected areas like the underarms. Techniques include curettage (scraping), liposuction, or excision.
- Benefits: Effective in significantly reducing sweat production in targeted areas.
- Risks: Scarring, infection, and changes in skin sensation are possible complications.
Emerging Therapies and Research on Hyperhidrosis Treatment
1. Botox Injections:
- Explanation: Botulinum toxin injections temporarily block the nerves that cause sweating. It’s particularly effective for underarm hyperhidrosis.
- Benefits: Minimally invasive with quick results.
- Risks: Temporary muscle weakness and the need for repeated treatments every few months.
2. MiraDry:
- Explanation: This non-invasive procedure uses microwave energy to destroy sweat glands in the underarms.
- Benefits: Permanent reduction in sweat production with minimal downtime.
- Risks: Potential for swelling, pain, and changes in skin sensation.
3. Iontophoresis:
- Explanation: This technique involves using a mild electrical current to temporarily block sweat glands, typically used for hands and feet.
- Benefits: Non-invasive and can be performed at home with the appropriate device.
- Risks: Skin irritation and discomfort during treatment sessions.
Benefits and Risks of Surgical Versus Non-Surgical Treatments
Surgical Treatments:
- Benefits: Often provide long-term or permanent relief from excessive sweating. They are highly effective for severe cases of hyperhidrosis.
- Risks: Involves higher risks such as infection, nerve damage, and compensatory sweating. Recovery time can be longer compared to non-surgical options.
Non-Surgical Treatments:
- Benefits: Typically involve less risk, minimal downtime, and are less invasive. Options like Botox and MiraDry offer quick relief with minimal side effects.
- Risks: Many non-surgical treatments require ongoing maintenance and repeated sessions. The results may not be as long-lasting as surgical options.
However, consulting with a healthcare professional can help determine the most suitable approach for managing this condition.
Lifestyle Modifications and Home Remedies for Hyperhidrosis
Managing hyperhidrosis at home involves practical steps to reduce symptoms and improve comfort. Here are some effective strategies:
Practical Tips for Managing Symptoms at Home
- Keep Cool: Stay in air-conditioned environments during hot weather and avoid hot, spicy foods that can trigger sweating.
- Regular Showers: Bathe frequently to keep skin clean and minimize bacteria that can cause odor.
- Use Antiperspirants: Apply antiperspirants at night for maximum effectiveness, as they need time to absorb and block sweat glands.
Importance of Lifestyle Choices
- Clothing: Opt for breathable, loose-fitting clothes made of natural fabrics like cotton. Dark colors can help conceal sweat stains.
- Diet: Avoid foods and beverages that can increase sweating, such as caffeine, alcohol, and spicy dishes. Incorporate a balanced diet rich in fruits and vegetables.
- Hydration: Drink plenty of water to help regulate body temperature and reduce overall sweating.
Home-Based Solutions and Over-the-Counter Products
- Antiperspirants: Over-the-counter antiperspirants with aluminum chloride are effective for mild hyperhidrosis.
- Absorbent Powders: Use talcum powder or cornstarch on sweat-prone areas to keep skin dry.
- Herbal Remedies: Sage tea and witch hazel are natural astringents that may help reduce sweating.
Implementing these lifestyle modifications and home remedies can significantly improve the management of hyperhidrosis, leading to a more comfortable and confident daily life.
The Role of Mental Health in Managing Hyperhidrosis
Hyperhidrosis, a condition characterized by excessive sweating, can have profound psychological impacts on those who suffer from it. Understanding and addressing the mental health aspects of hyperhidrosis is crucial for comprehensive management of the condition.
Discussing the Psychological Impact of Hyperhidrosis
Living with hyperhidrosis often leads to significant emotional distress. Many individuals experience heightened levels of anxiety and self-consciousness due to the constant worry about visible sweat marks and the potential for social embarrassment. This can lead to avoidance of social situations, a decrease in self-esteem, and feelings of isolation. Understanding these psychological impacts is the first step towards effective management.
Strategies for Coping with Anxiety and Social Stigma
Developing strategies to cope with the anxiety and social stigma associated with hyperhidrosis is essential. Cognitive-behavioral techniques, such as mindfulness and relaxation exercises, can help manage anxiety levels. Building a support network of understanding friends and family members can also provide emotional relief. Additionally, wearing breathable clothing and using antiperspirants specifically designed for hyperhidrosis can reduce physical symptoms and boost confidence in social situations.
Professional Help from Mental Health Experts
Seeking professional help from mental health experts can be highly beneficial for those struggling with the psychological effects of hyperhidrosis. Therapists can provide tailored strategies to manage anxiety and depression, helping individuals to develop a healthier mindset. Support groups, whether in-person or online, can offer a sense of community and shared understanding, making it easier to cope with the condition.
However, addressing the mental health aspects of hyperhidrosis is vital for overall well-being. By recognizing the psychological impact, adopting effective coping strategies, and seeking professional support, individuals can better manage their condition and improve their quality of life.
FAQs about Hyperhidrosis Treatment
What is Hyperhidrosis?
Hyperhidrosis is a condition characterized by excessive sweating that affects daily activities. It can occur in specific areas like the underarms, hands, feet, or face, and sometimes across the entire body.
What Causes Hyperhidrosis?
The exact cause of hyperhidrosis is not fully understood. It can be primary (idiopathic) with no identifiable cause, often running in families, or secondary due to underlying medical conditions like thyroid problems, diabetes, or menopause.
What are the Treatment Options?
- Topical Treatments: Antiperspirants with aluminum chloride are often the first line of treatment.
- Medications: Prescription medications can help reduce sweating.
- Botox Injections: Botox can block the nerves that cause sweating.
- Iontophoresis: A procedure that uses electrical currents to reduce sweating, especially in the hands and feet.
- Surgery: In severe cases, surgical options like sympathectomy may be considered.
Are These Treatments Effective?
Yes, many treatments for hyperhidrosis are effective. The success rate varies depending on the treatment method and the individual. For example, Botox injections have a high success rate for underarm sweating, while iontophoresis is particularly effective for sweaty hands and feet.
Are There Any Side Effects?
Most treatments are safe but can have side effects. Topical treatments may cause skin irritation. Medications can cause dry mouth and blurred vision. Botox injections may cause temporary muscle weakness. It’s important to discuss potential side effects with your doctor.
How Do I Know Which Treatment is Right for Me?
Consult with a healthcare professional to determine the best treatment plan for your specific condition. They can evaluate your symptoms, medical history, and lifestyle to recommend the most effective and appropriate treatment options.
Conclusion
In summary, we’ve explored the key aspects of hyperhidrosis, including its causes, symptoms, and various treatment options. From lifestyle changes to medical interventions like antiperspirants, medications, and surgical procedures, there are numerous ways to manage excessive sweating effectively.
It’s crucial to consult healthcare professionals to determine the most suitable treatment plan tailored to your individual needs. With ongoing advancements in medical science, the future looks promising for those dealing with hyperhidrosis, offering new hope and improved quality of life.
References
For those seeking more information or further validation of the data provided on hyperhidrosis treatments, the following sources are highly recommended:
- Mayo Clinic – Offers a comprehensive overview of hyperhidrosis, including symptoms, causes, and treatment options. Access detailed content from medical experts here.
- WebMD – Provides valuable insights into the diagnosis and management of hyperhidrosis. Learn more about innovative treatment methods and patient care advice here.
- International Hyperhidrosis Society – As a leading authority on sweat-related conditions, this organization offers in-depth research, patient stories, and treatment resources. Explore their extensive library of articles and resources here.
- PubMed Central – An invaluable resource for accessing peer-reviewed scientific studies and clinical trials on hyperhidrosis. Check out the latest research here.
These sources are maintained by reputable institutions or organizations, ensuring that the information is both accurate and up-to-date, aiding individuals in making well-informed decisions about their health care.